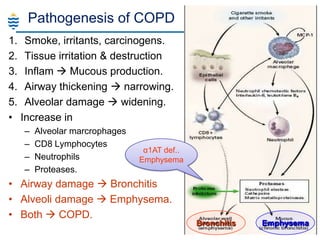
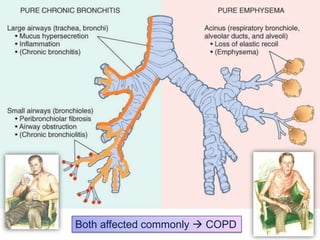
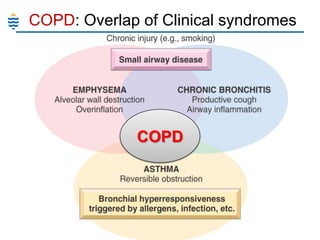
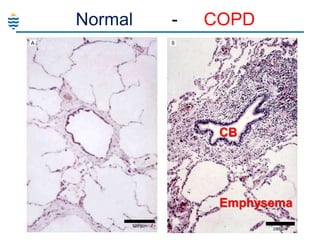
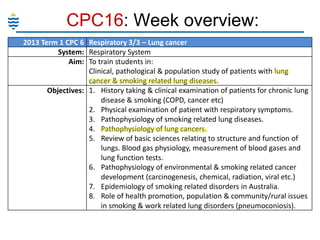
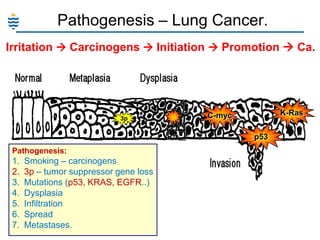
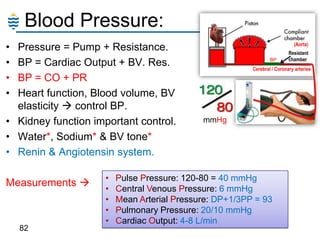
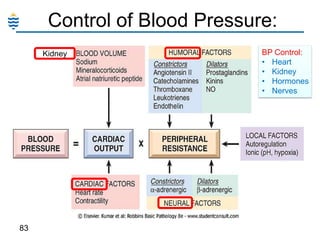
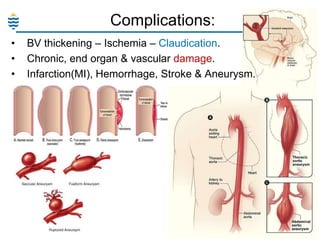
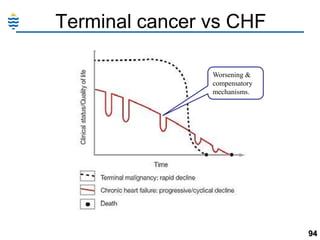
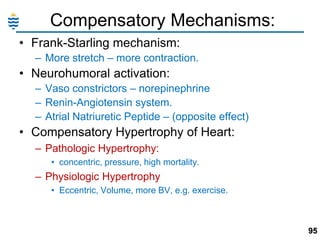
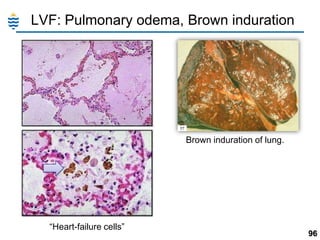
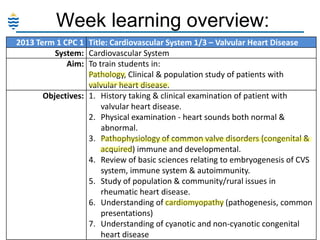
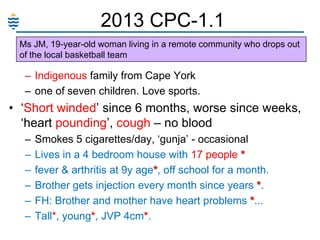
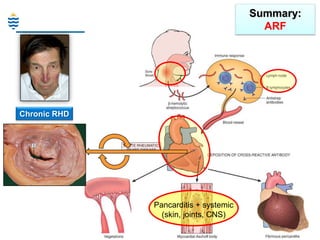
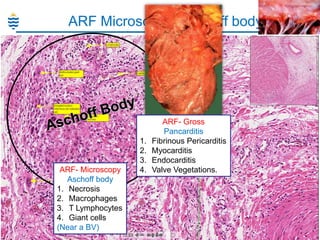
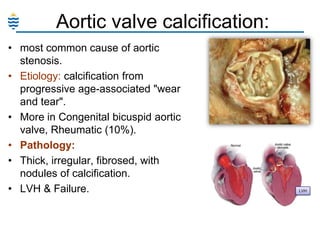
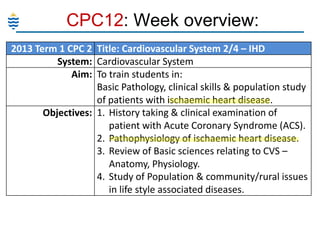
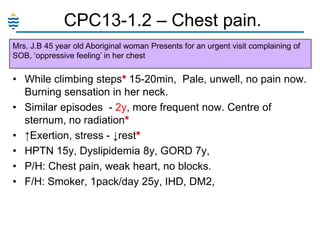
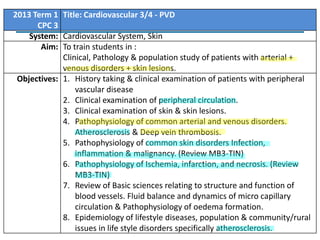
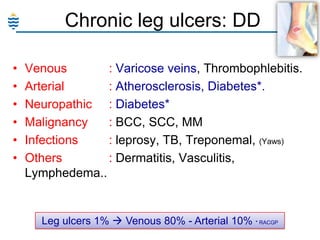
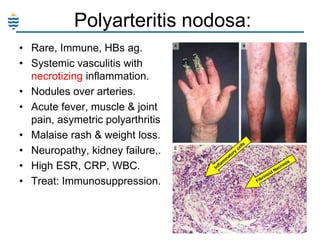
The document outlines a comprehensive training curriculum for medical students focusing on the cardiovascular and respiratory systems, covering conditions such as valvular heart disease, ischemic heart disease, pneumonia, and various types of vascular disorders. Key objectives include history taking, clinical examination, pathophysiology, and community health issues related to these conditions. Detailed case studies and pathophysiology insights provide a framework for understanding common diseases, risk factors, and clinical correlations.
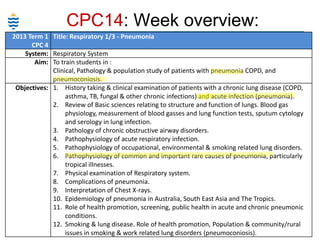
![CPC15: Week overview:
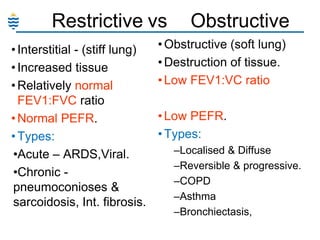
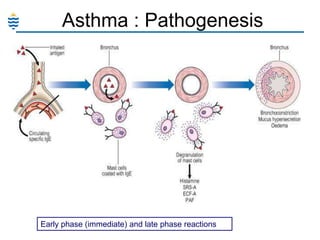
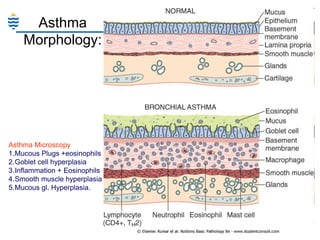
2013 Term 1 CPC 5 Title: Respiratory 2/2 - Asthma & COPD
System: Respiratory System
Aim: To train students in :
Clinical, Pathology and Population studies of patients with
Upper Airway Disease Processes. Asthma, Chronic Cough,
Emphysema, COPD, Chronic Bronchitis and Acute
Bronchitis. [Epiglottitis, Croup]
Objectives: 1. History taking & clinical examination of patients with
obstructive airway disease, upper airway disease.
2. Physical examination of Respiratory system.
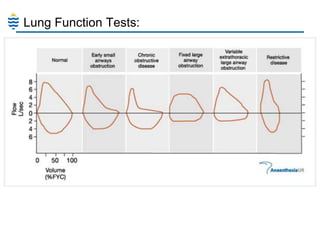
3. Review of Basic sciences relating to structure and
function of lungs. Blood gas physiology, measurement
of blood gasses and lung function tests,
4. Pathophysiology of acute upper airway injury.](https://image.slidesharecdn.com/mb4-yearreview-term1-131110212733-phpapp01/85/Pathology-Review-Term1-55-320.jpg)