The document discusses pathology of the cervix, including:
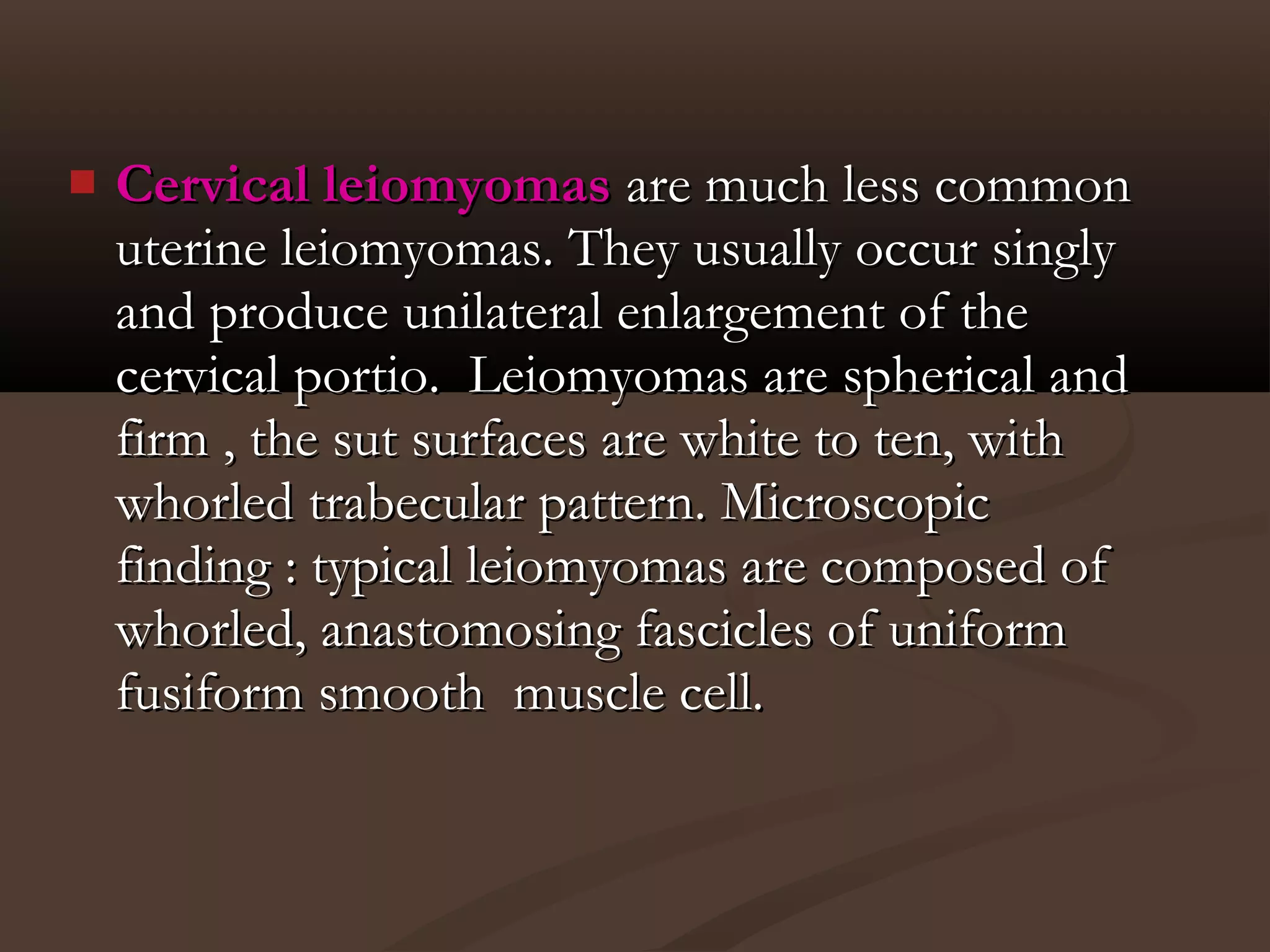
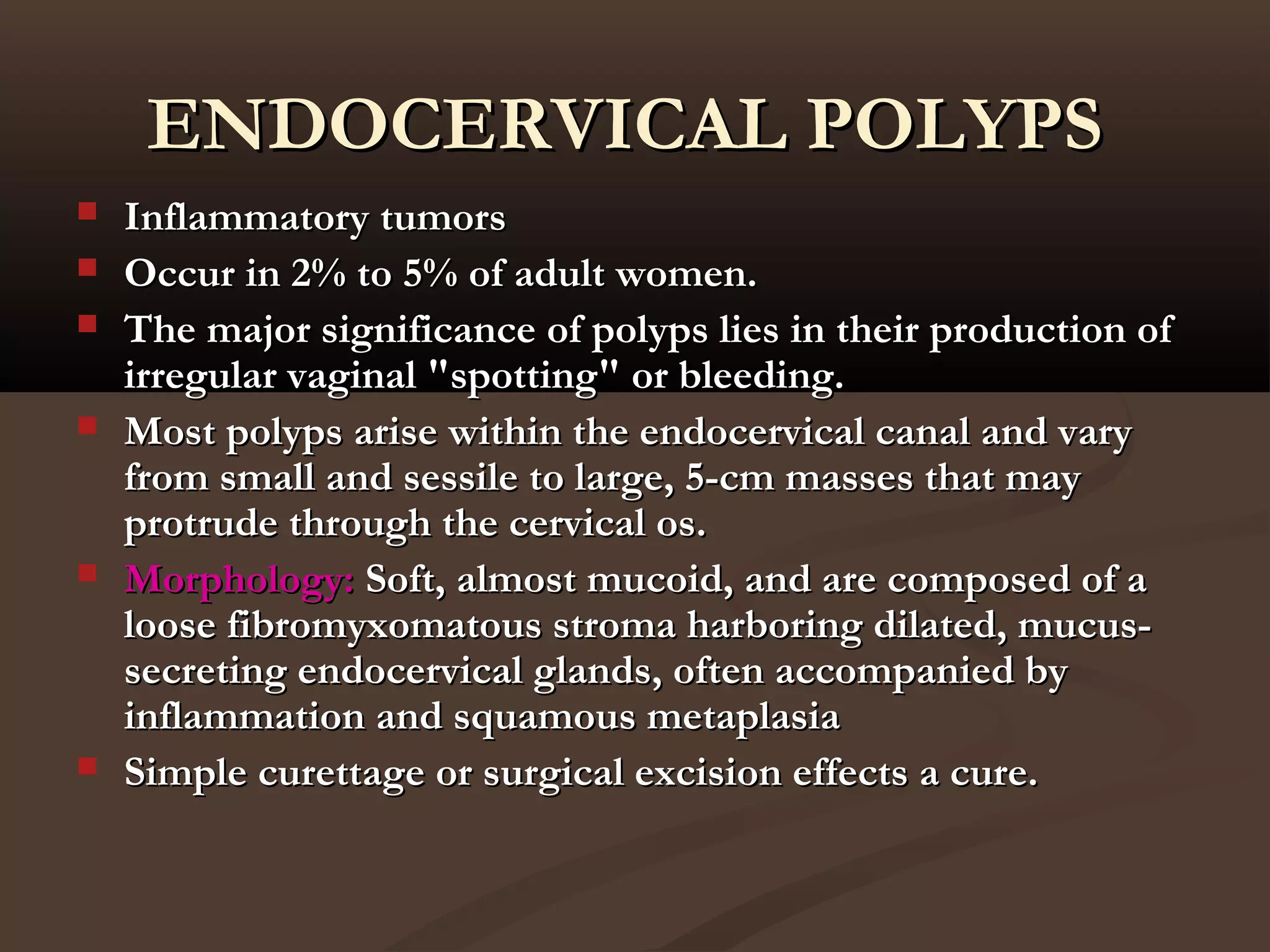
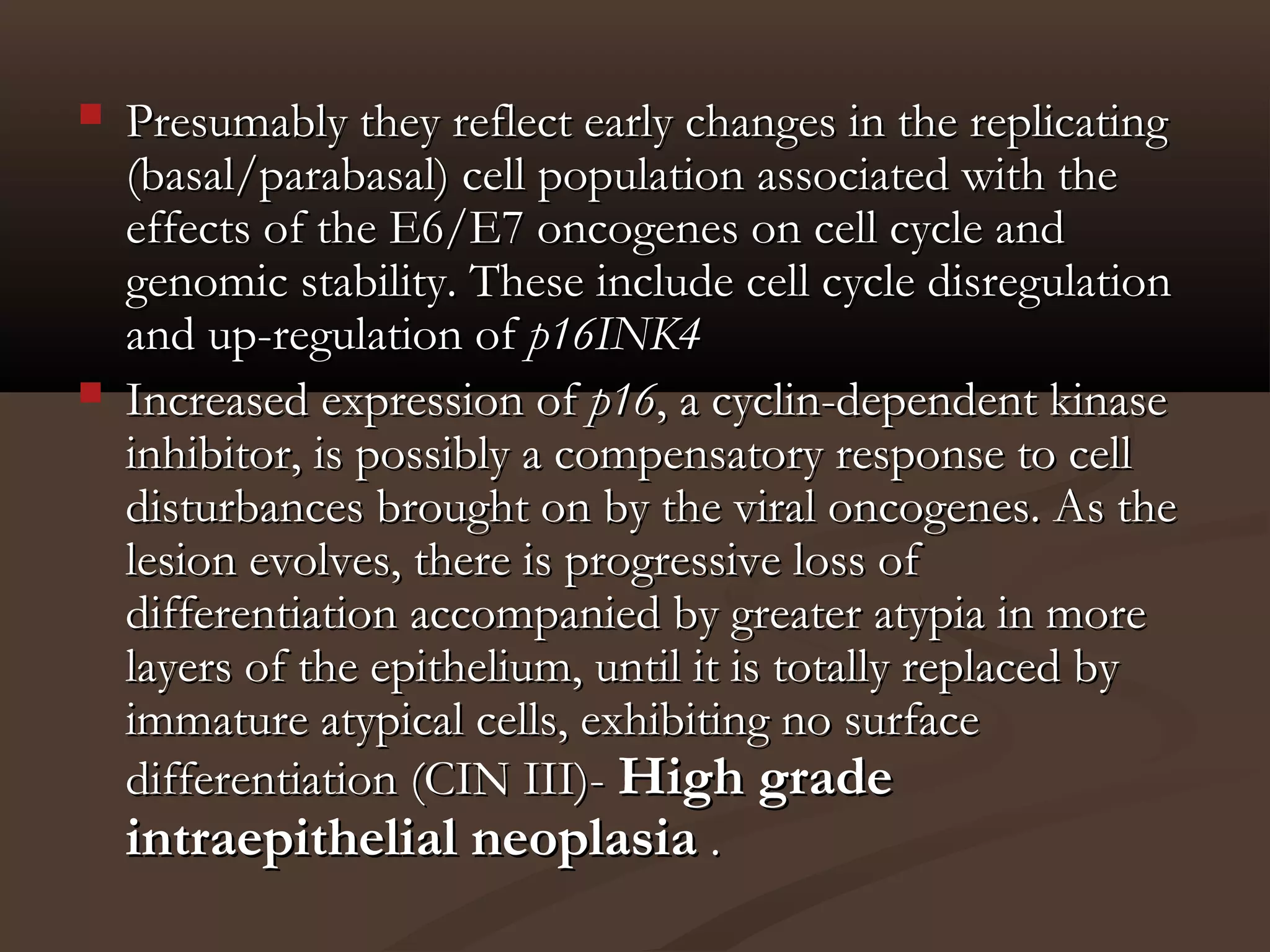
1. Benign diseases like inflammations (acute and chronic cervicitis), metaplasias, hyperplasias, and benign tumors like endocervical polyps and leiomyomas.
2. Precancerous lesions like squamous intraepithelial lesions and glandular intraepithelial lesions.
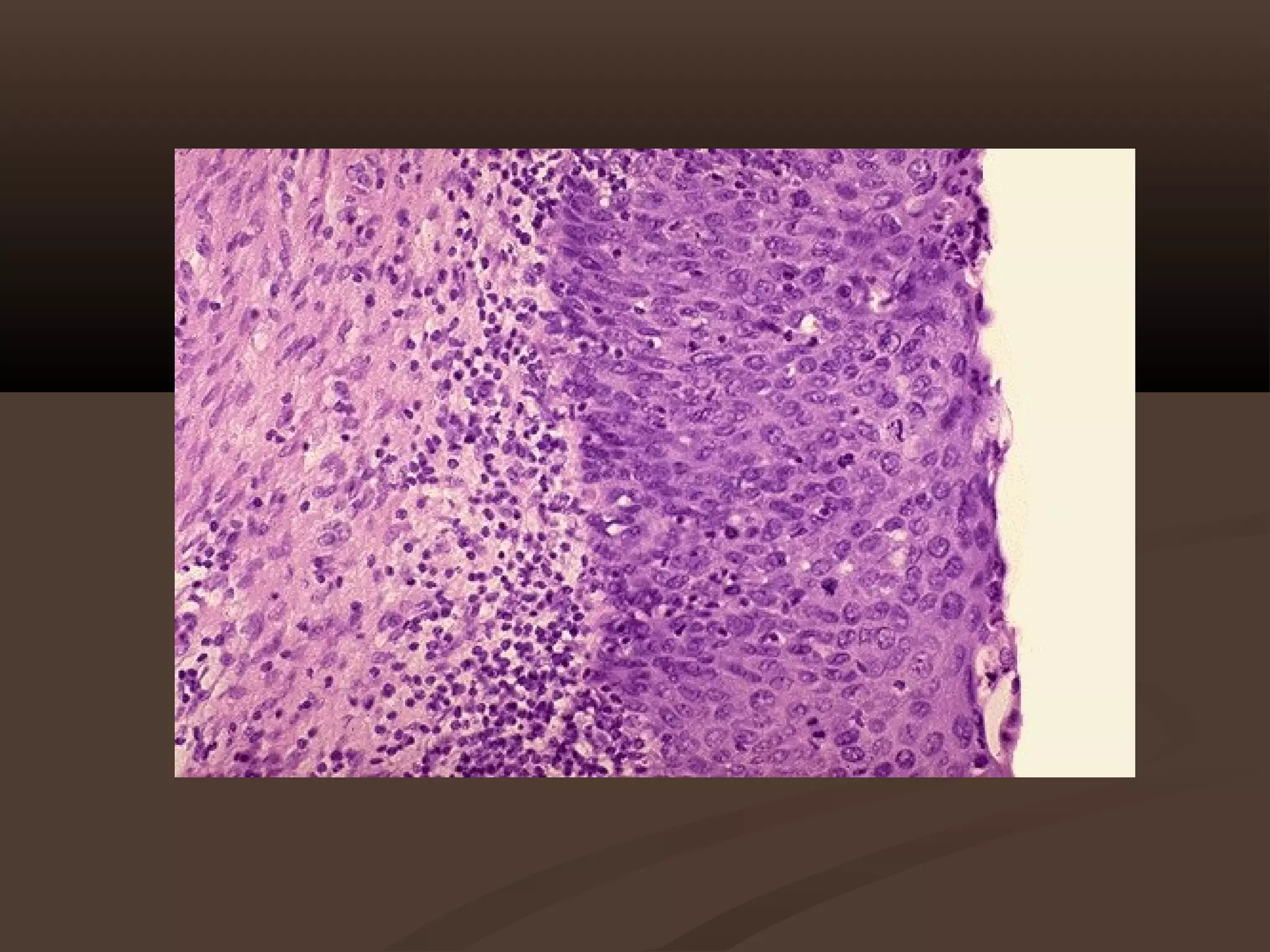
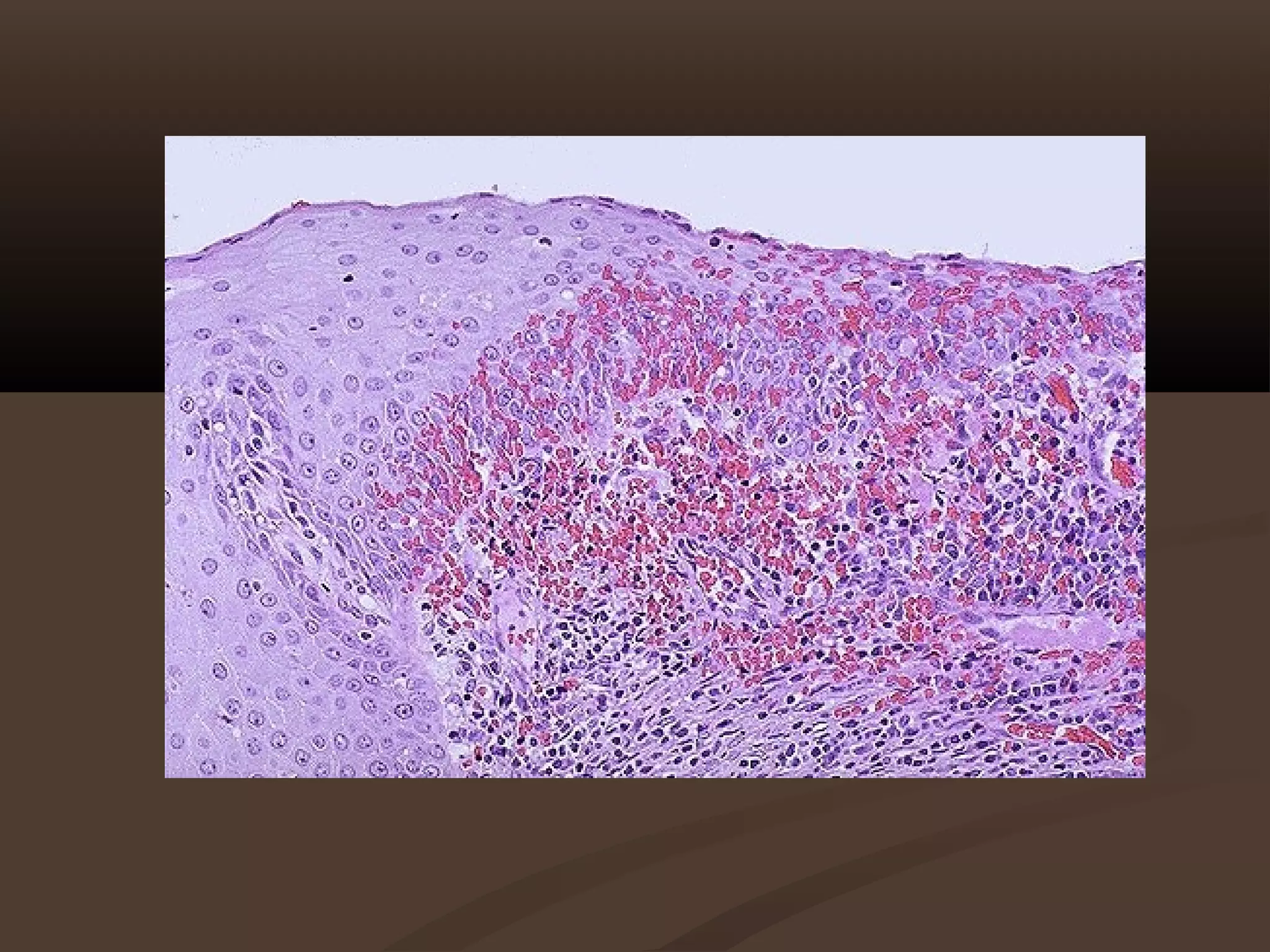
3. Cancerous tumors including invasive carcinomas, mesynchymal tumors, mixed epithelial mesynchymal tumors, and other rare tumor types. Chronic cervicitis is most often caused by sexually transmitted pathogens like Chlamydia trachomatis and Neisseria gonorrhoeae. Squamous metaplasia and other


















































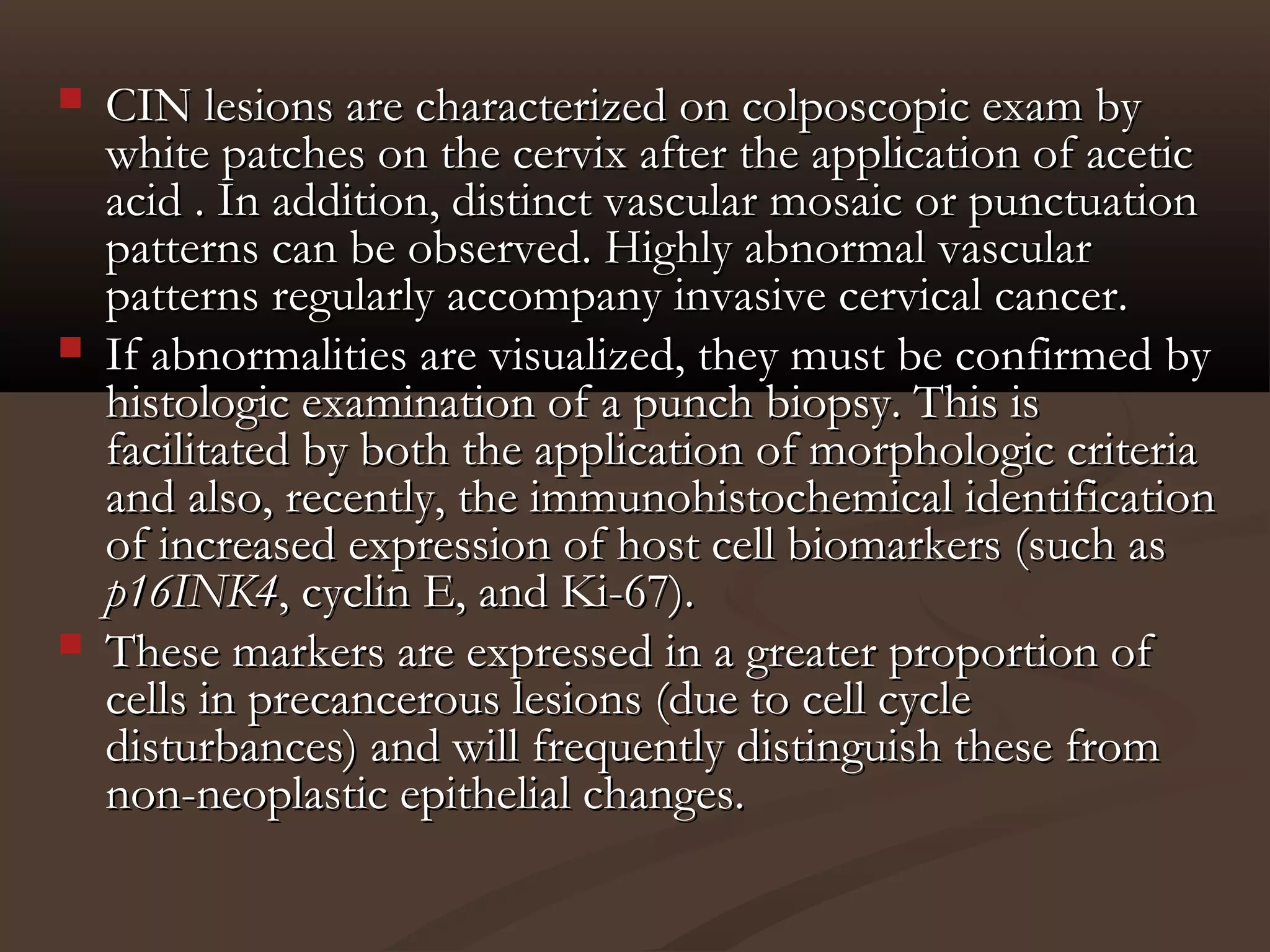





























![Epithelial Changes (Squamous Cell)Epithelial Changes (Squamous Cell)
Atypical squamous cells of undetermined significanceAtypical squamous cells of undetermined significance
(ASCUS) --(ASCUS) -- the most common type of abnormal result.the most common type of abnormal result.
It is not cancer. It is often due to infection or irritation. Many timesIt is not cancer. It is often due to infection or irritation. Many times
these resolve on their own.these resolve on their own.
Most women will be re-tested in a few months. High risk womenMost women will be re-tested in a few months. High risk women
will have colposcopy right away.will have colposcopy right away.
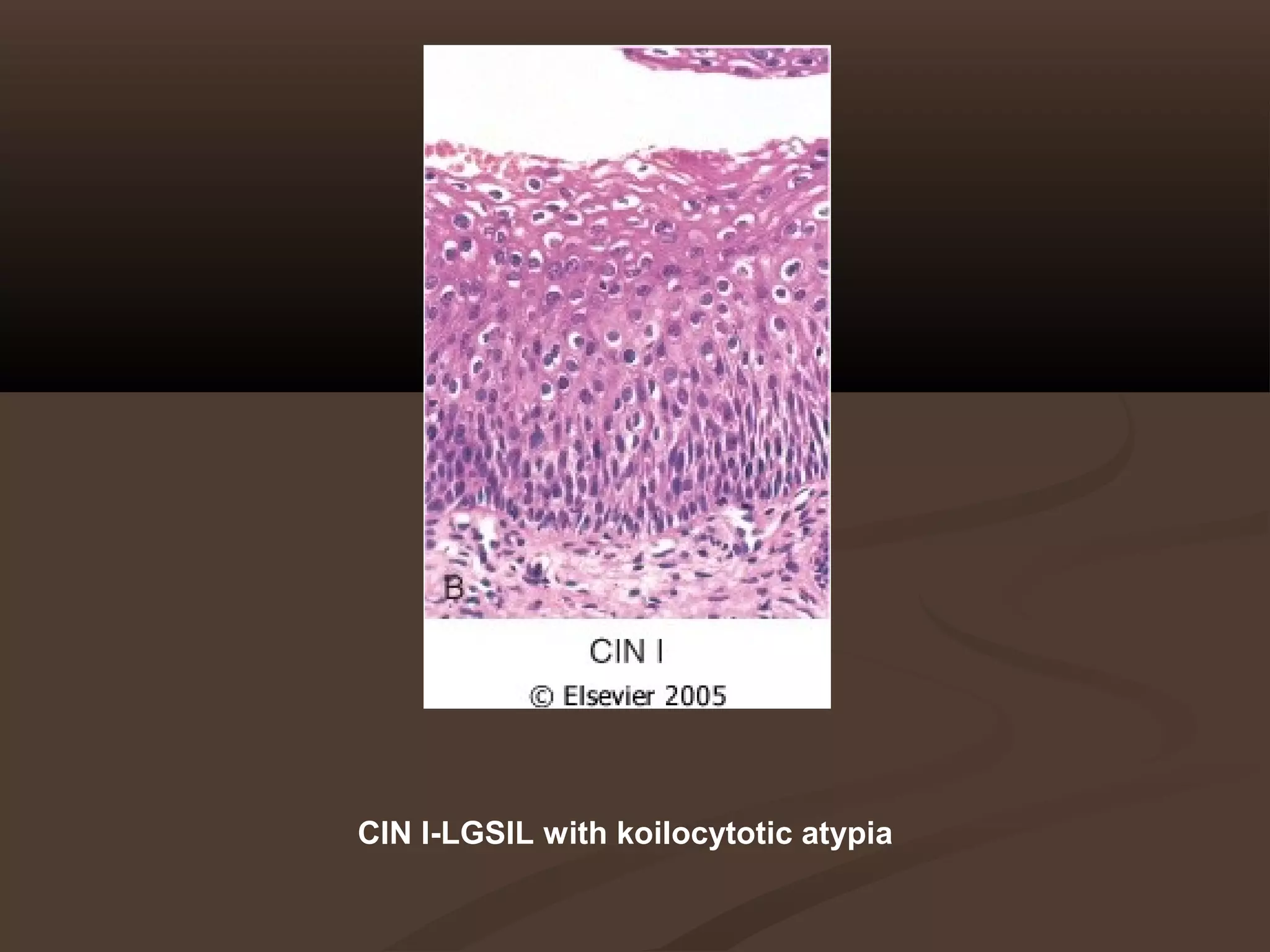
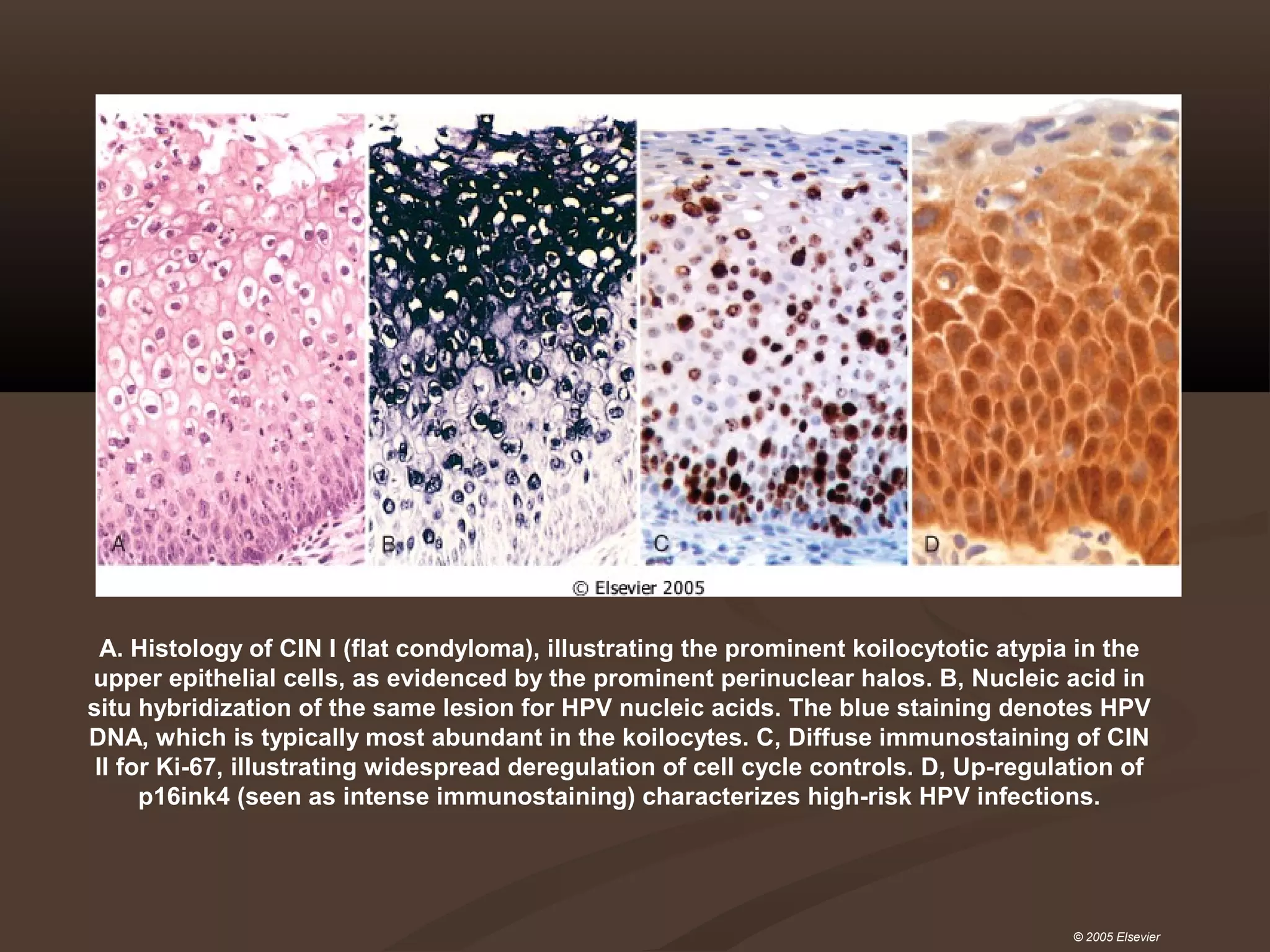
Squamous intraepithelial lesion (SIL)Squamous intraepithelial lesion (SIL)
Low-grade squamous intraepithelial lesion (LSIL)--Low-grade squamous intraepithelial lesion (LSIL)-- AA
woman with these result will usually have a colposcopywoman with these result will usually have a colposcopy
within 4 weeks. It is not yet cancer.within 4 weeks. It is not yet cancer.
Mild dysplasia (cervical intraepithelial neoplasia [CIN]-I)Mild dysplasia (cervical intraepithelial neoplasia [CIN]-I)
---- a woman will usually have a colposcopy right away. Thisa woman will usually have a colposcopy right away. This
is not yet cancer.is not yet cancer.
High-grade squamous intraepithelial lesion (HSIL) SevereHigh-grade squamous intraepithelial lesion (HSIL) Severe
dysplasia and carsinoma in situ (CIN-III) --dysplasia and carsinoma in situ (CIN-III) -- this is cancer,this is cancer,
but limited to the cervix and still has an excellent chance ofbut limited to the cervix and still has an excellent chance of
cure.cure.
Squamous cell carcinomaSquamous cell carcinoma](https://image.slidesharecdn.com/cervix-181006170916/75/PATHOLOGY-OF-THE-CERVIX-108-2048.jpg)



