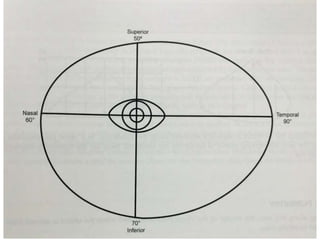
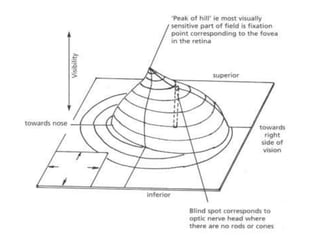
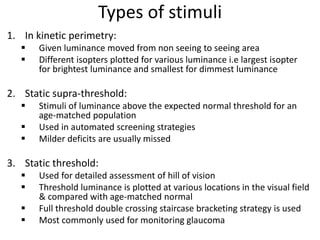
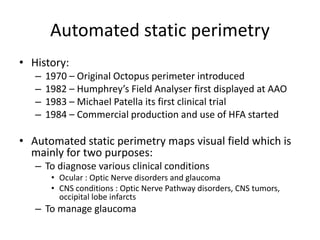
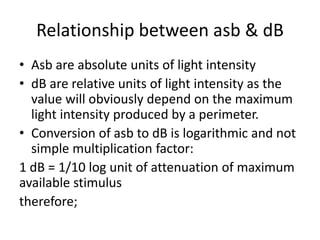
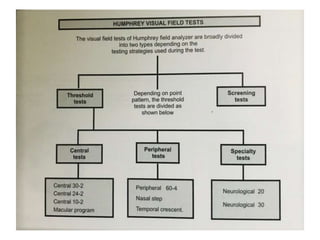
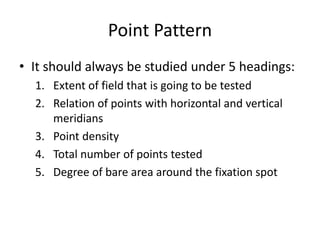
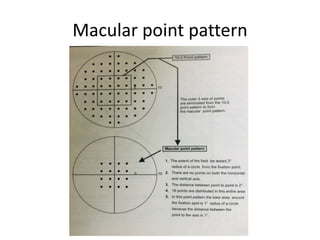
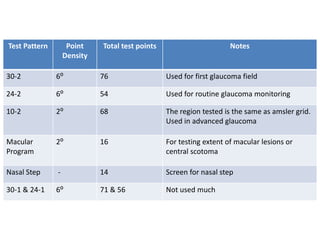
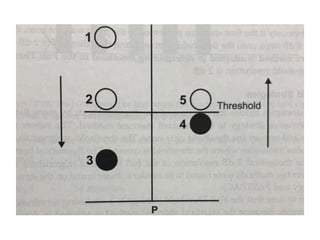
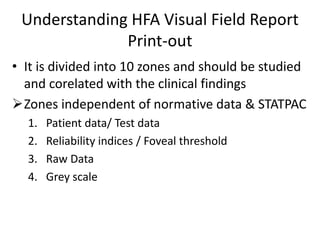
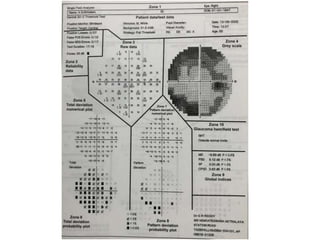
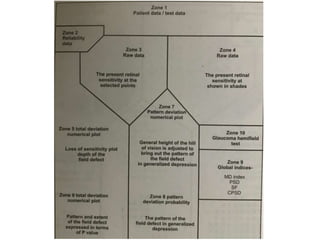
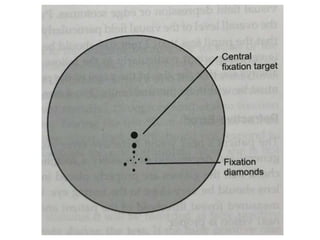
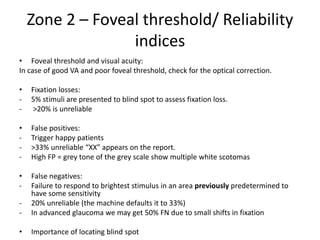
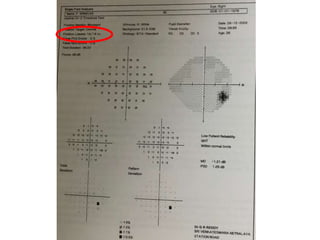
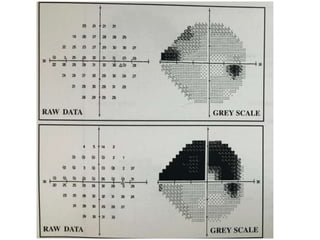
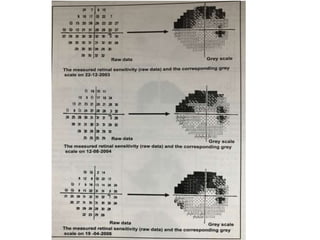
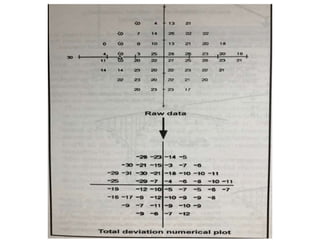
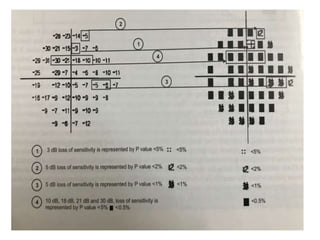
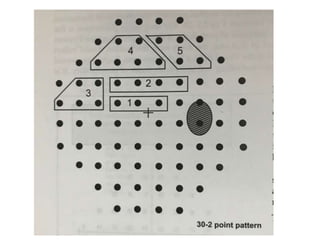
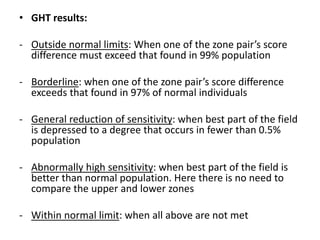
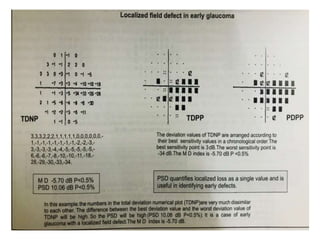
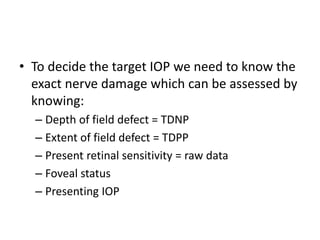
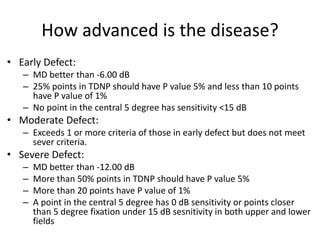
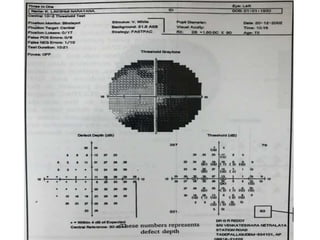
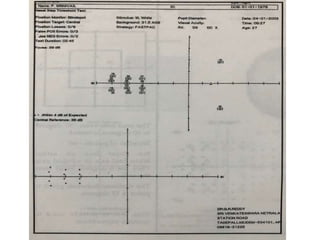
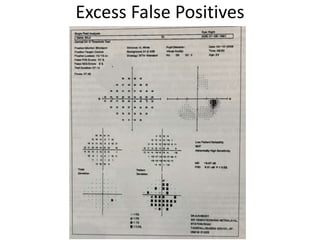
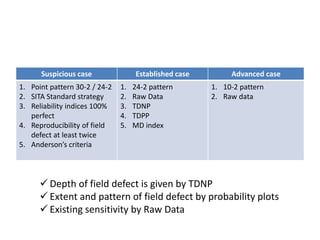
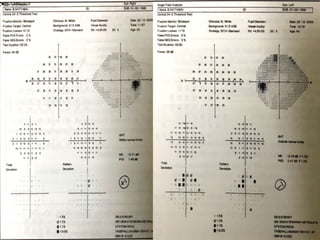
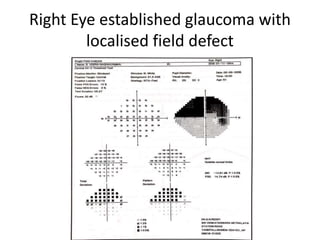
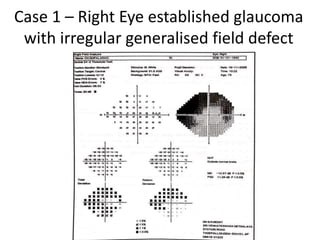
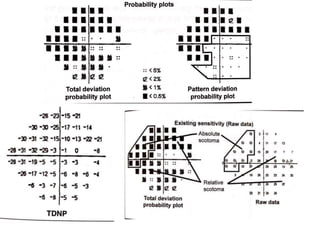
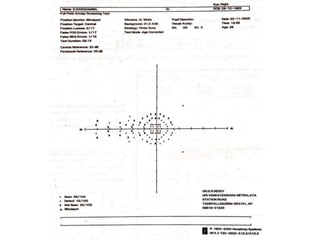
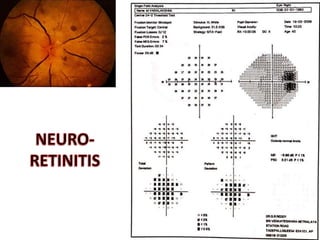
This document covers the essential aspects of perimetry, including the definition and types of visual field testing, which consist of kinetic and static perimetry. It elaborates on the tools and strategies employed for testing, including the examination of key concepts like scotomas, luminance, and the various automated perimetry systems available. The text also discusses the interpretation of visual field reports, focusing on criteria for diagnosing and monitoring glaucoma.