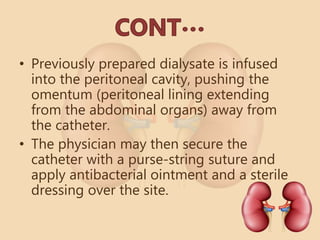
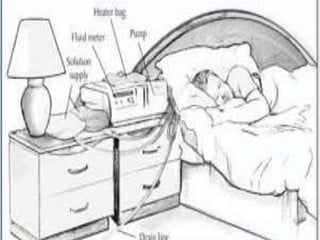
Dialysis is a clinical technique that involves the movement of fluid and solutes across a semi-permeable membrane to remove toxic substances and maintain fluid balance in patients with severe kidney disease. Peritoneal dialysis (PD) uses the patient's peritoneal membrane as a filter and includes procedures like inflow, dwell, and drain phases, which can be performed manually or with an automated cycler. Complications of PD may include infections, hernias, and nutritional deficiencies, and effective management is crucial for patient outcomes.