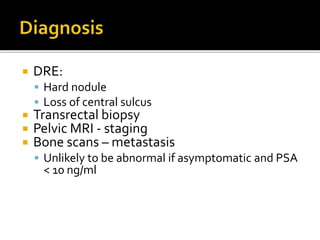
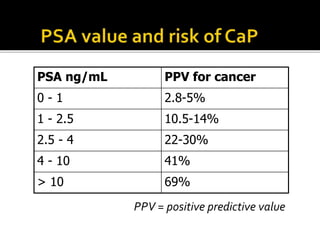
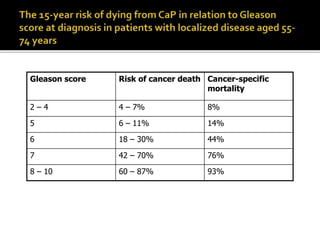
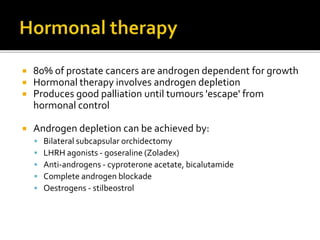
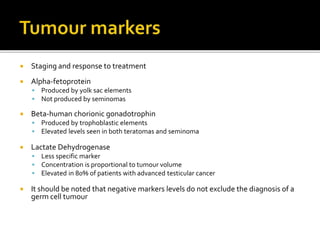
The document discusses prostate cancer, including that it is the most common malignancy of the male urogenital tract, with about 10,000 cases per year in the UK. It is rare before age 50 and found in 80% of men older than 80 upon autopsy. Prostate cancer arises in the prostate gland and can spread through the capsule, lymph nodes, bones, and other sites. Risk factors include family history and diet. Screening includes digital rectal exam and PSA testing, while diagnosis involves biopsy. Staging uses the TNM system and Gleason grading provides a prognosis. Treatment depends on stage and includes surgery, radiation, hormone therapy, and active surveillance.