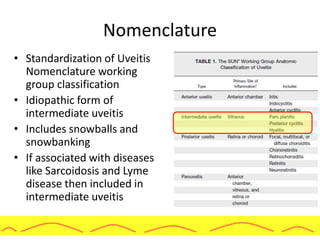
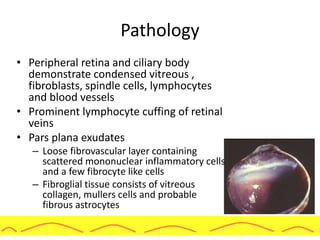
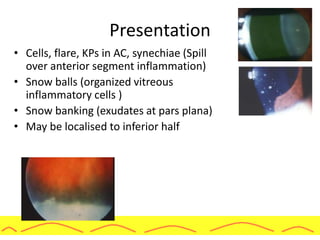
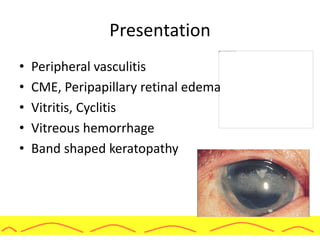
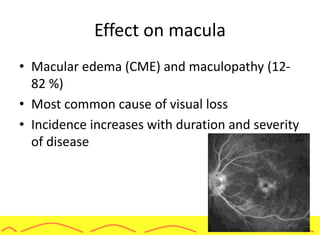
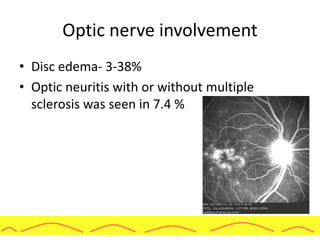
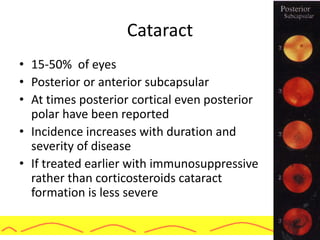
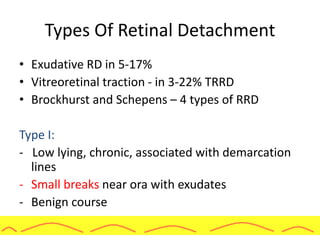
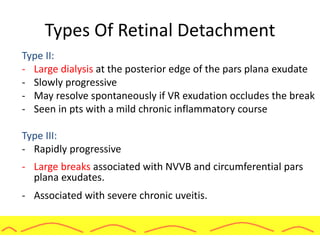
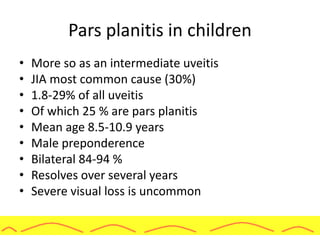
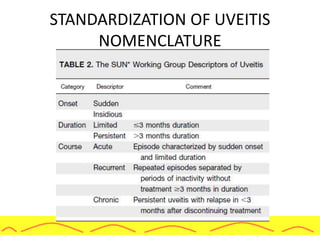
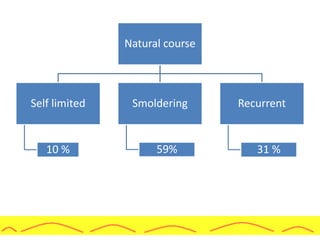
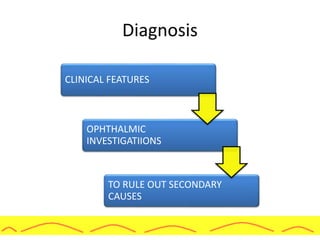
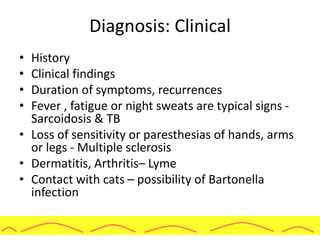
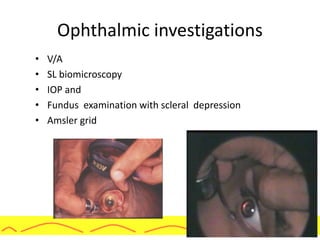
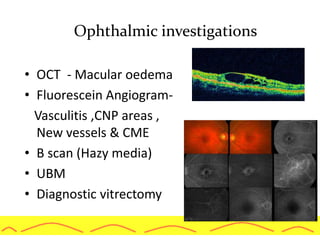
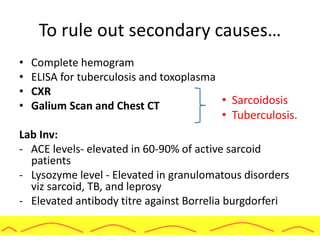
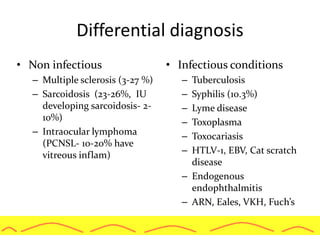
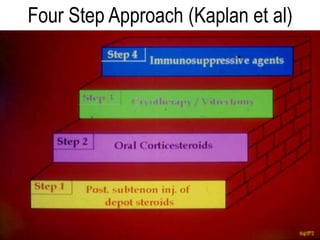
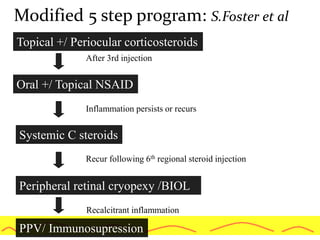
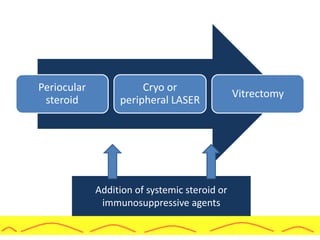
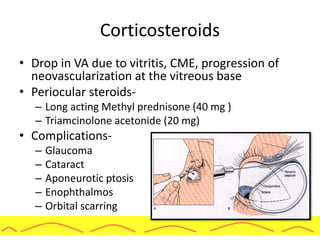
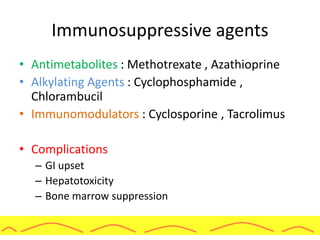
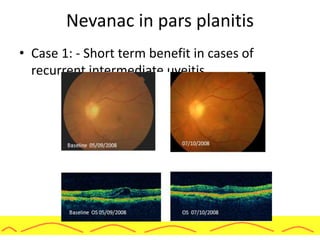
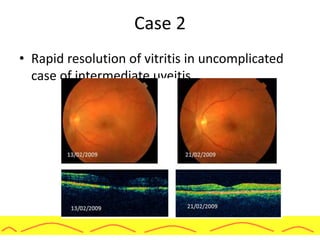
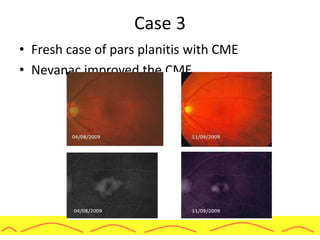
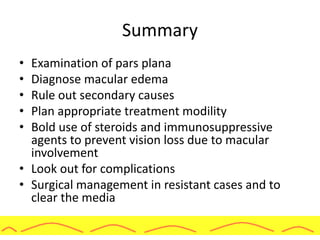
The document discusses pars planitis, a type of intermediate uveitis characterized by various clinical features including vision loss and associated complications. It outlines the history, etiology, pathogenesis, clinical presentation, diagnosis, and management of this condition, emphasizing the role of corticosteroids and immunosuppressive agents. Additionally, it touches upon the epidemiology, risk factors, and specific management strategies for both adults and children affected by pars planitis.