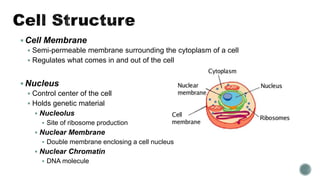
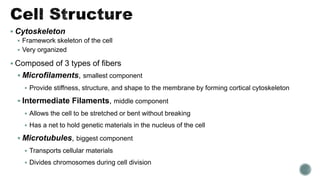
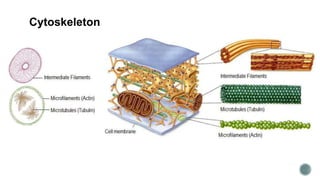
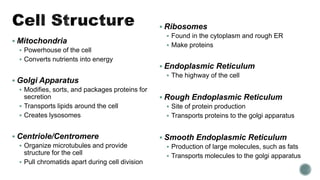
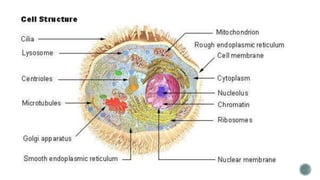
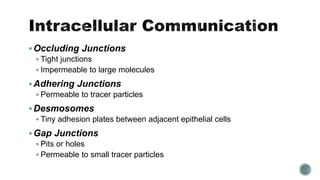
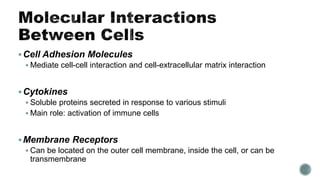
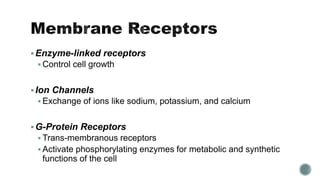
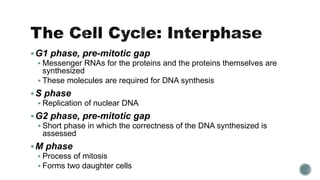
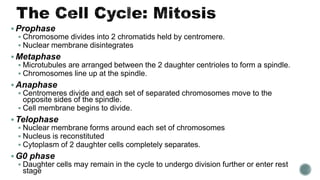
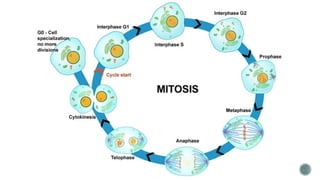
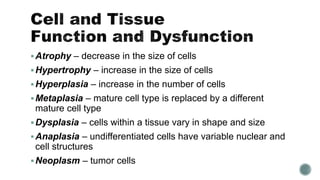
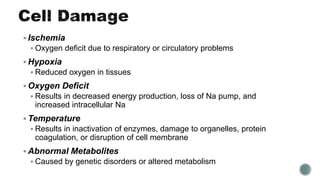
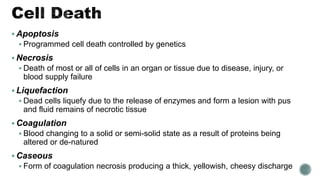
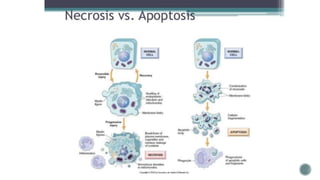
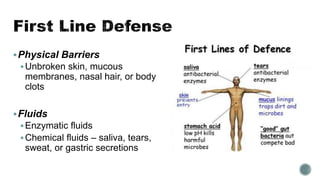
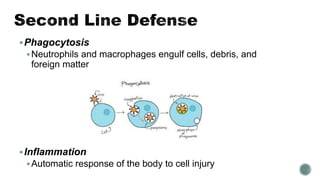
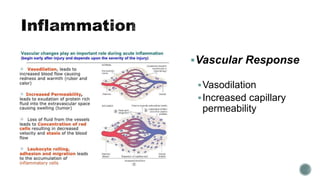
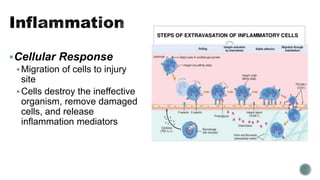
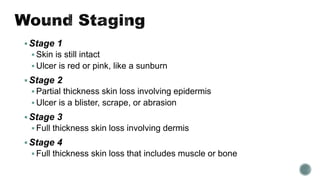
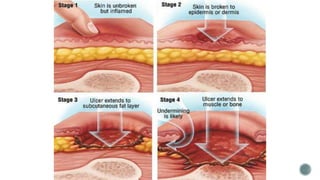
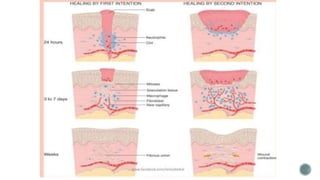
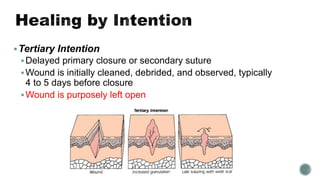
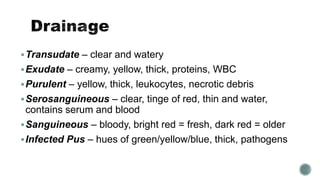
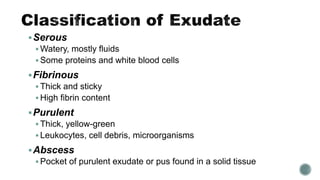
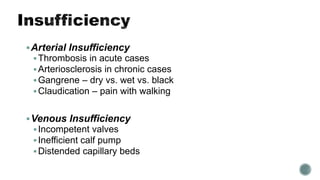
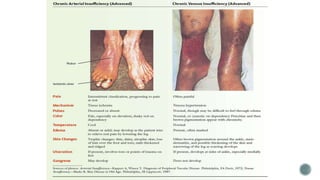
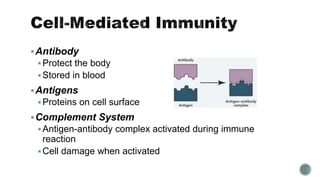
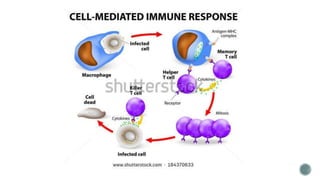
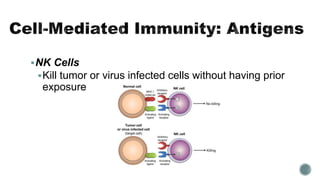
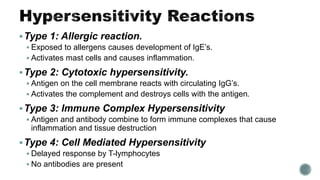
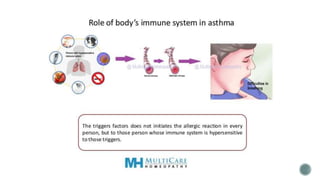
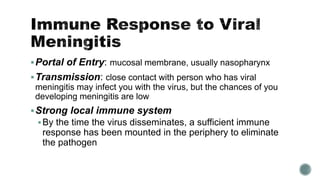
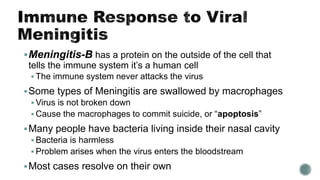
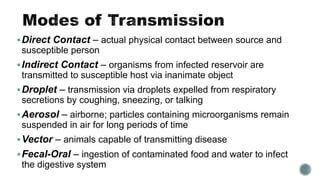
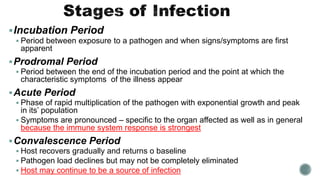
The document provides a comprehensive overview of cellular structures, functions, and various biological processes involving cell injury, inflammation, and immune responses. It discusses cellular components such as the nucleus, mitochondria, and ribosomes, as well as processes like apoptosis, necrosis, and the immune response, including types of hypersensitivity reactions. Additionally, it covers various diseases, infections, and their mechanisms, alongside descriptions of healing processes and immune system functions.