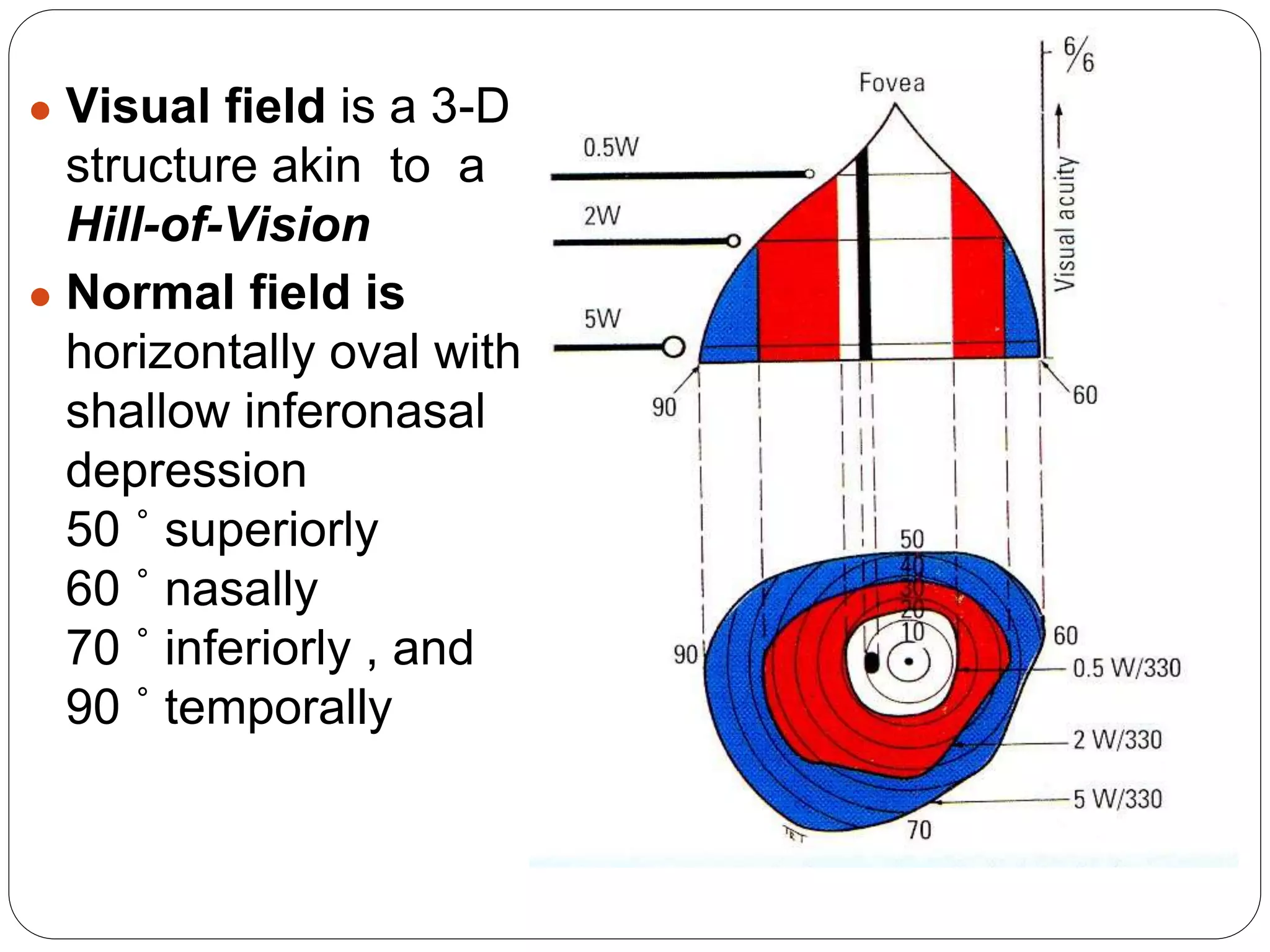
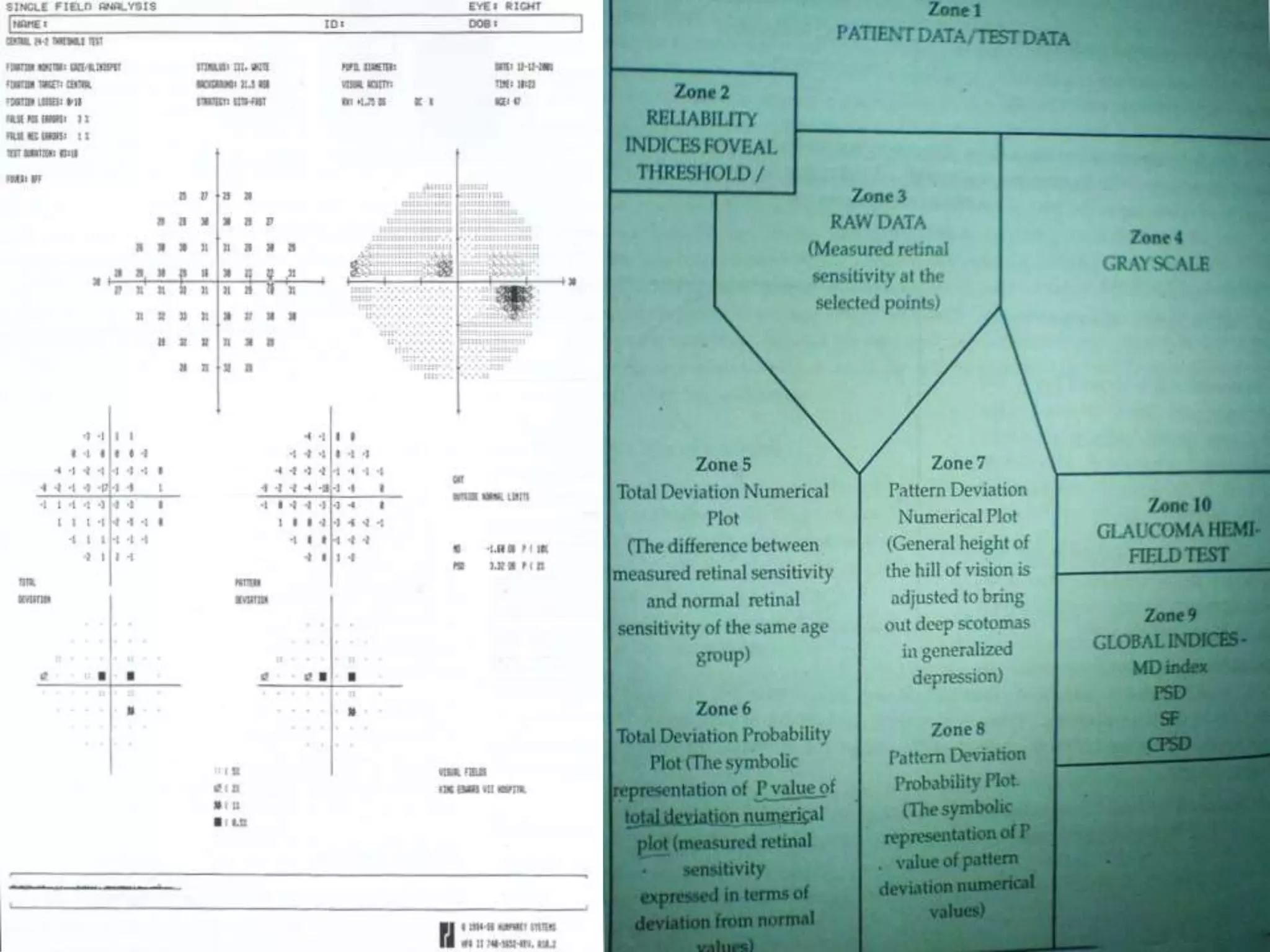
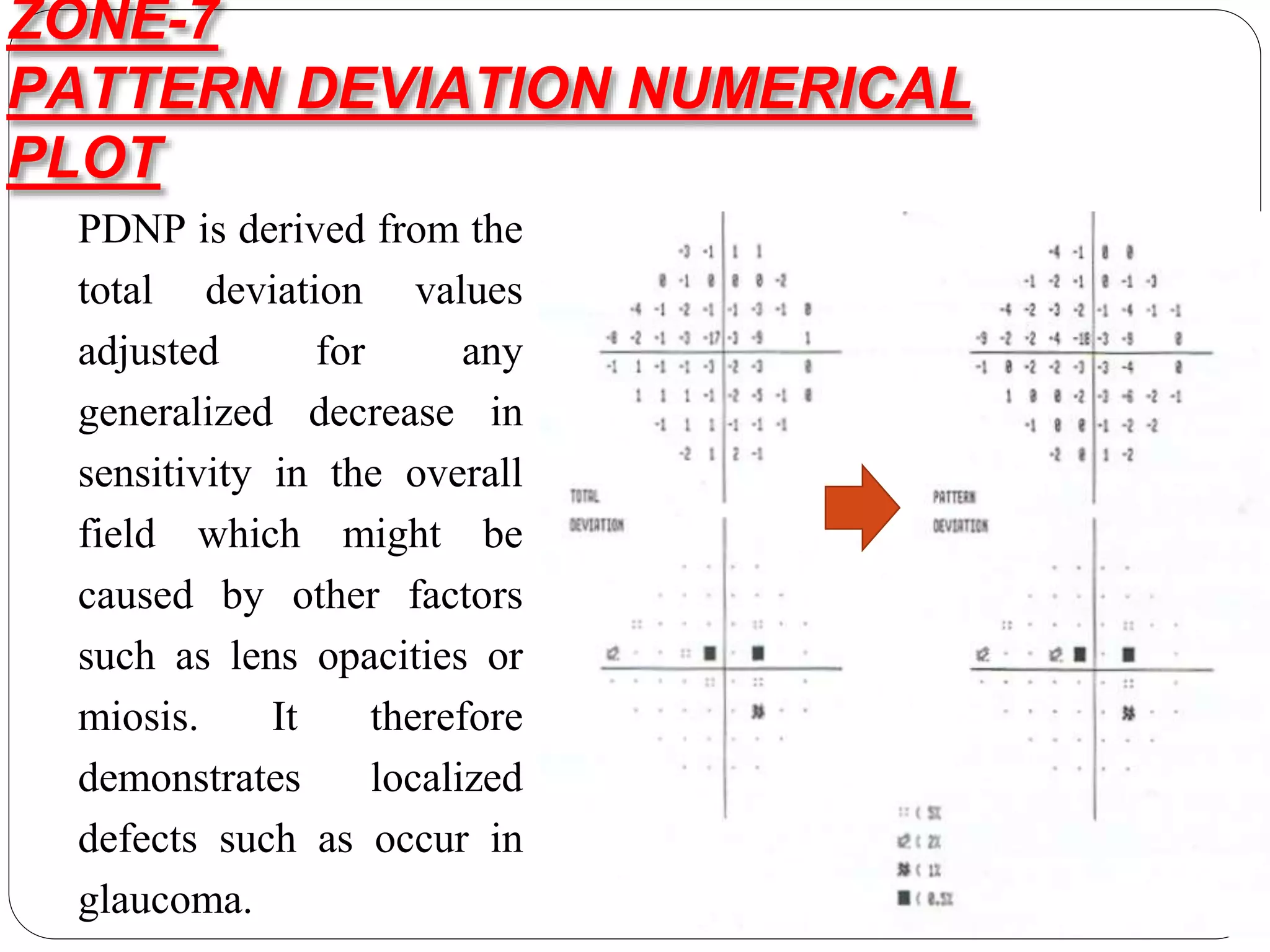
The document discusses automated perimetry, which quantifies sensitivity across the visual field. It describes key terminology like isopters, scotomas, and luminance. Different testing strategies are outlined, including threshold perimetry using SITA. Printout zones are explained, such as raw data, reliability indices, and global indices like mean deviation. Common defects are described. Visual field progression is monitored using GPA event and trend analysis.