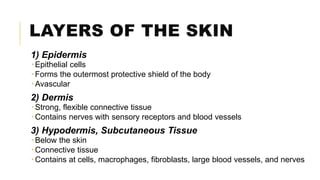
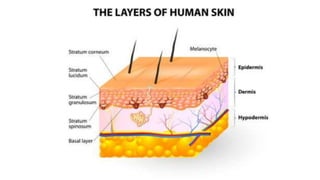
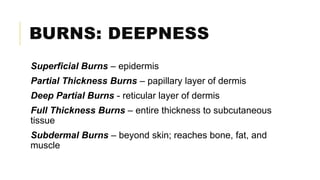
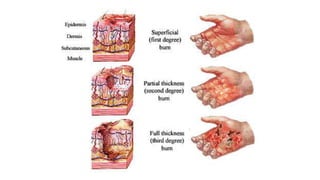
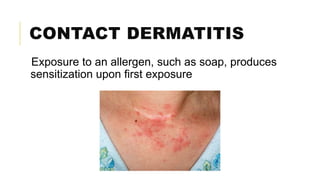
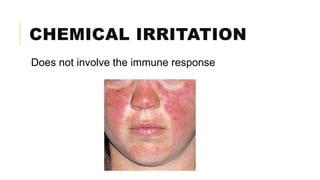
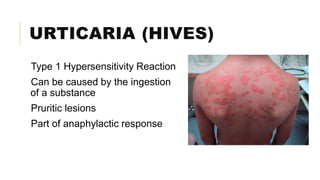
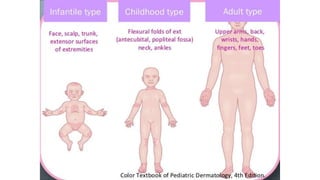
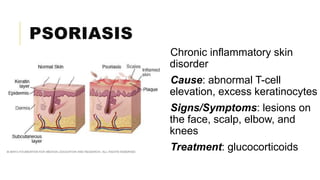
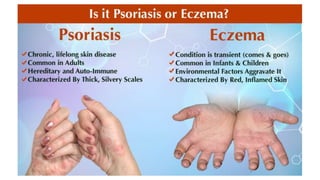
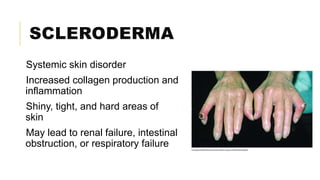
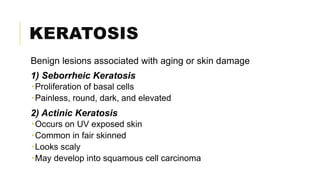
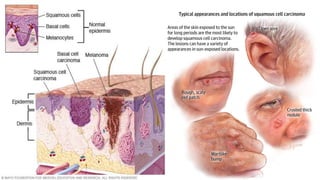
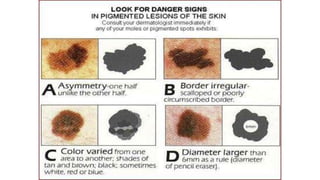
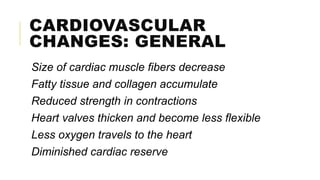
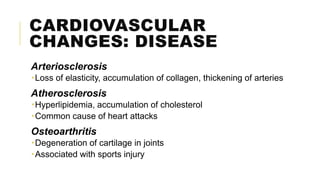
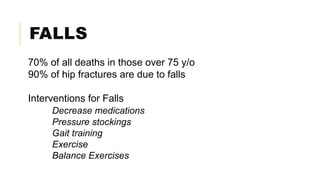
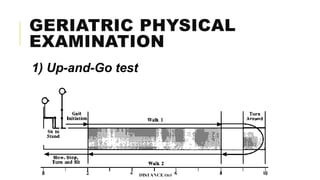
The document outlines the functions and layers of the skin, detailing the pathophysiology of burns and various inflammatory skin disorders. It also discusses skin cancer types, physiological changes associated with aging, and the cardiovascular and neurologic changes that occur, emphasizing fall risks in the elderly. Interventions for fall prevention and geriatric physical examinations are mentioned as crucial in managing these age-related challenges.