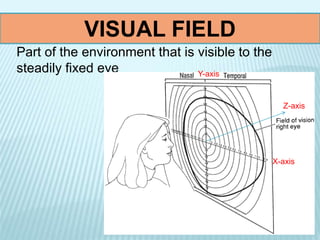
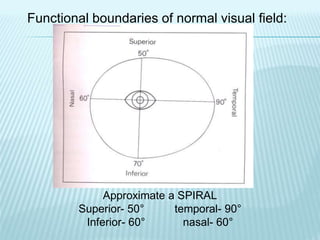
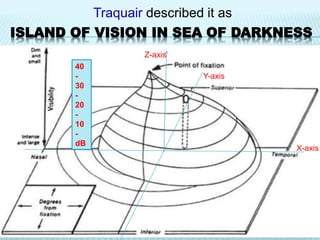
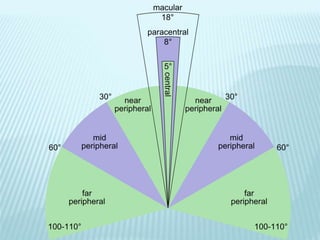
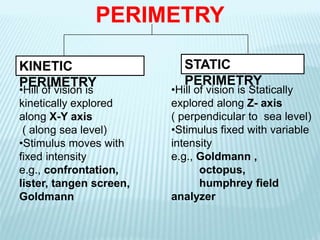
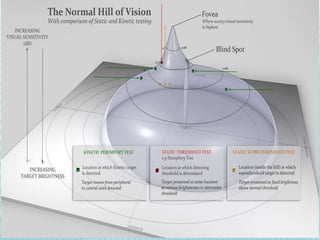
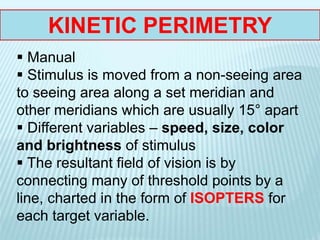
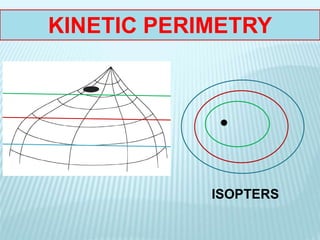
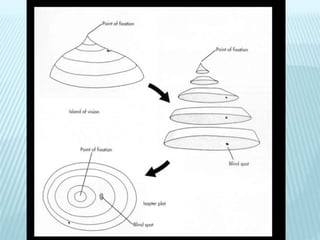
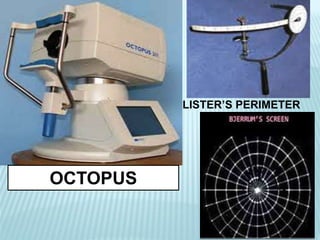
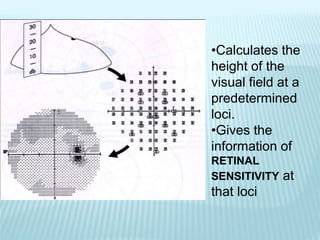
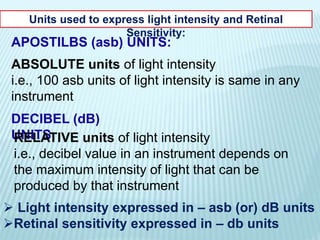
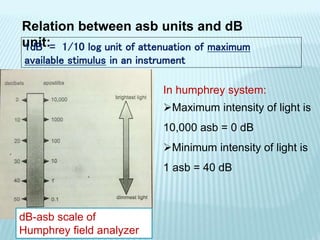
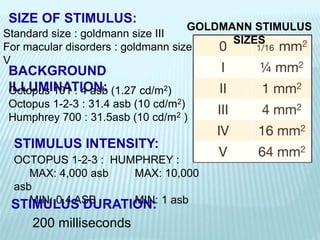
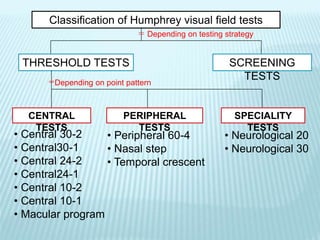
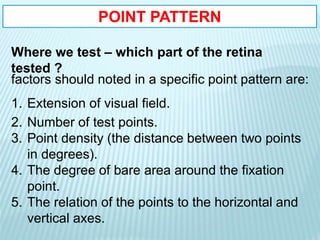
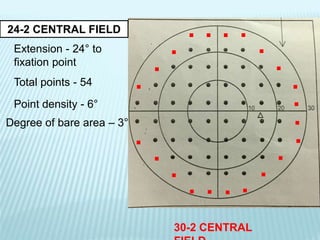
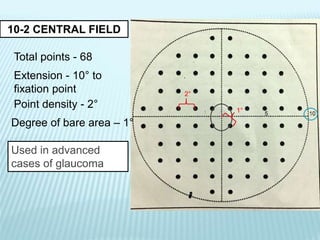
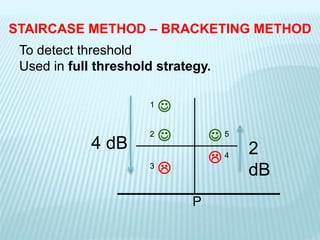
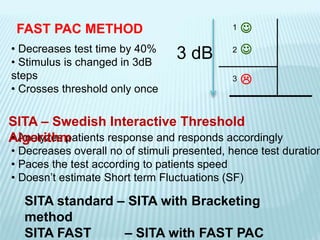
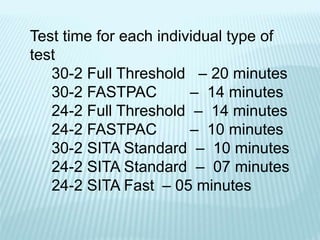
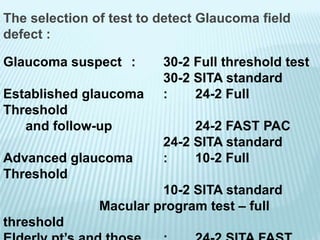
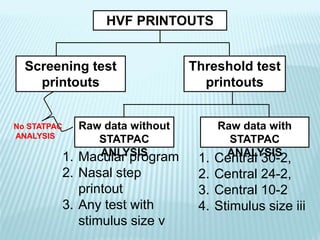
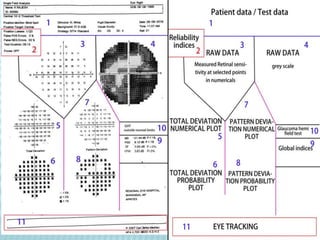
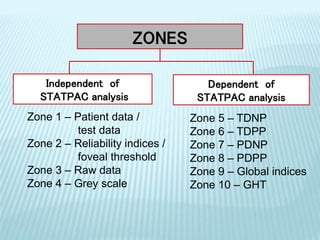
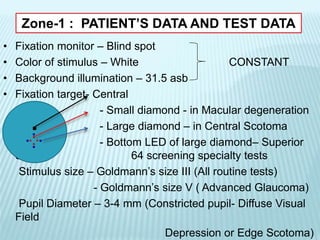
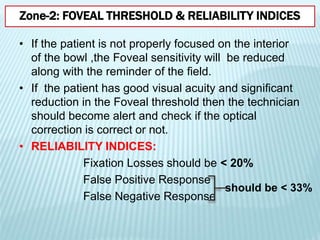
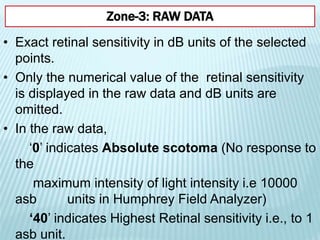
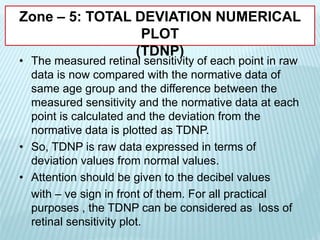
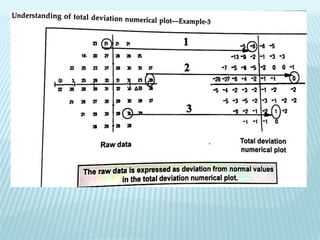
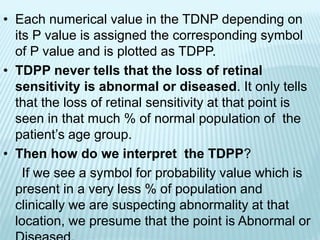
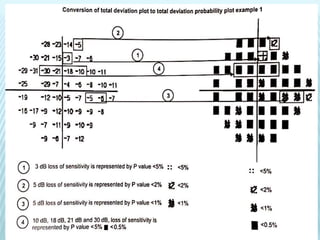
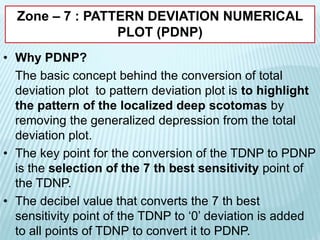
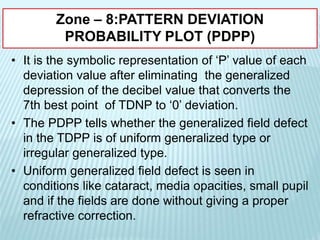
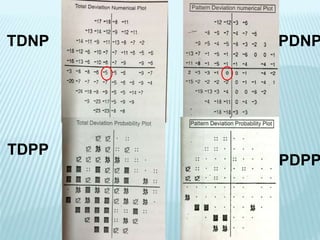
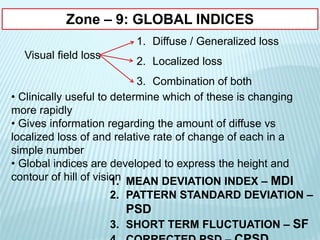
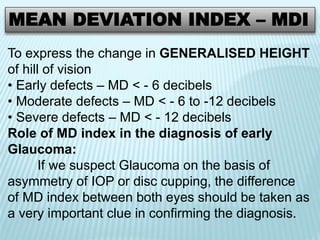
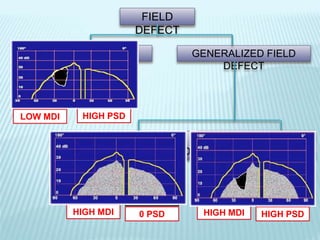
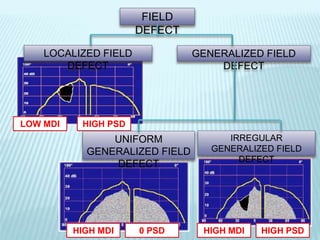
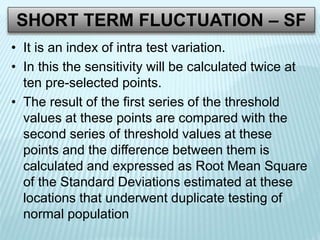
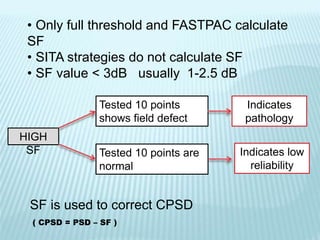
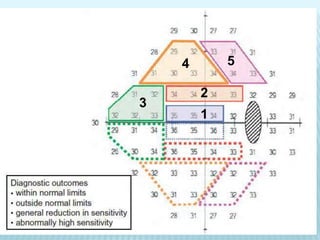
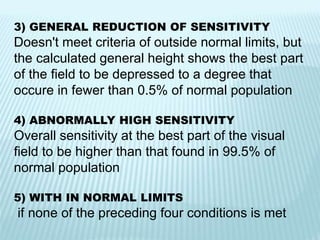
This document provides information about visual field testing. It discusses the anatomy of the visual field and hill of vision. It describes different types of perimetry tests including kinetic and static perimetry. It explains variables used in perimetry like stimulus intensity and size. It provides details about different visual field tests on Humphrey like point patterns, testing strategies, durations and printouts. It discusses analyzing visual field results including reliability indices and total and pattern deviation plots.