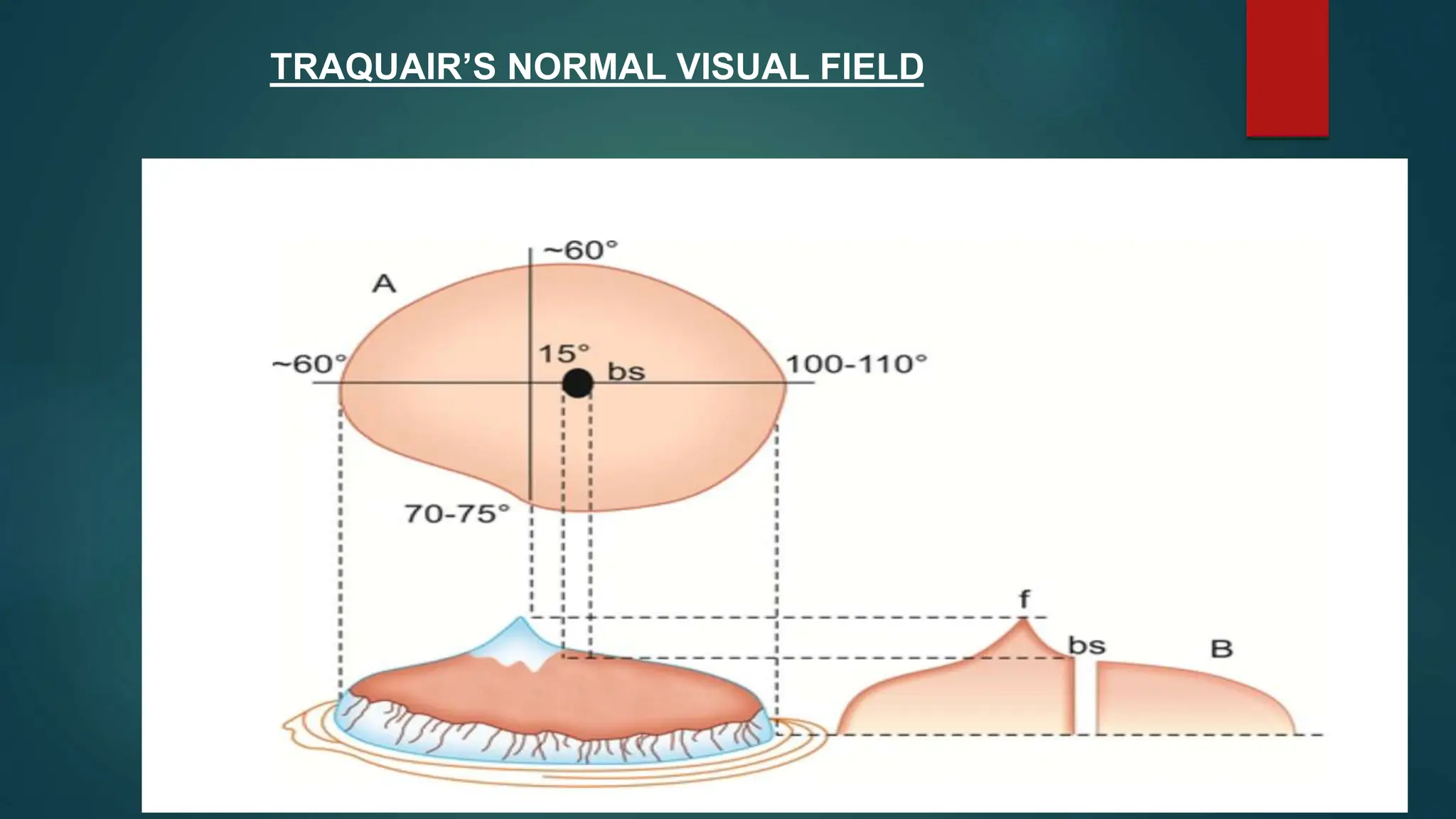
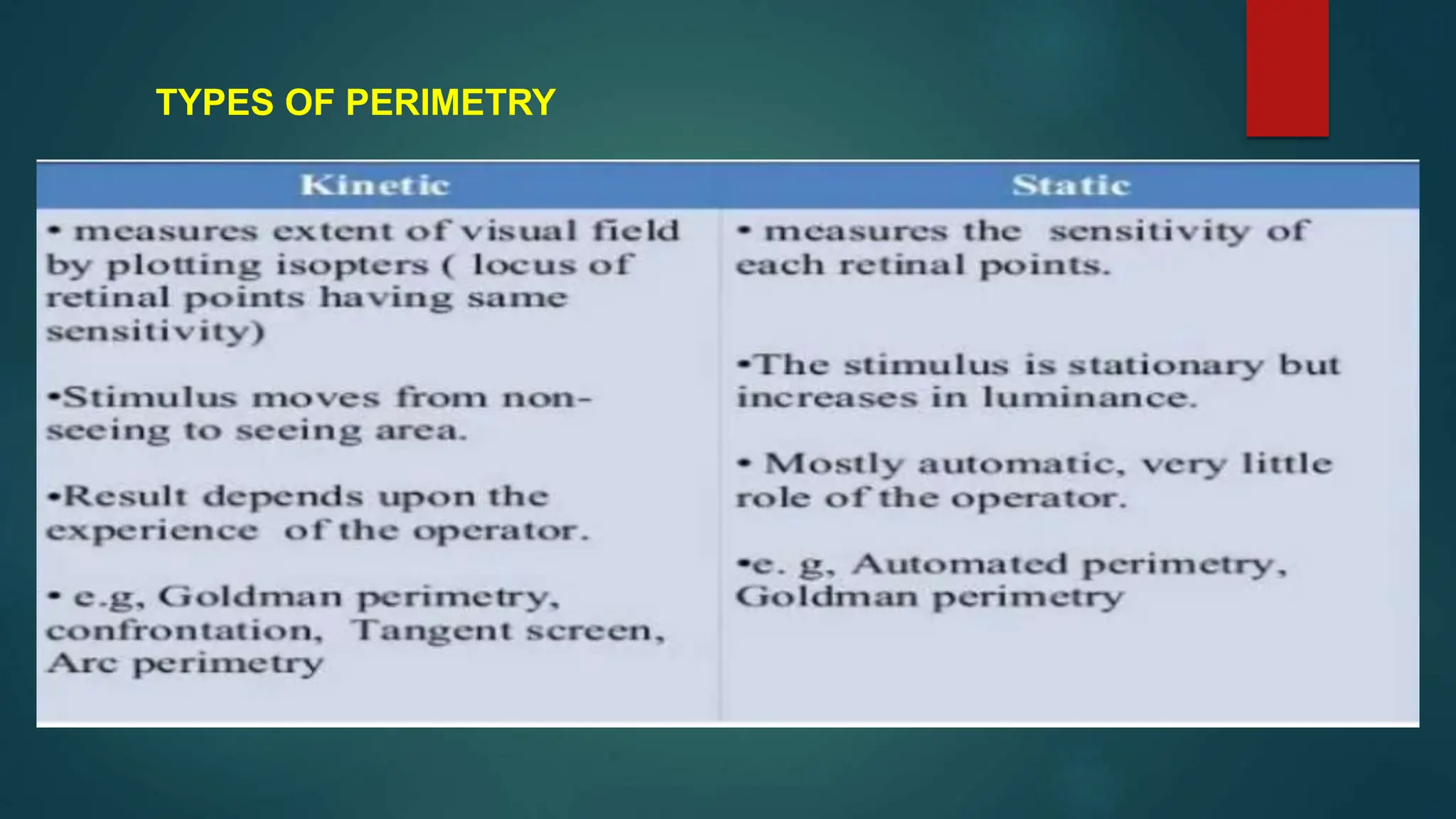
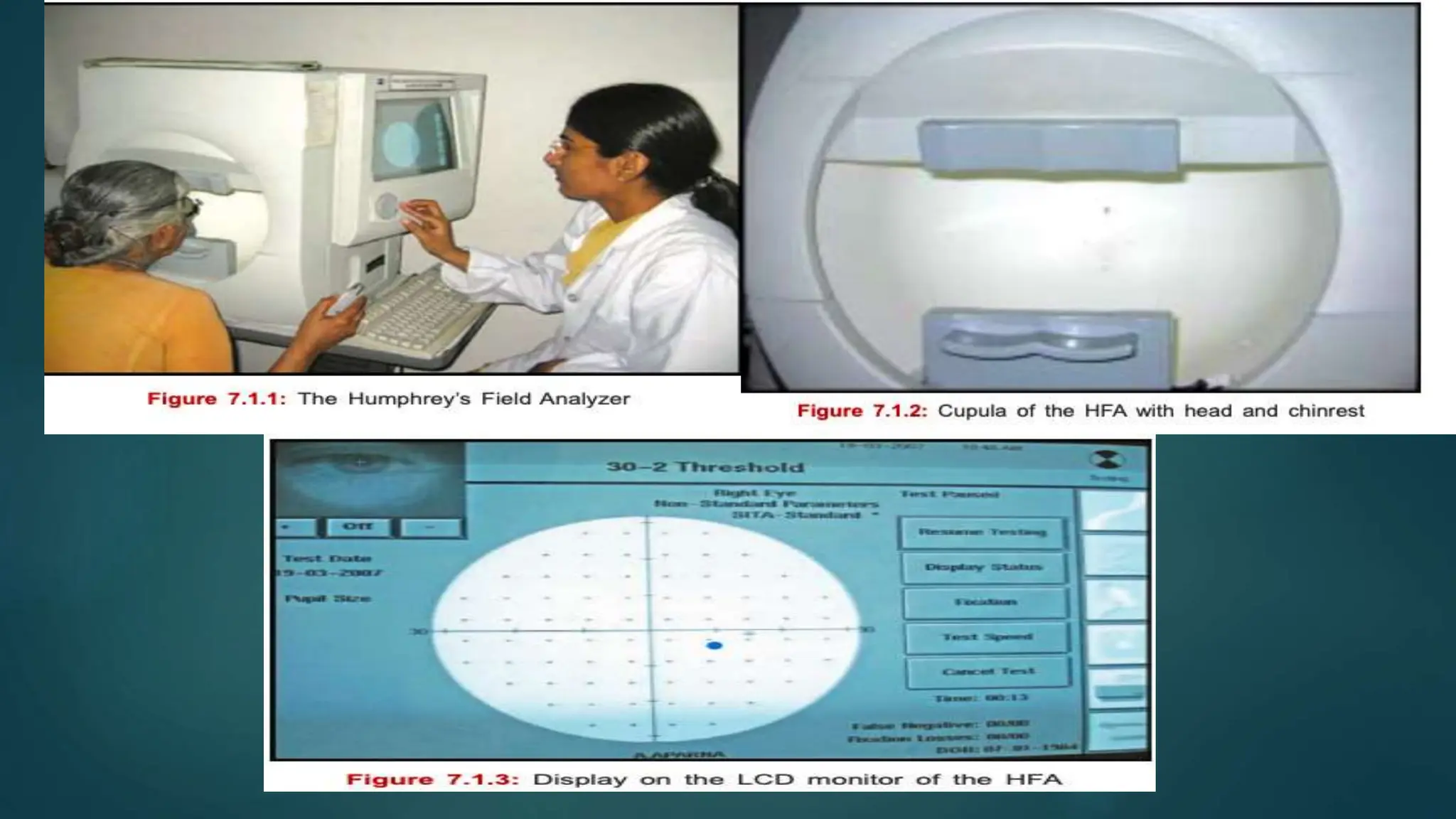
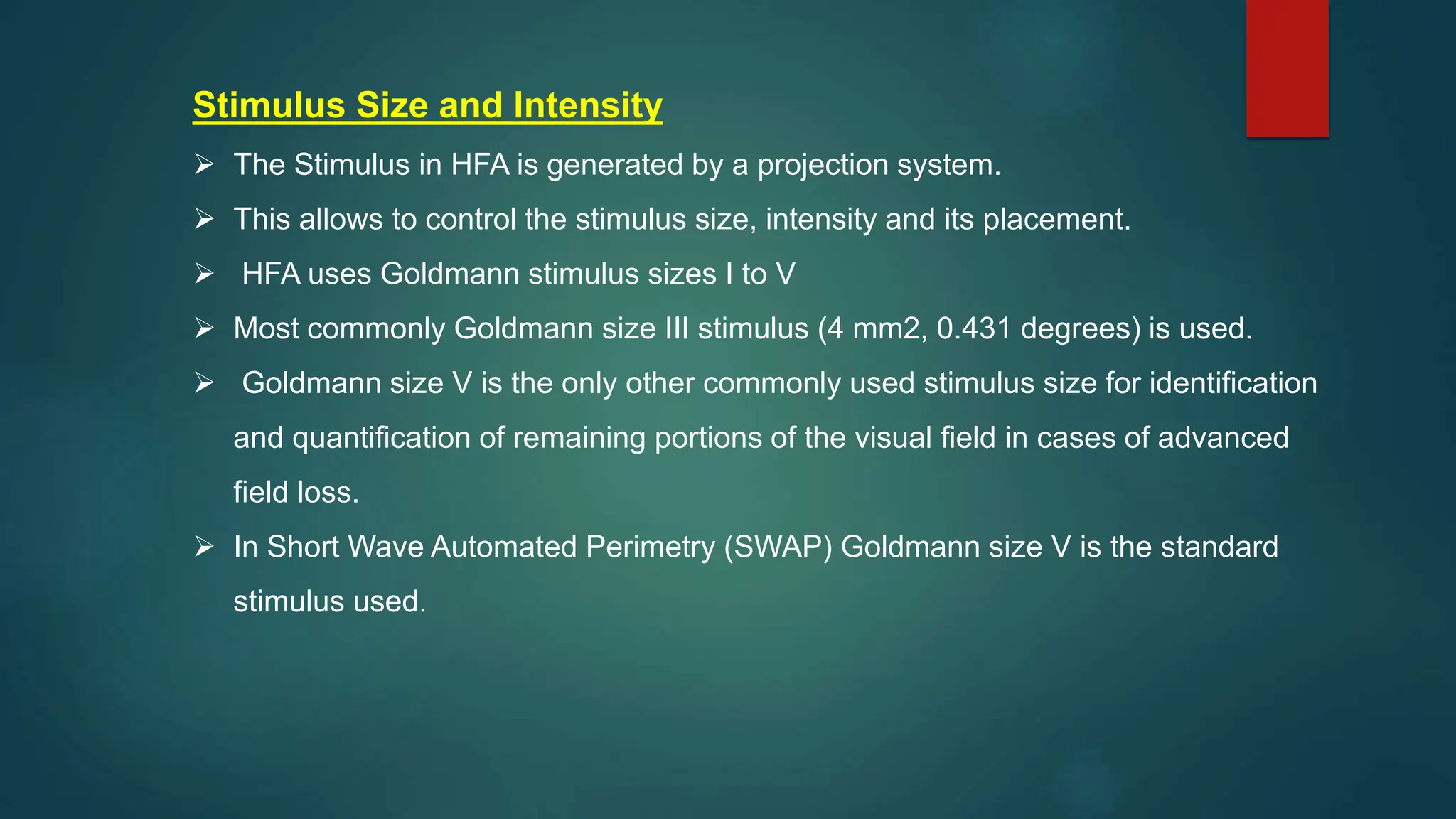
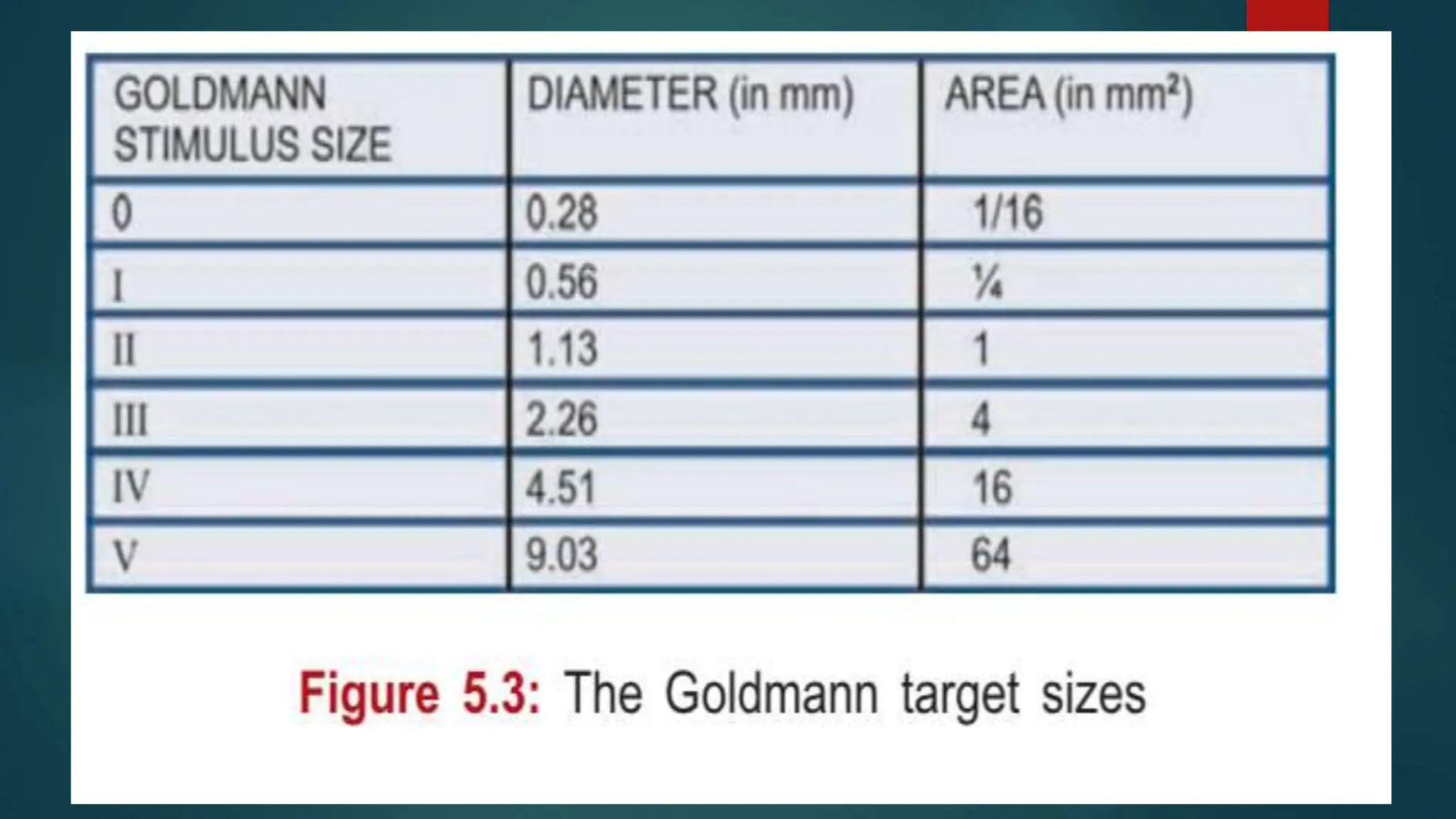
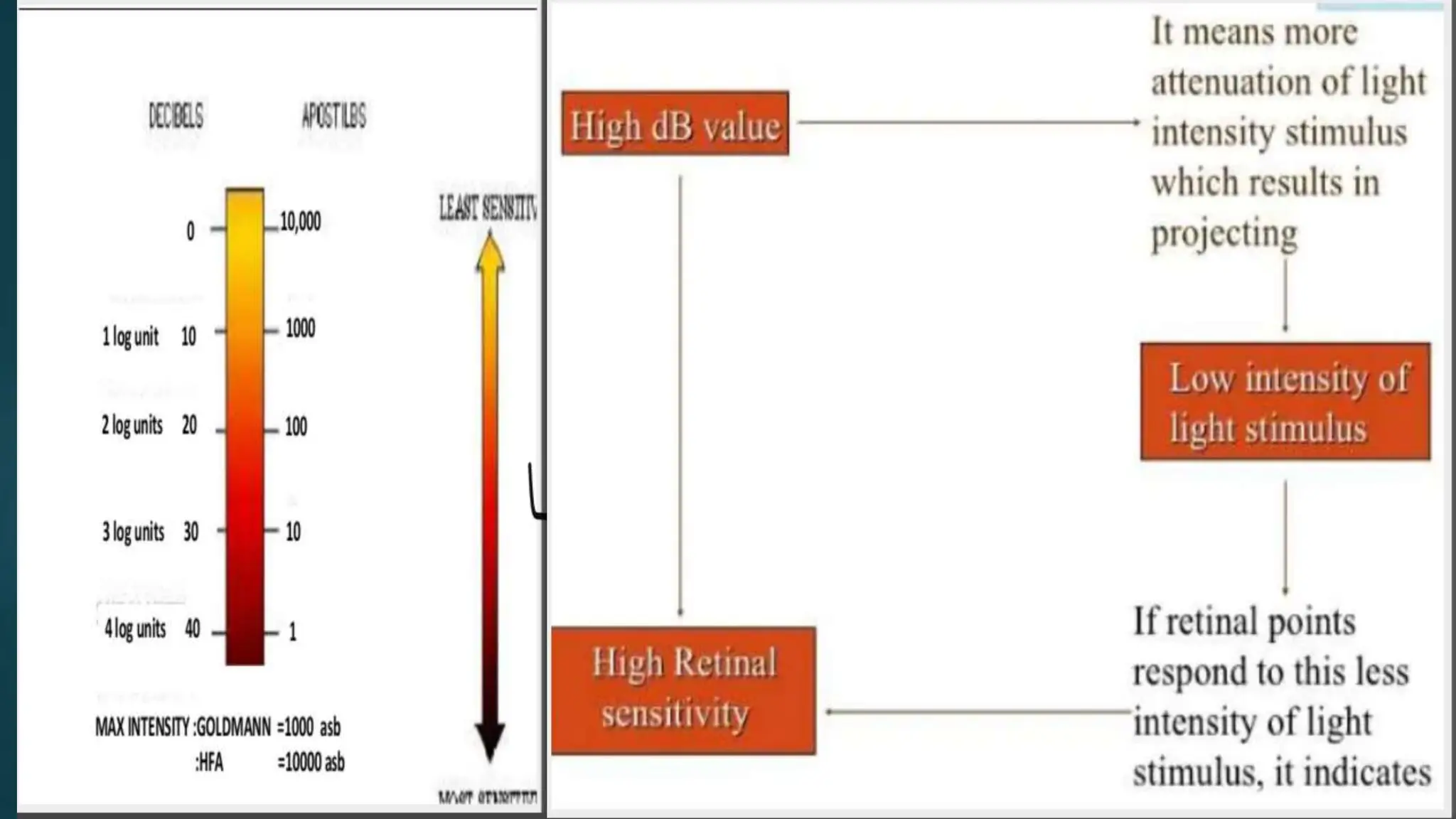
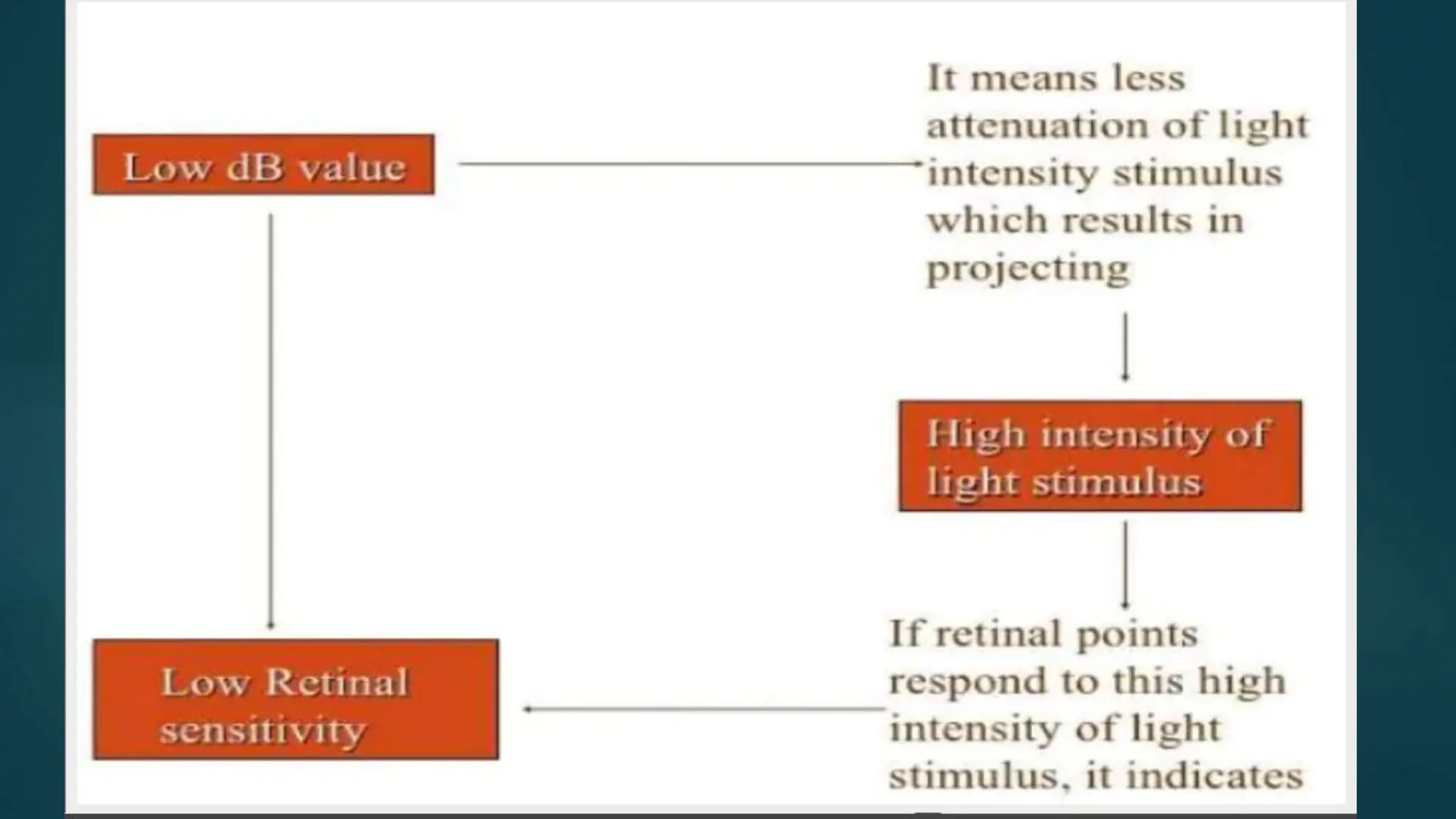
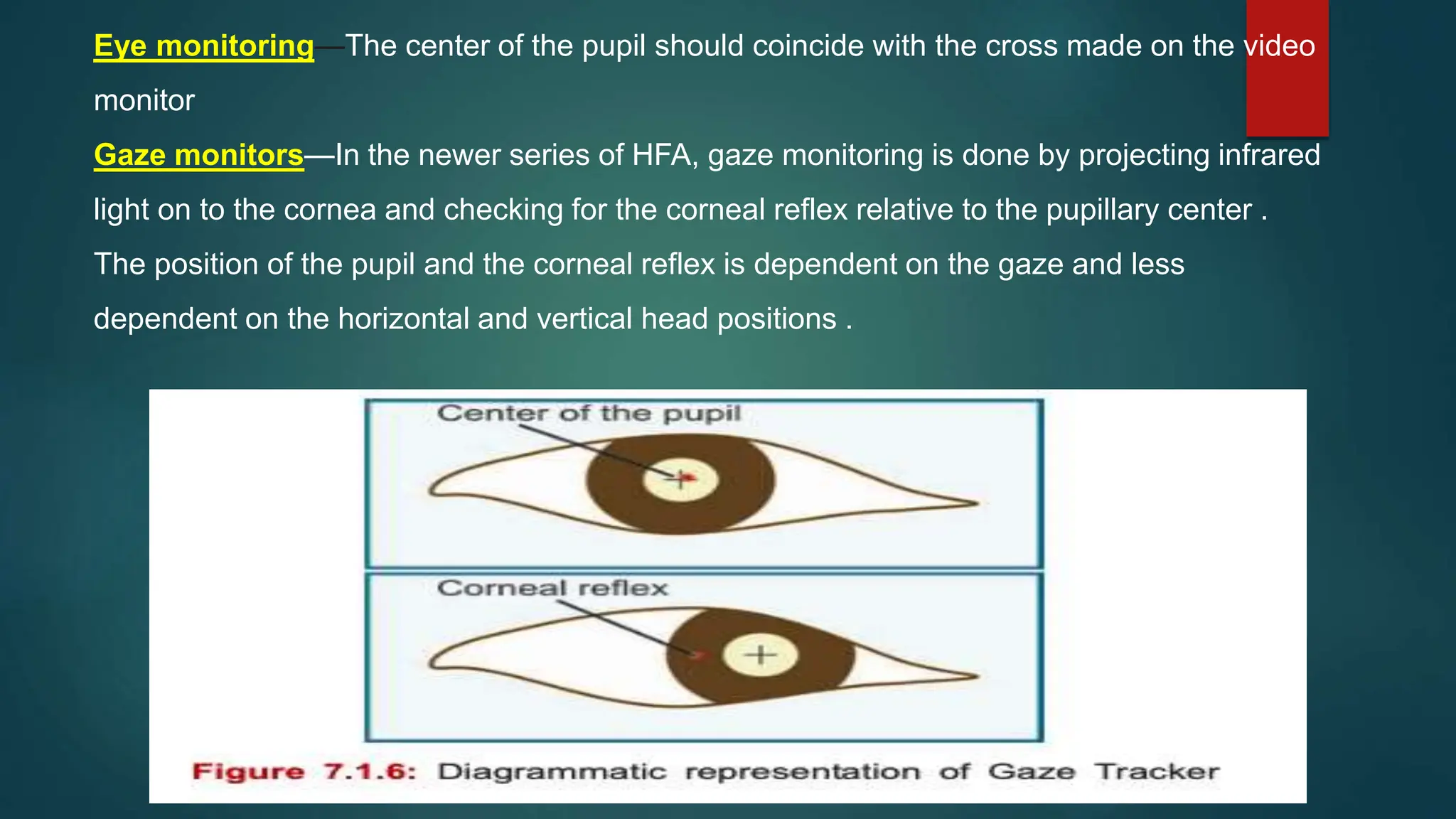
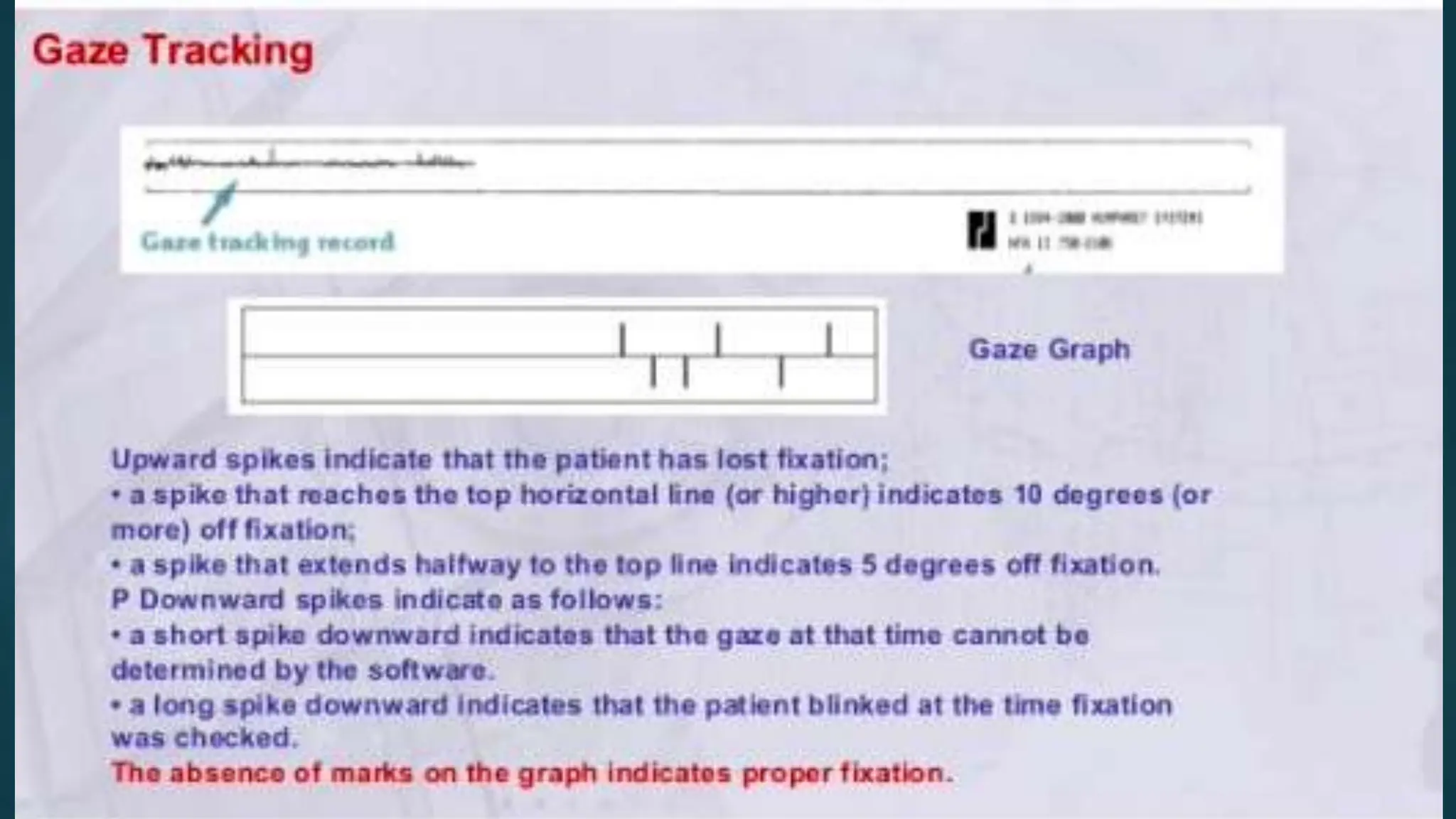
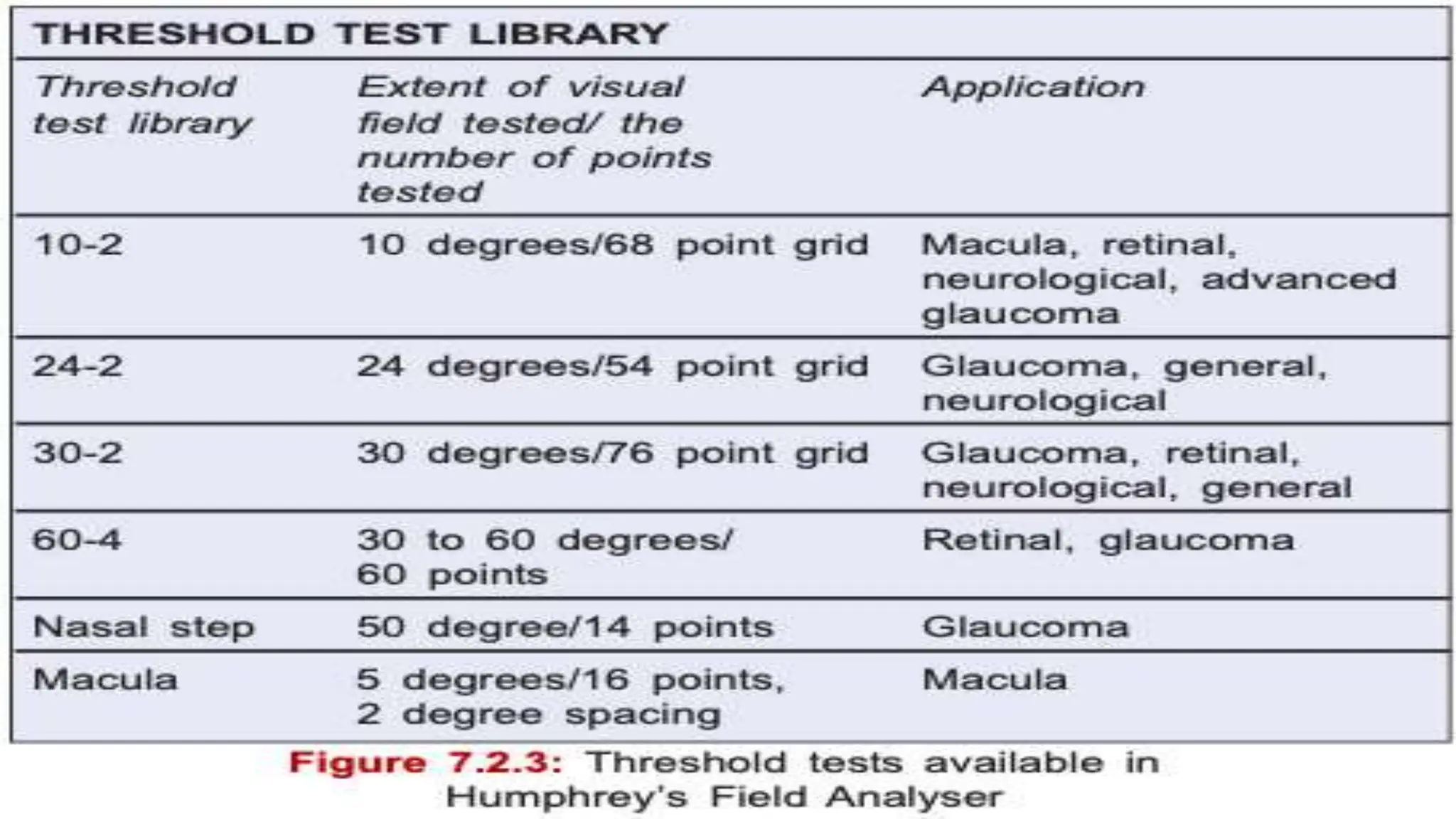
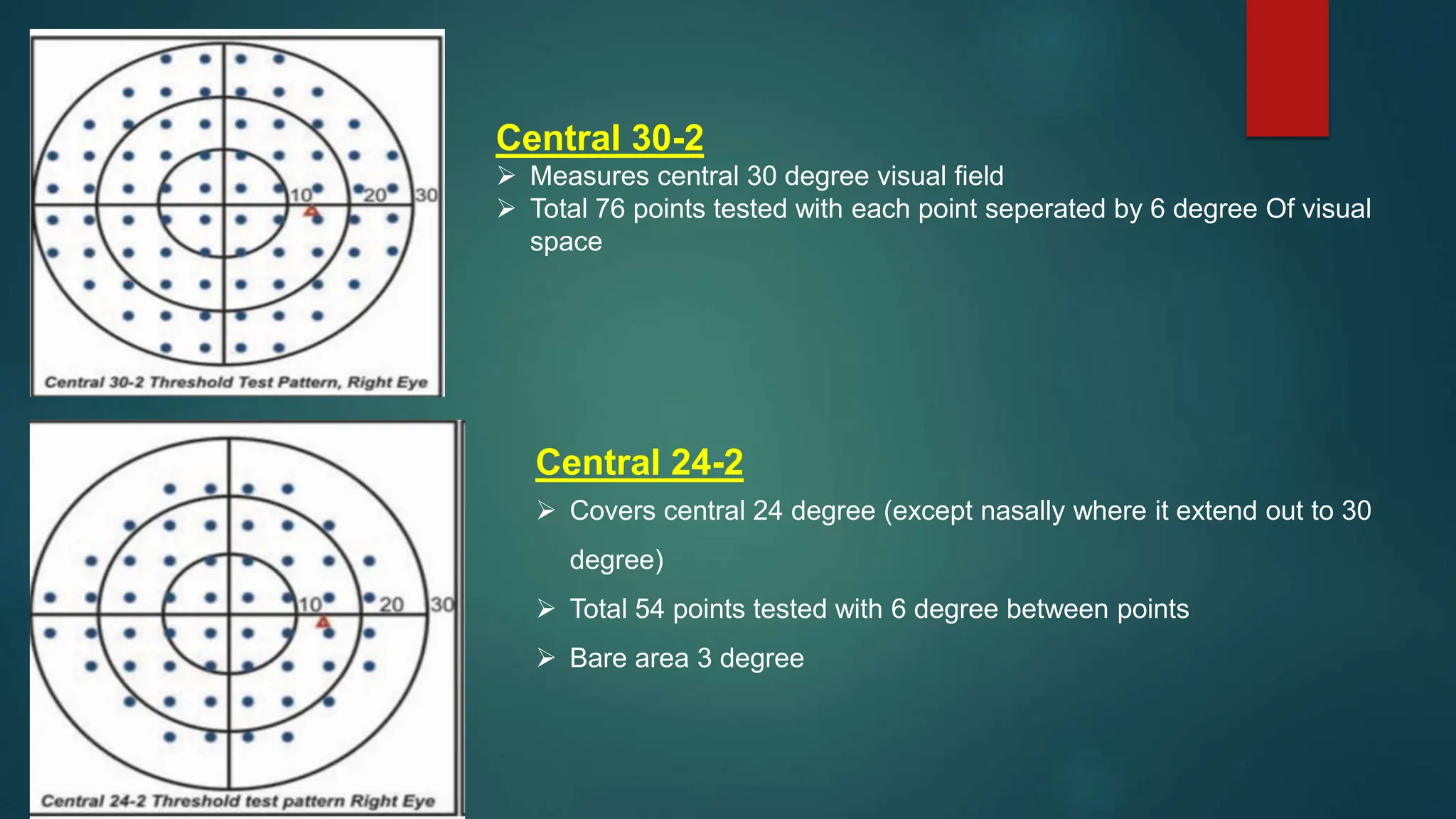
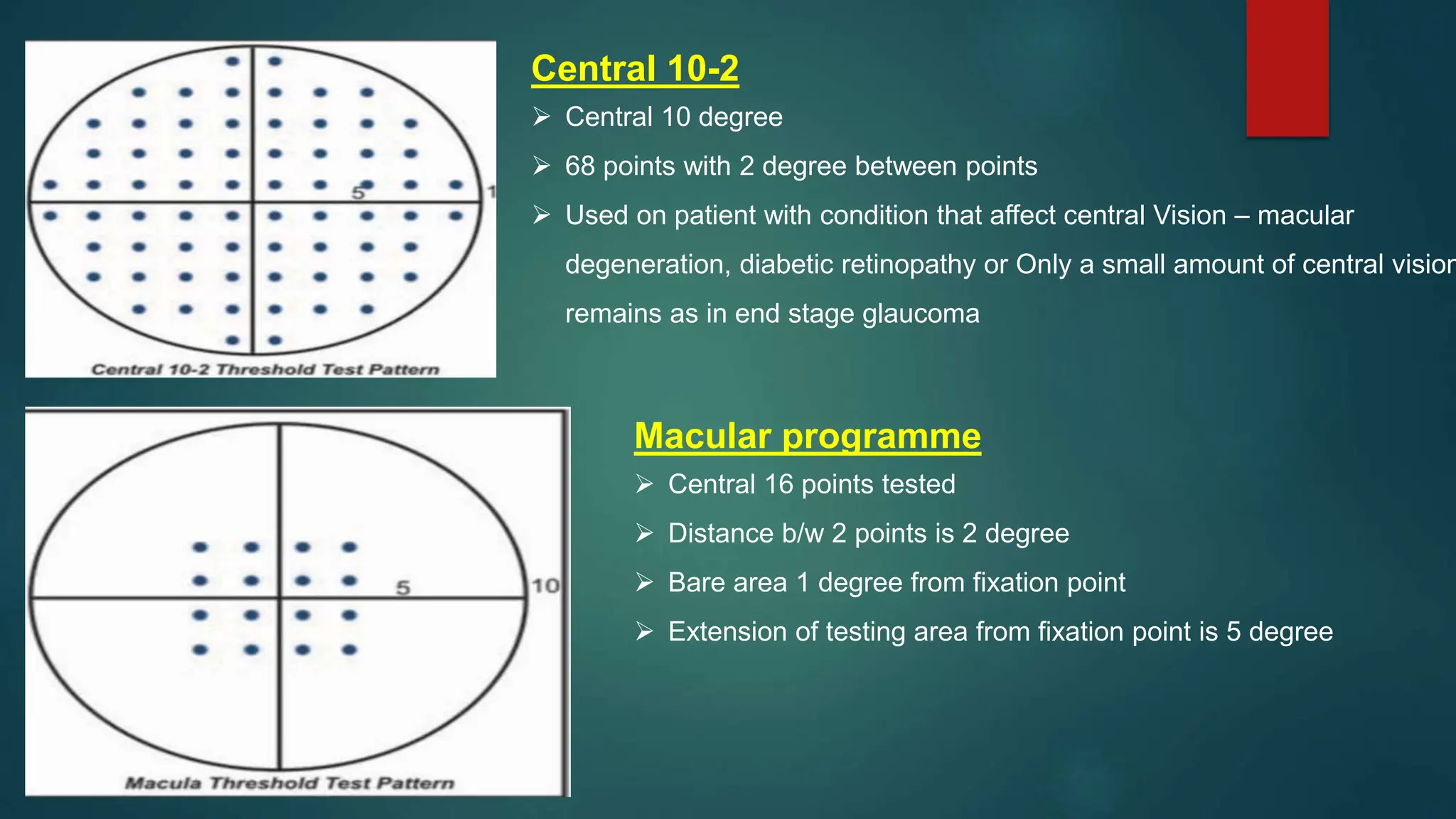
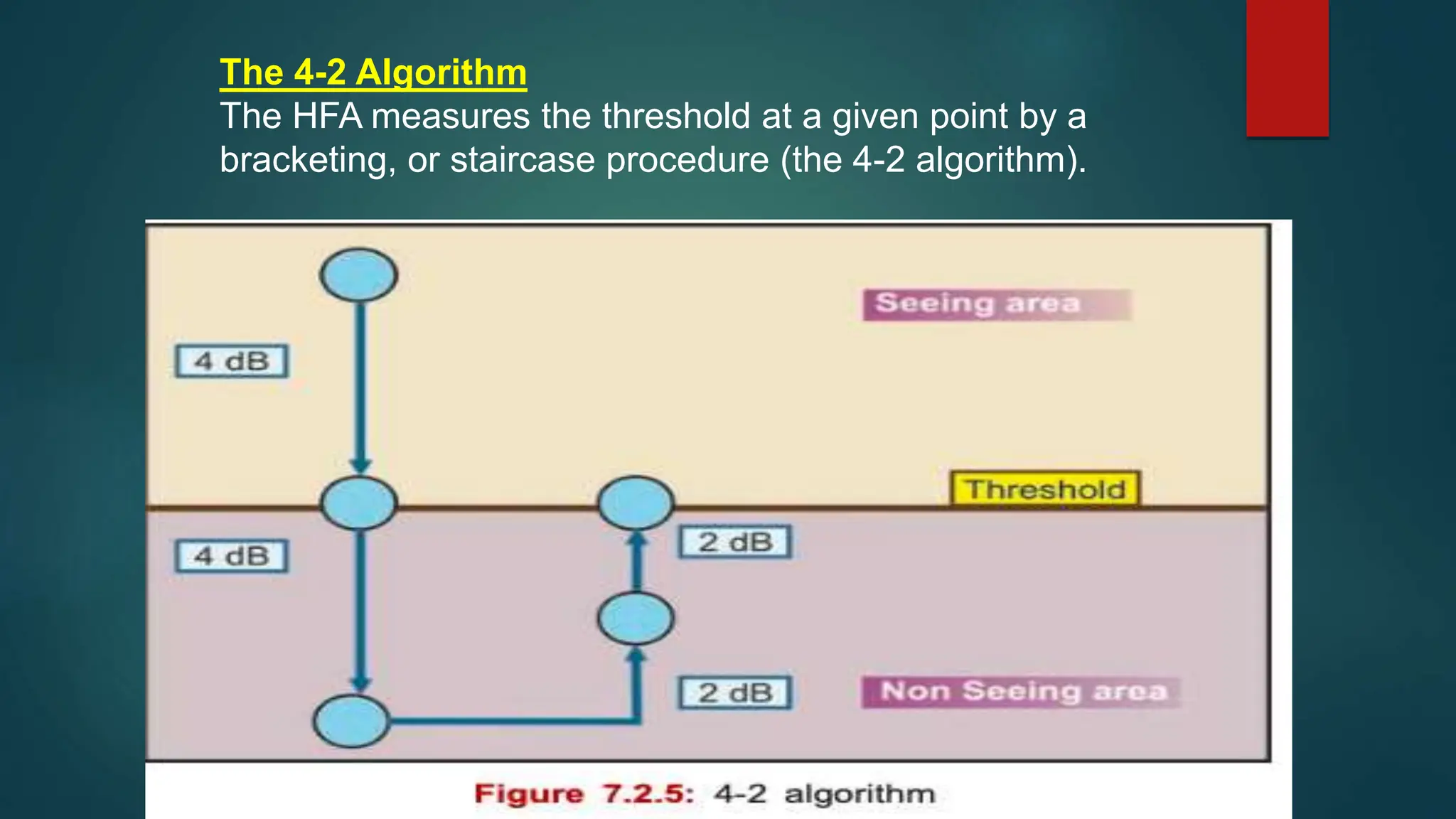
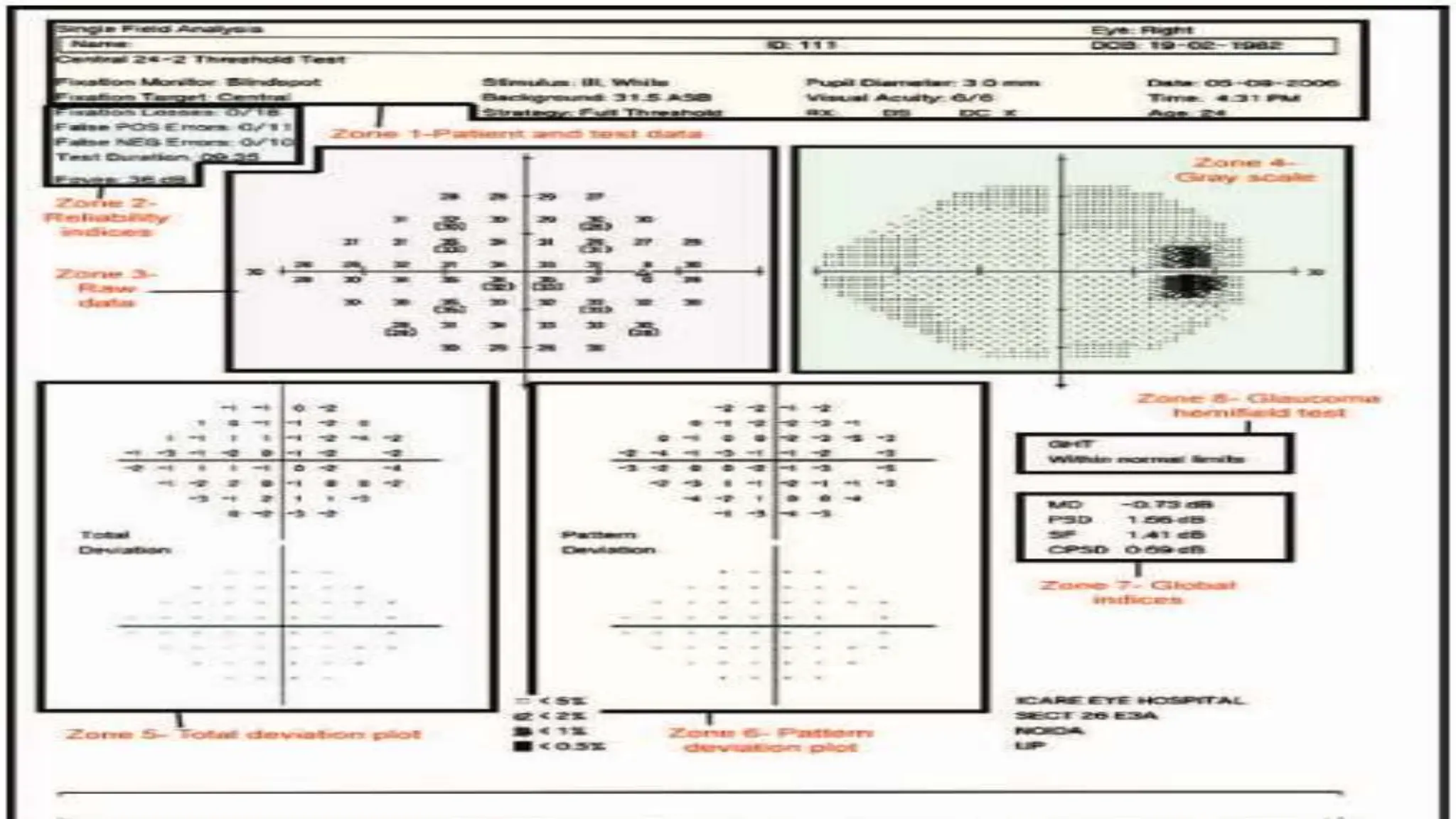
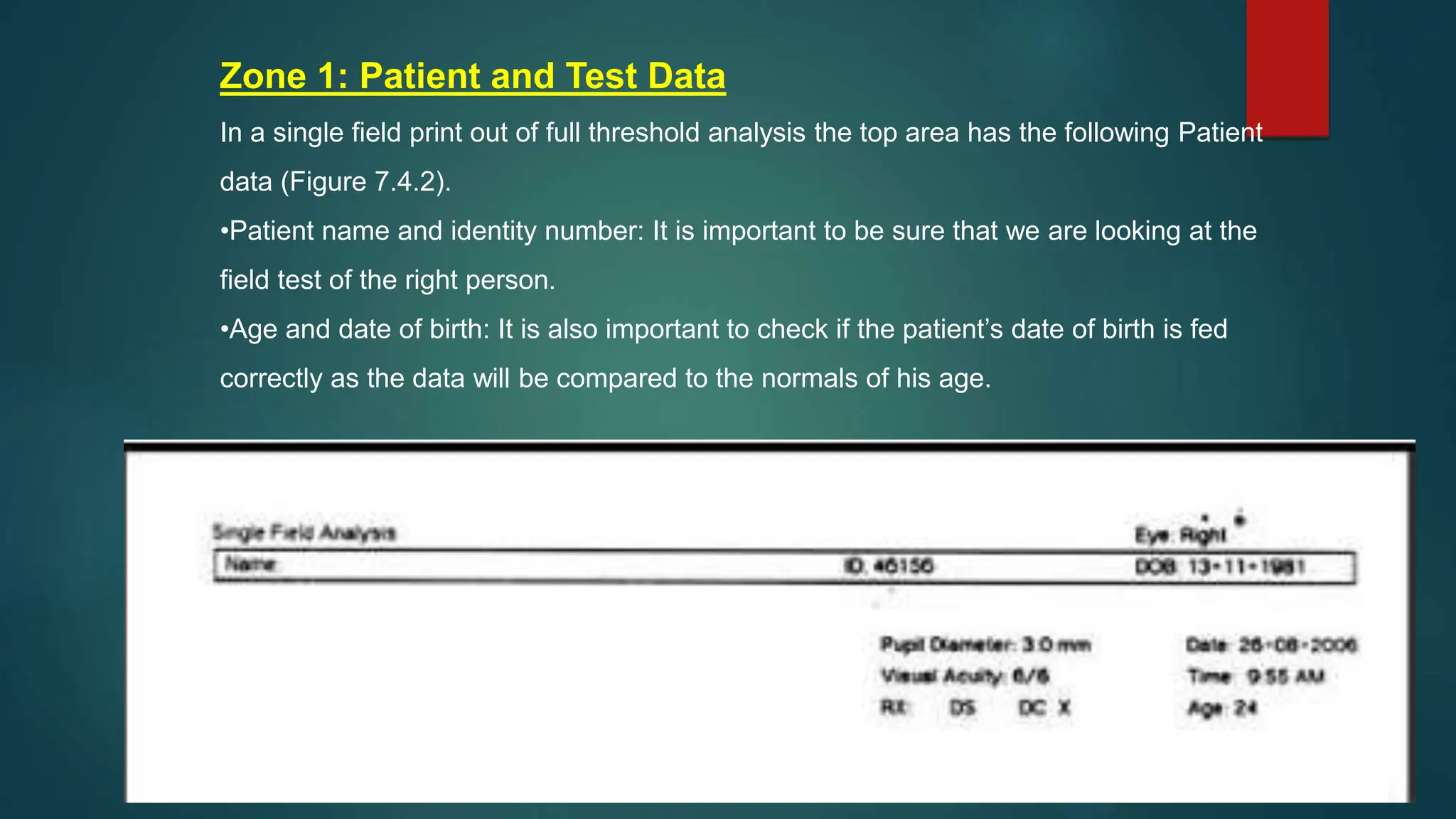
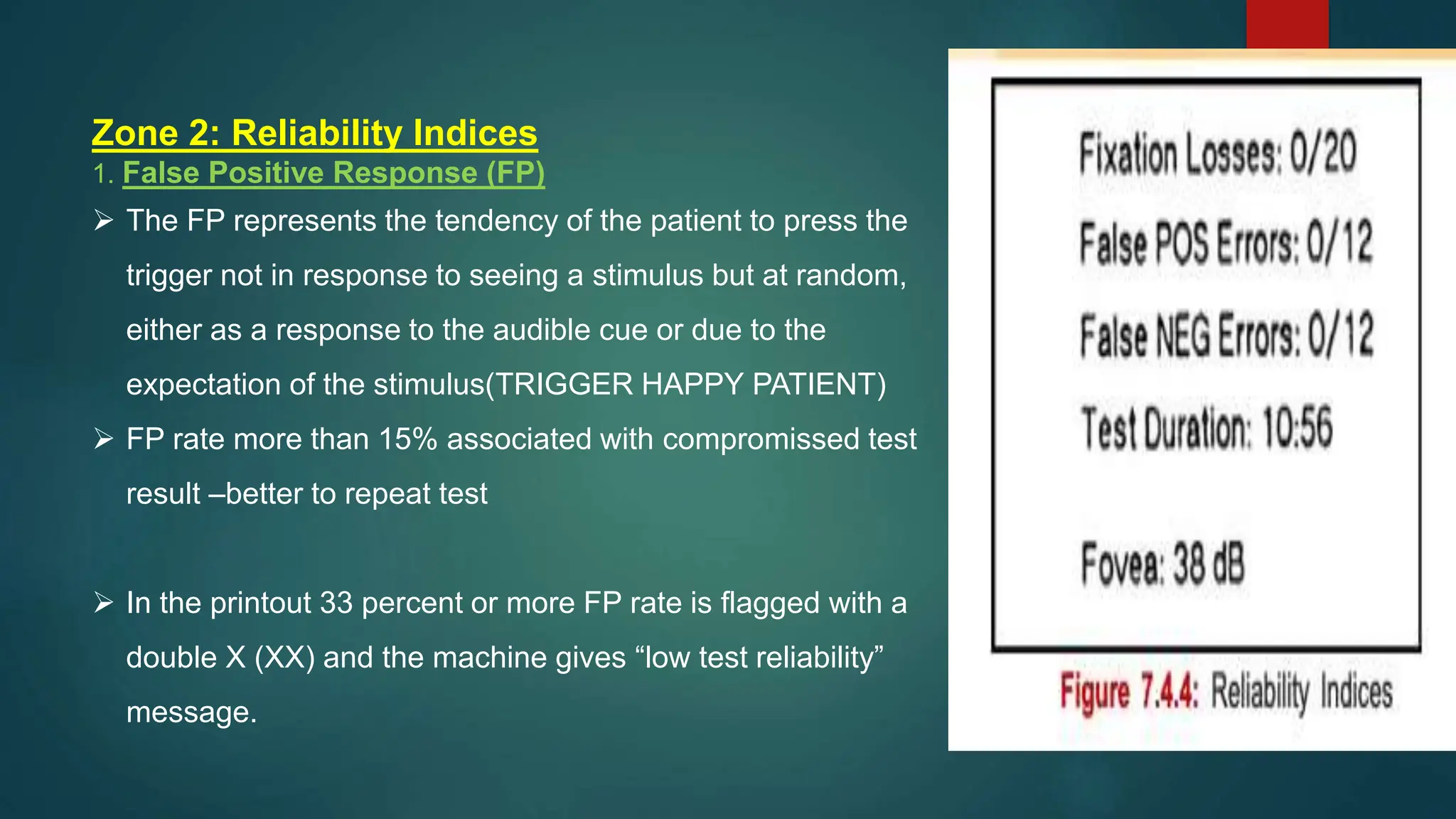
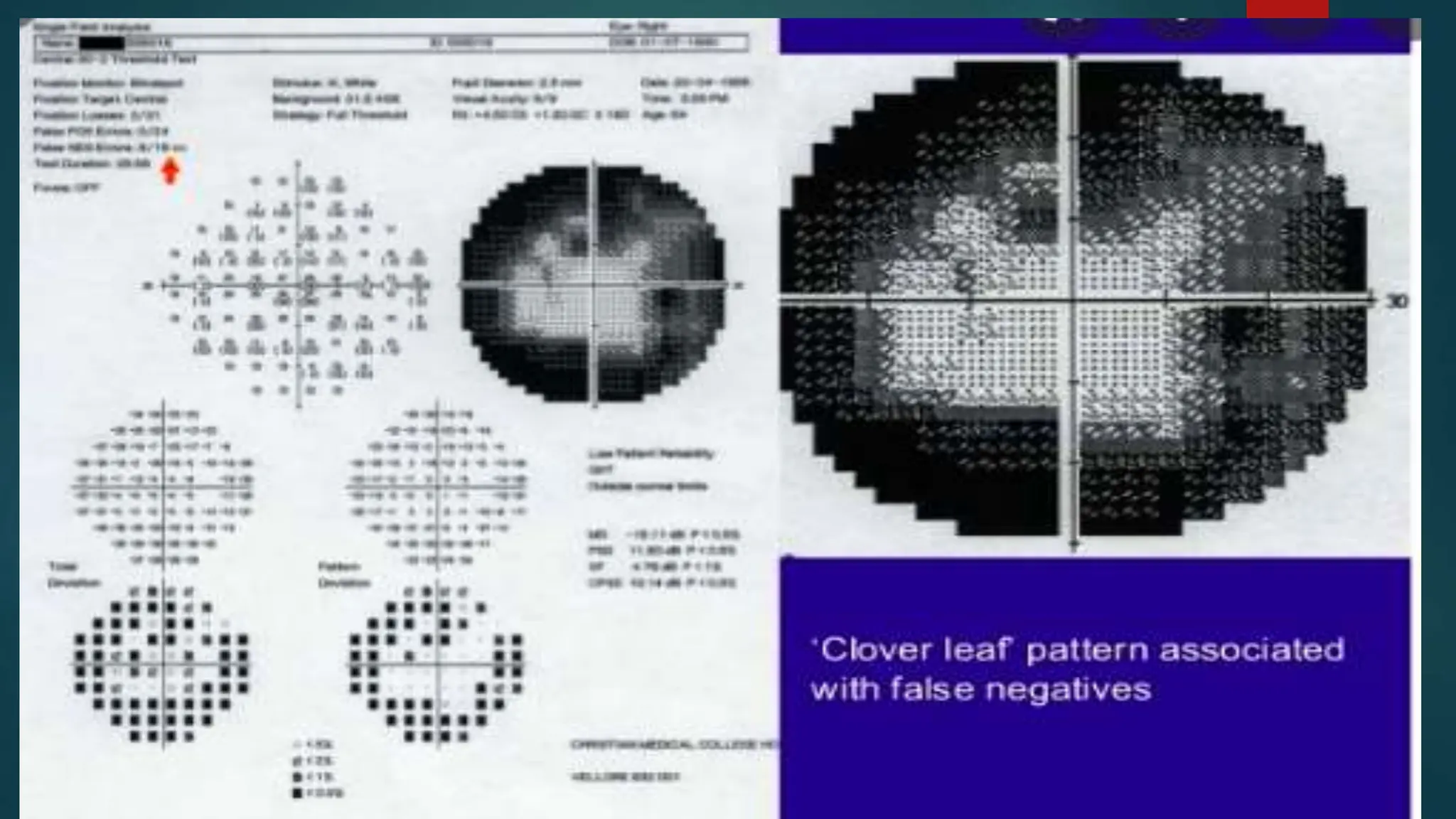
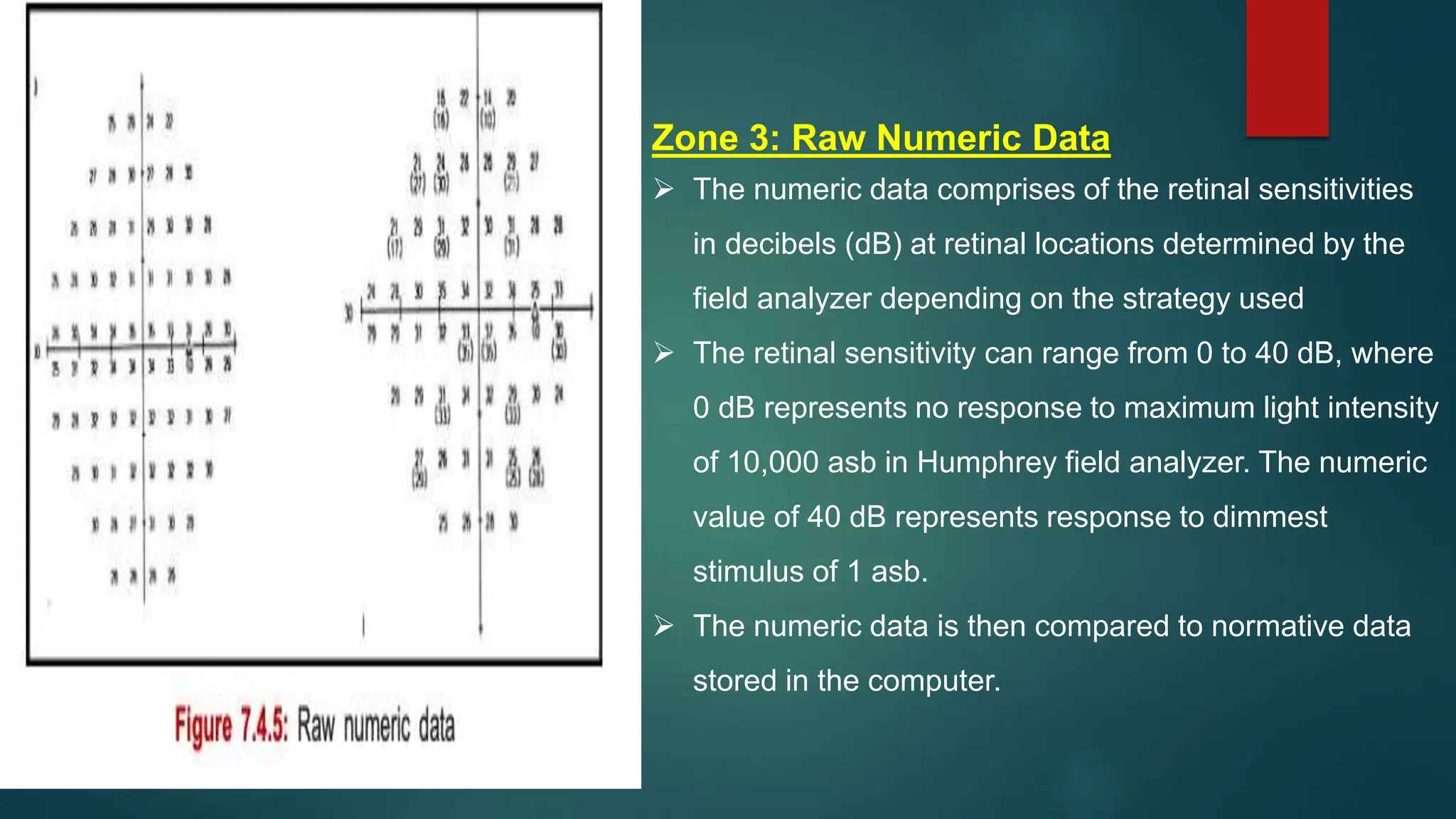
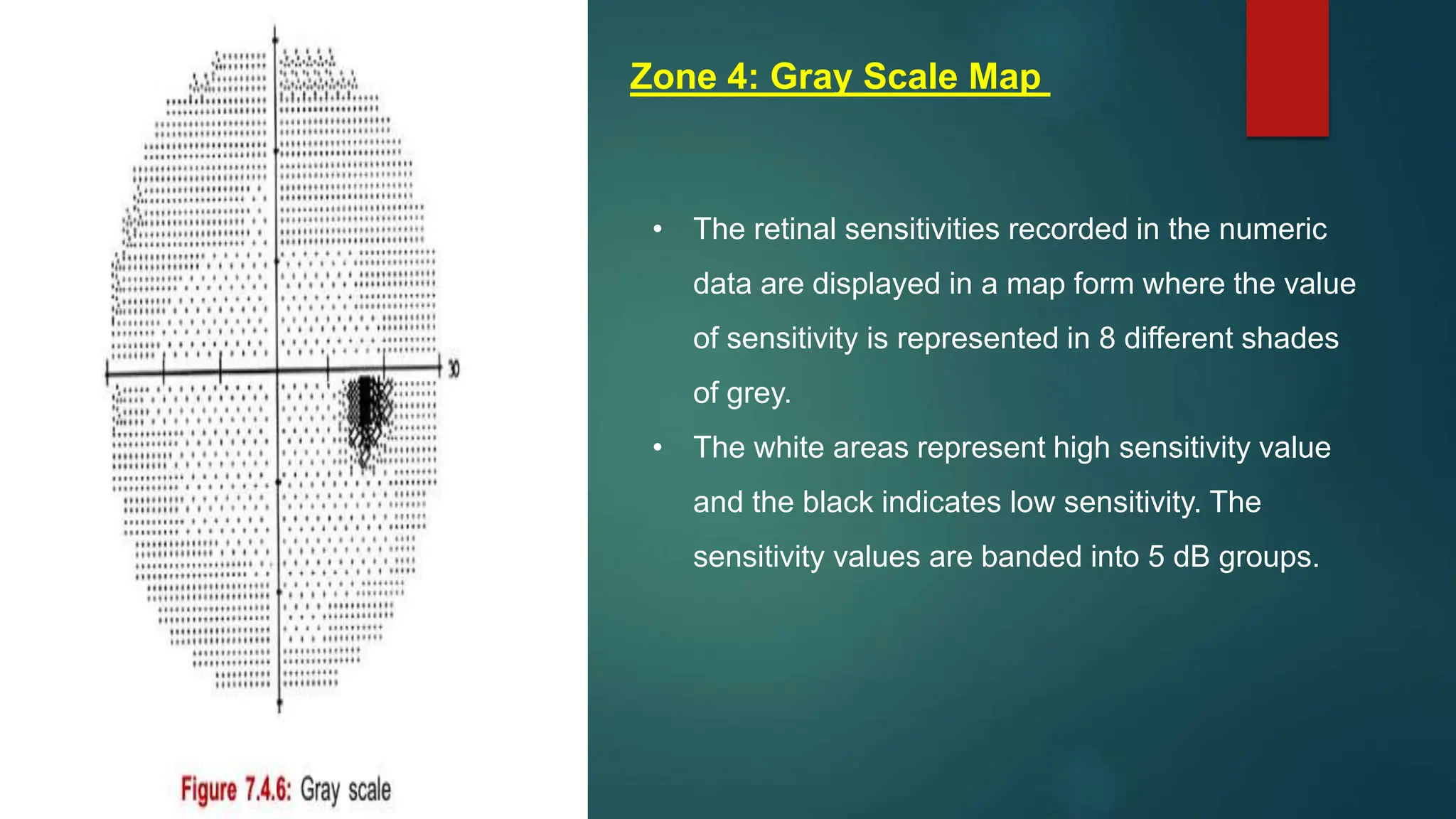
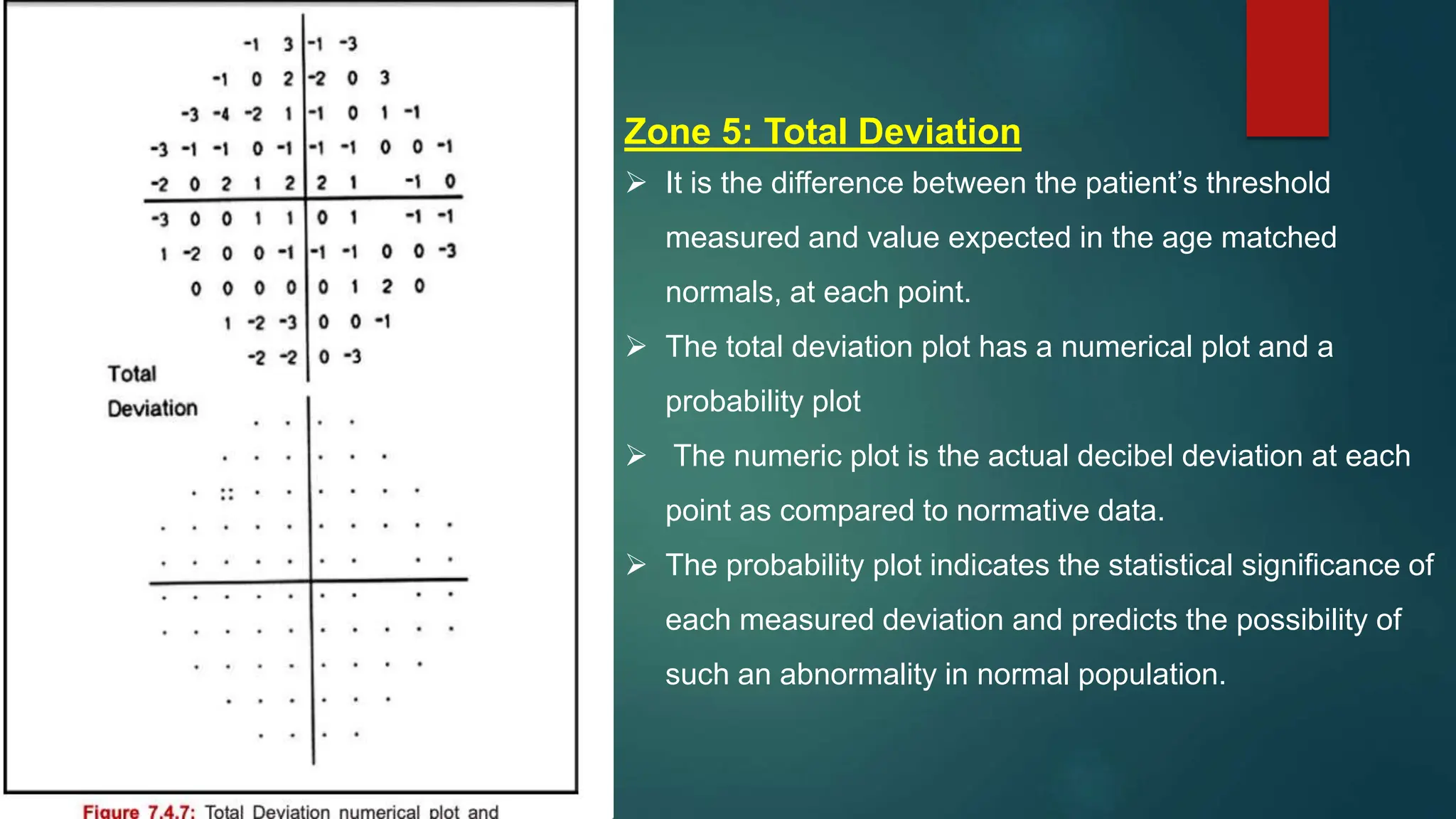
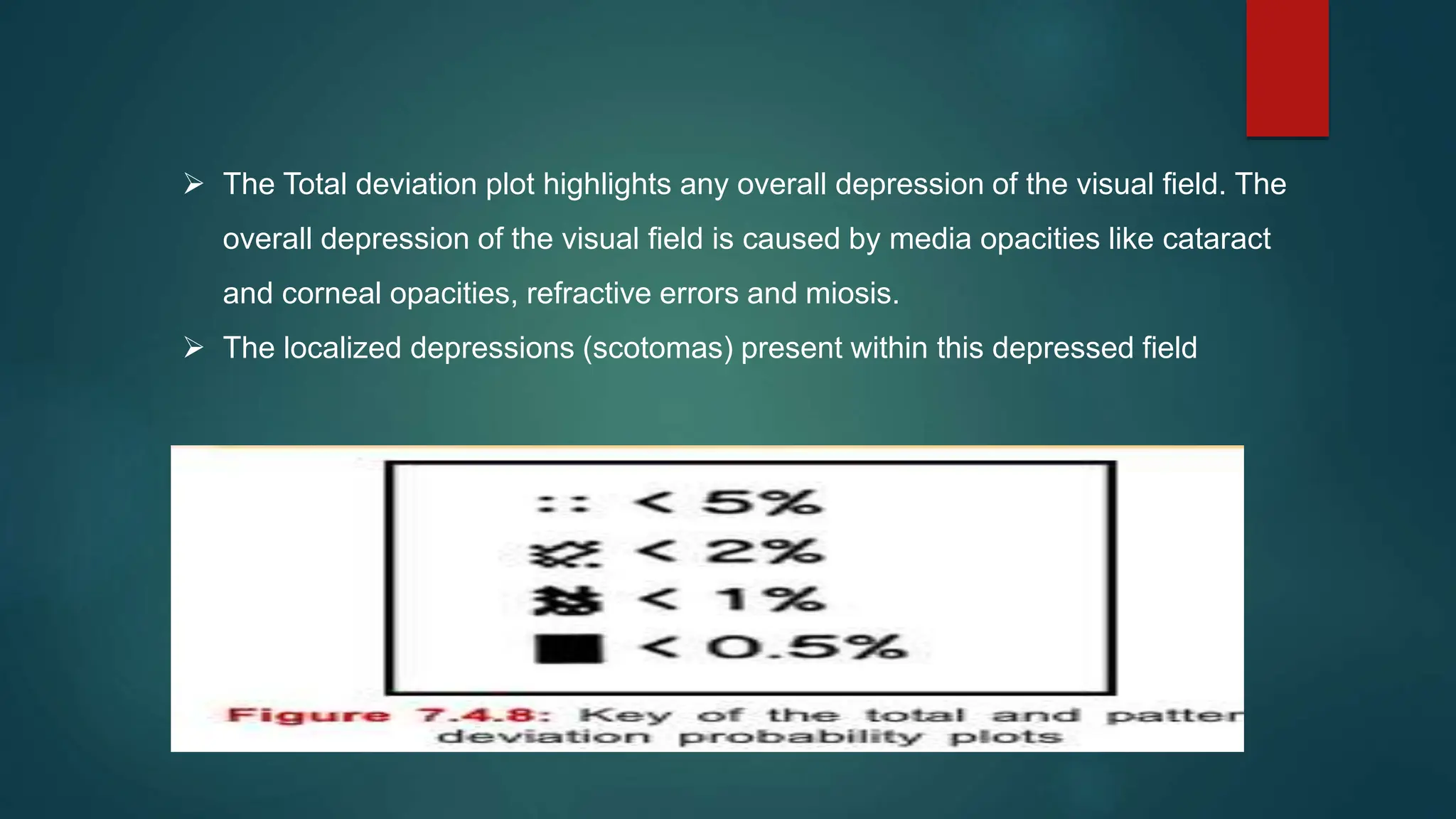
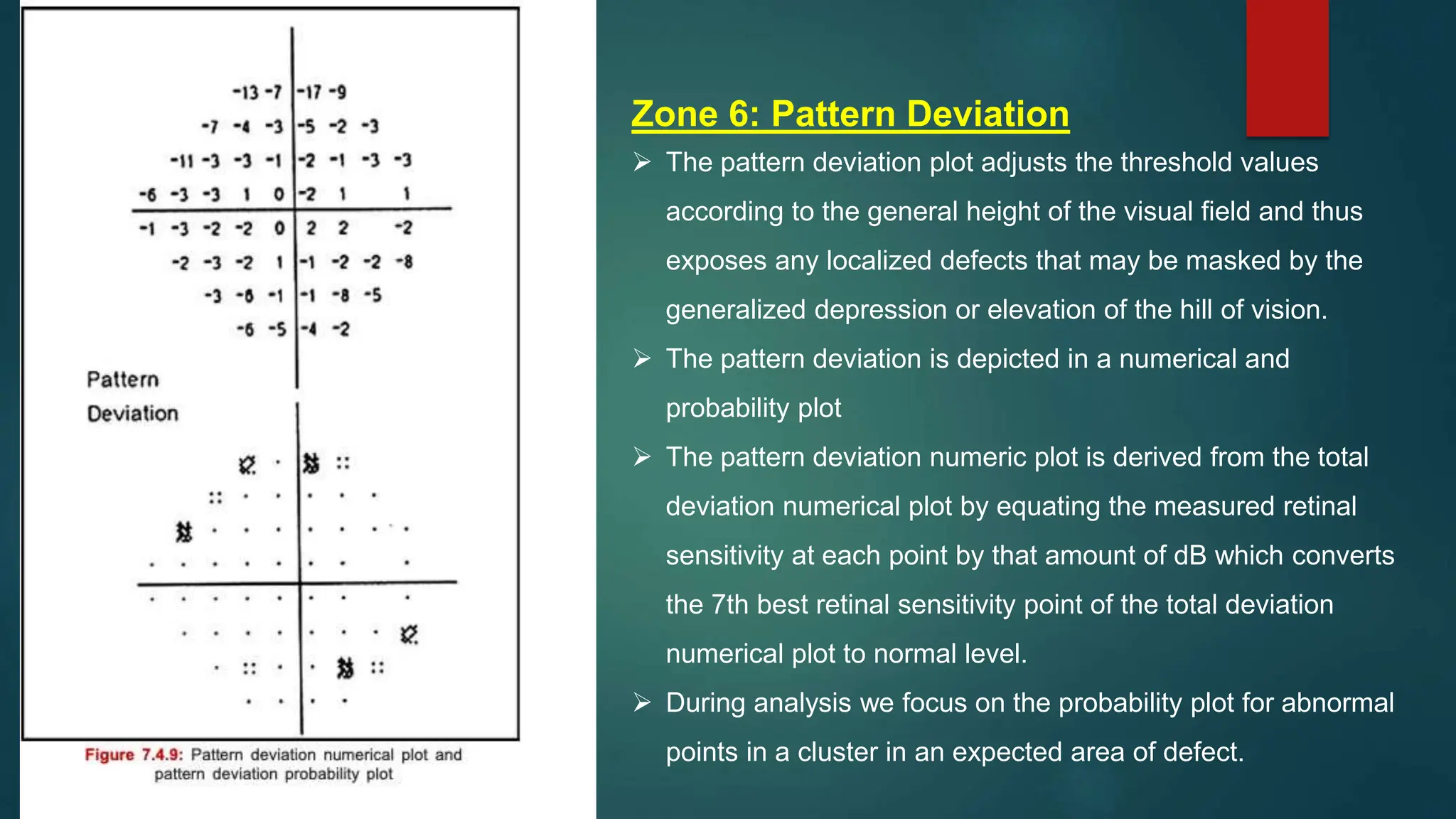
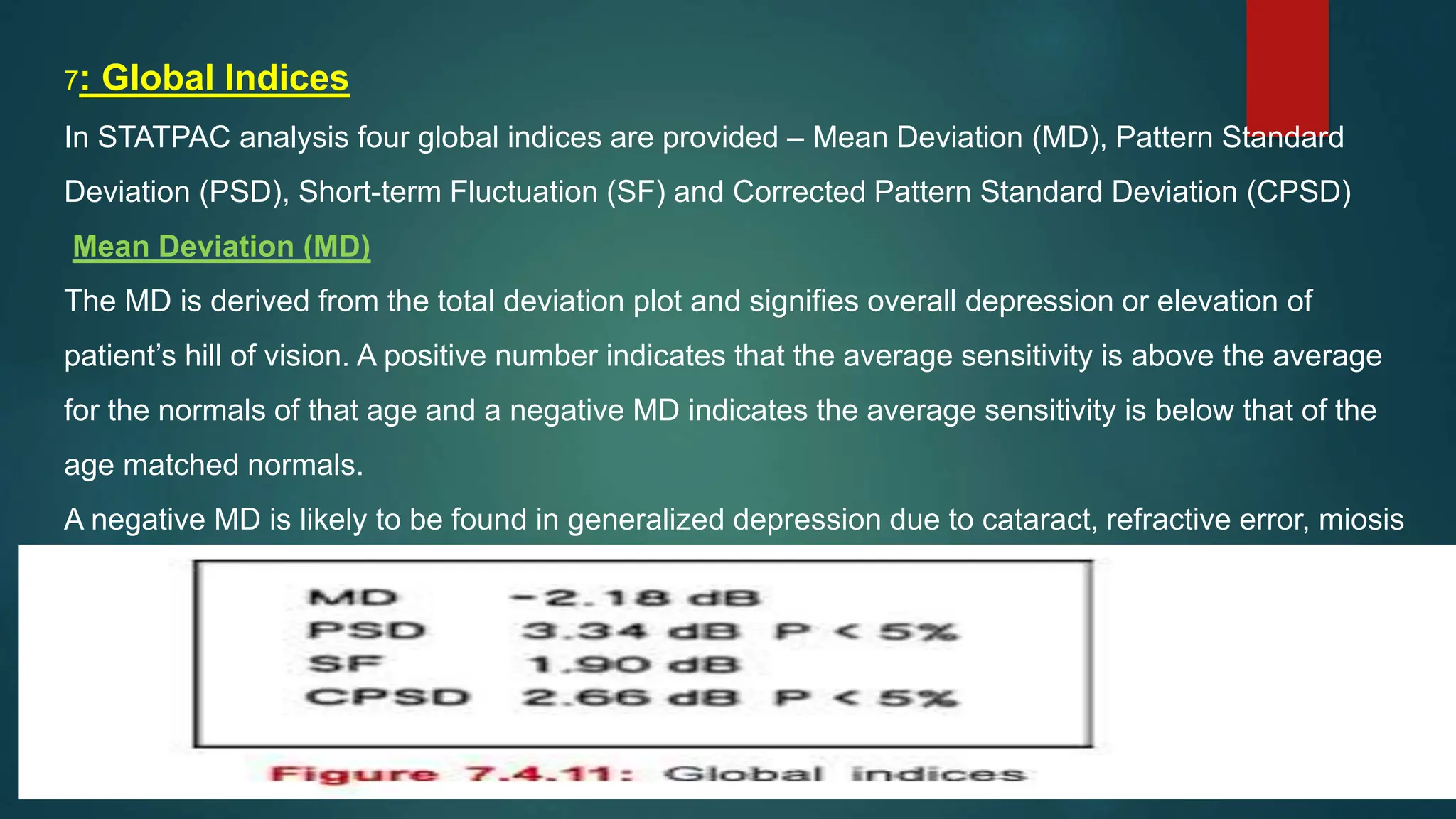
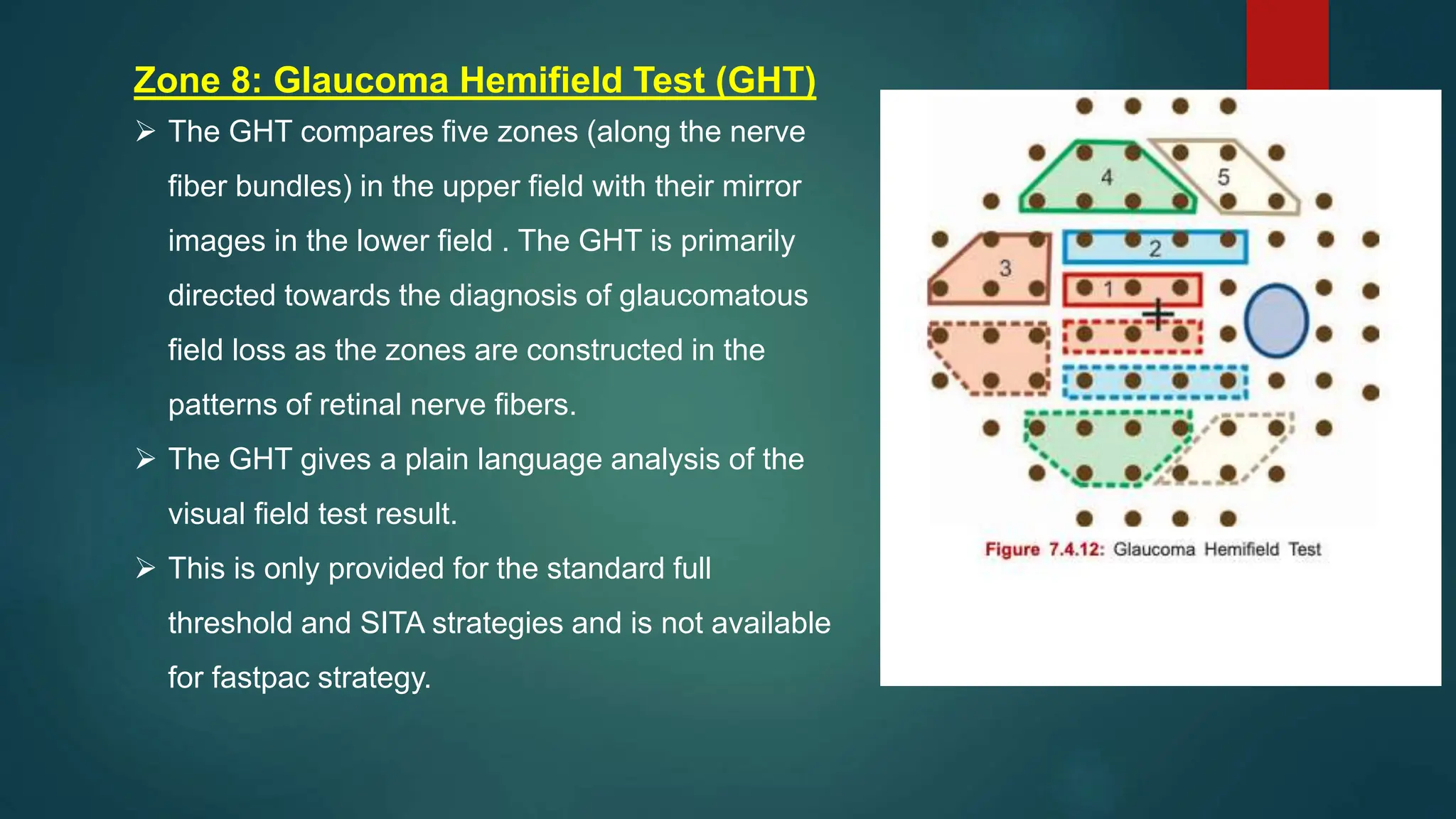
The document provides an in-depth overview of Humphrey Visual Field Analysis, explaining the definition of visual field, its testing methods, and the functionalities of the Humphrey Field Analyzer (HFA). It details various aspects such as stimulus size, intensity, fixation monitoring, threshold strategies, and data analysis approaches related to assessing visual field performance and diagnosing conditions like glaucoma. It also covers patient preparation, instructional guidelines, and parameters that influence test accuracy, emphasizing the importance of correct refractive correction and monitoring during the test.