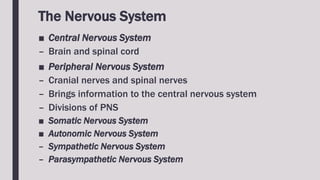
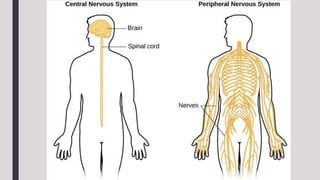
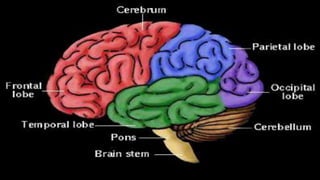
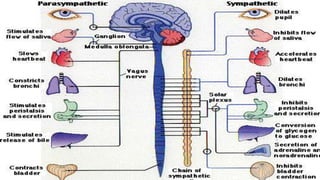
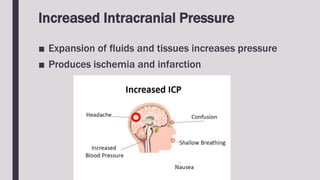
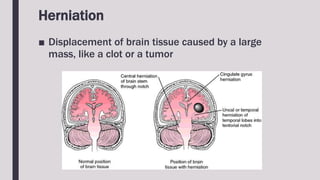
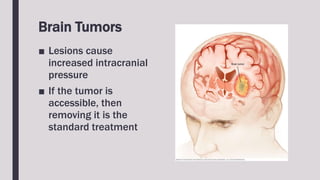
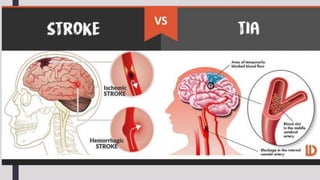
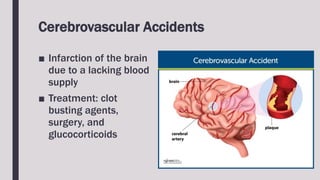
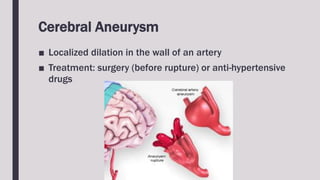
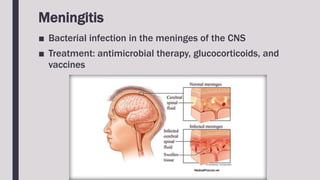
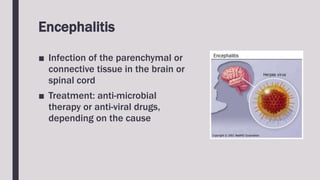
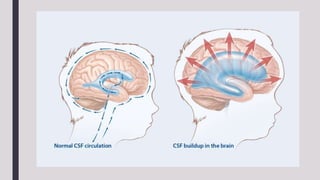
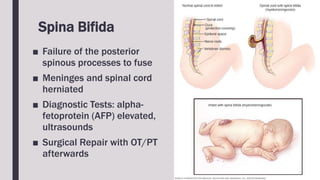
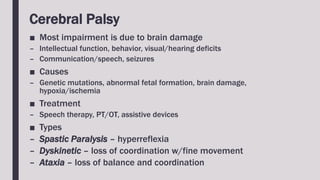
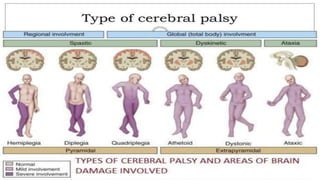
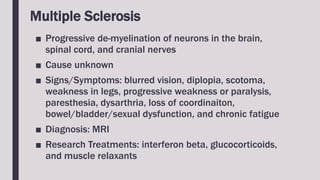
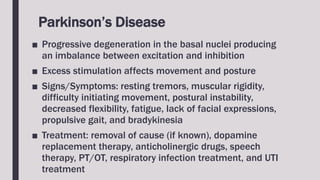
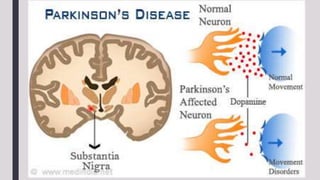
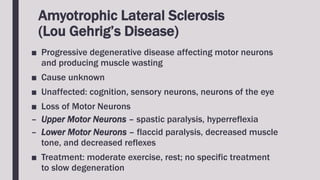
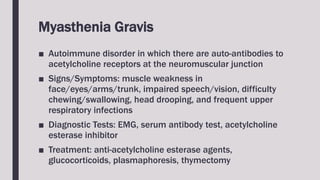
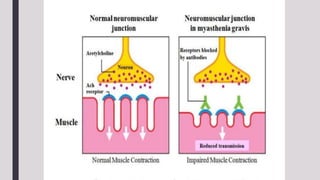
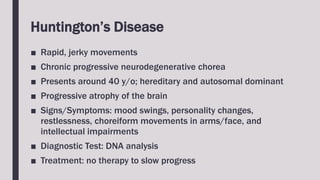
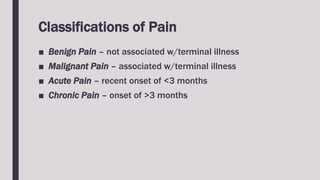
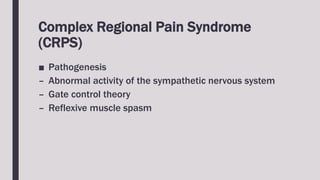
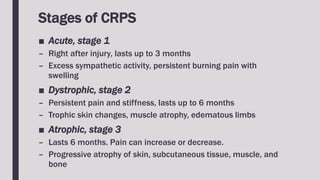
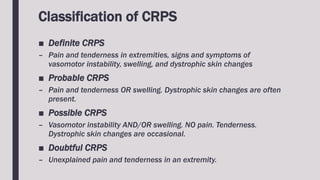
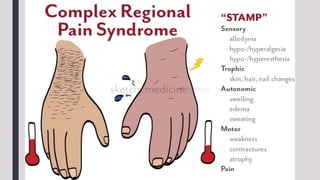
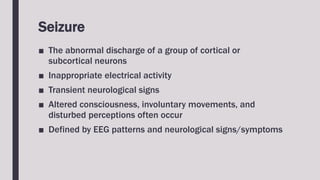
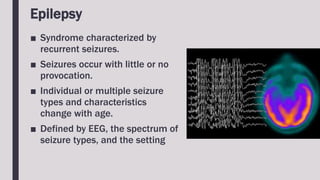
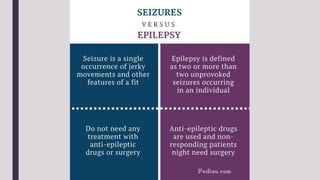
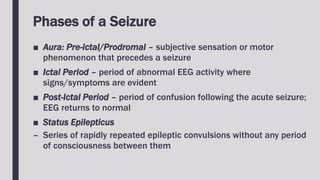
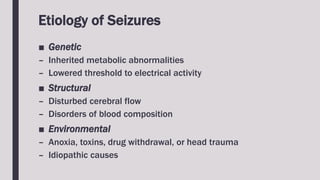
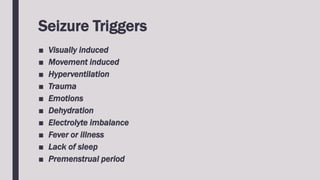
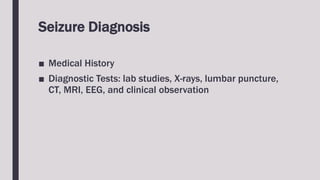
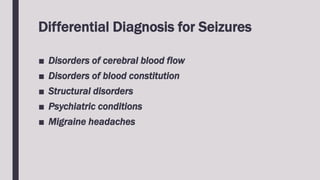
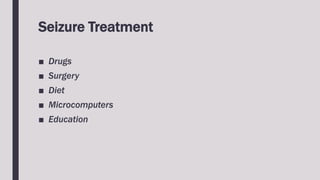
The document outlines the structure and function of the nervous system, detailing the central and peripheral nervous systems along with their components. It covers various neurological disorders, including acute and chronic conditions, their causes, symptoms, and treatments. Additionally, it explains pain perception and seizures, providing insights into their classification, diagnosis, and management.