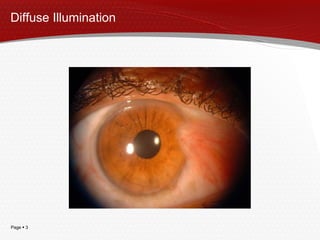
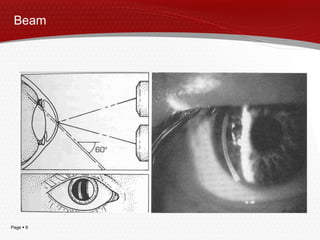
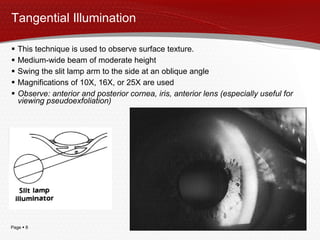
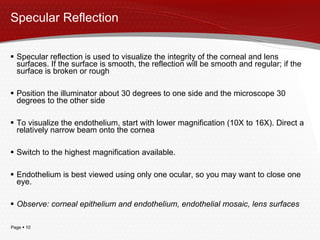
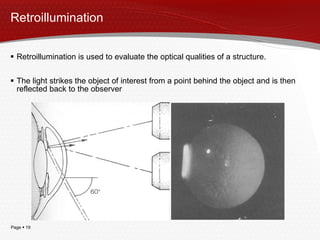
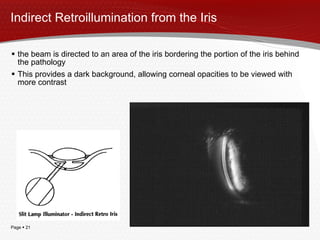
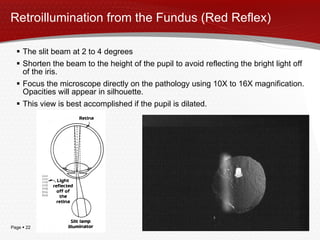
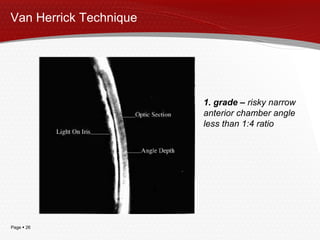
This document describes various illumination techniques used with a slit lamp to examine different parts of the eye. It discusses diffuse, direct, tangential, and specular illumination techniques as well as indirect, retroillumination, and Van Herrick techniques. Each technique is used to illuminate a specific area of the eye in order to observe different structures like the cornea, iris, lens, anterior chamber angle, and detect any pathologies present. Proper illumination angles and magnifications are outlined for visualizing various eye tissues and evaluating properties like surface texture and integrity.
![Slit Lamp Illumination Techniques Author: Irina Jagiloviča e-mail: [email_address] www: www.optometristiem.lv](https://image.slidesharecdn.com/slitlampilluminationtechniques-091129061239-phpapp02/85/Slit-Lamp-Illumination-Techniques-1-320.jpg)