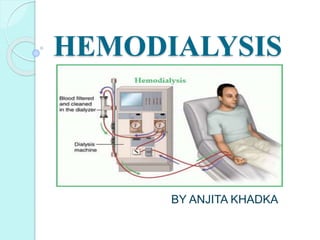
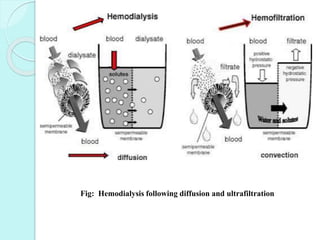
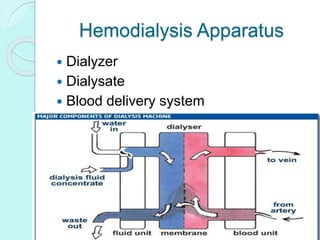
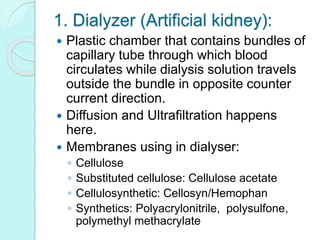
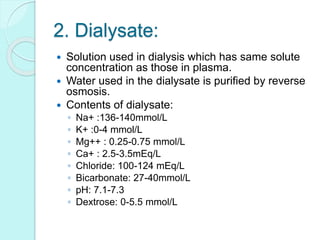
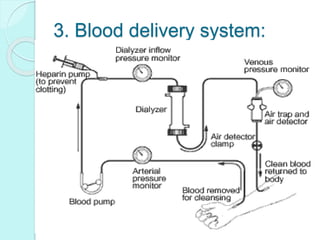
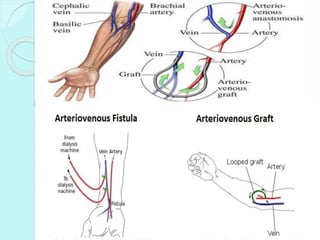
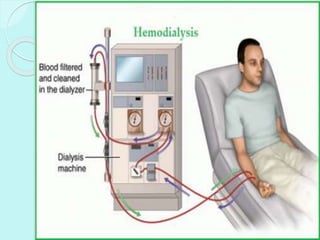
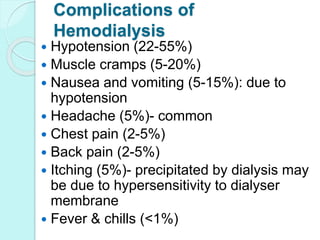
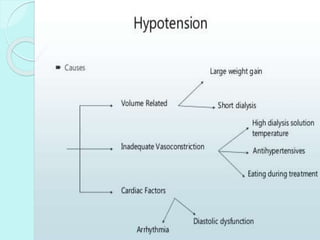
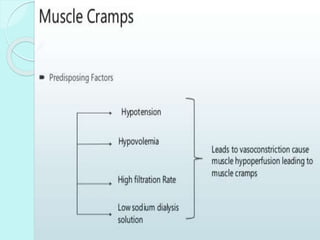
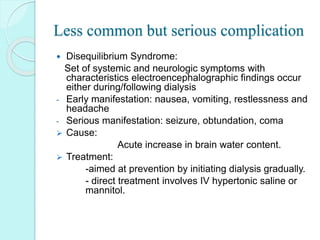
Hemodialysis is a medical procedure that removes waste and excess fluid from the blood of patients with kidney failure. It uses a hemodialysis machine and an artificial kidney called a dialyzer to filter the blood outside of the body. Blood flows through the dialyzer where diffusion and ultrafiltration remove waste and regulate electrolytes, and is then returned to the patient. Hemodialysis is usually done three times a week for four hours each session through an arteriovenous fistula, graft, or catheter. Potential complications include hypotension, muscle cramps, nausea, and disequilibrium syndrome.