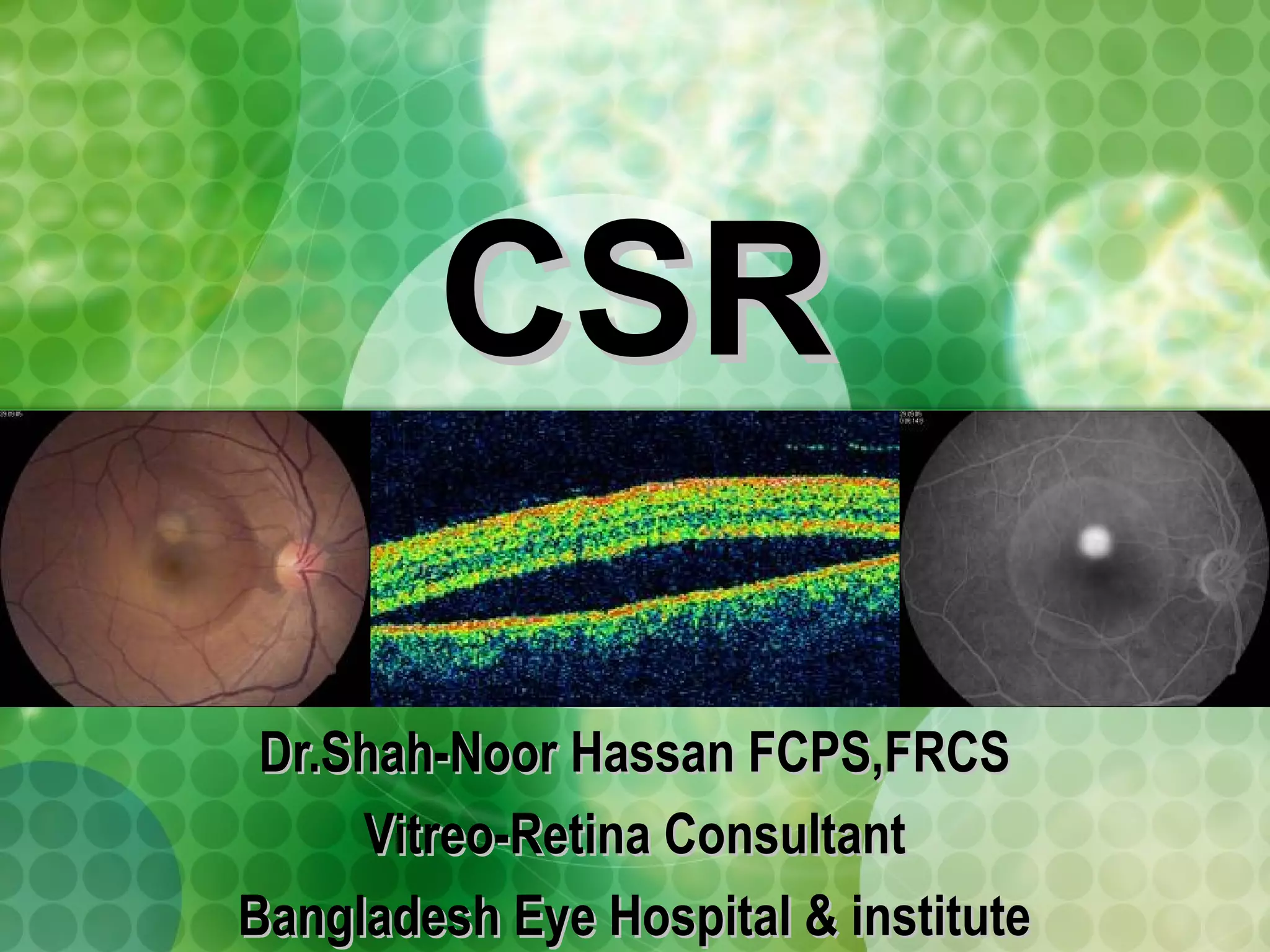
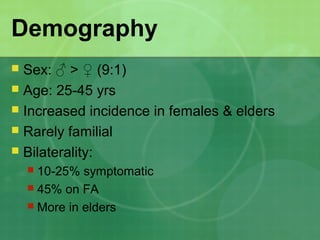
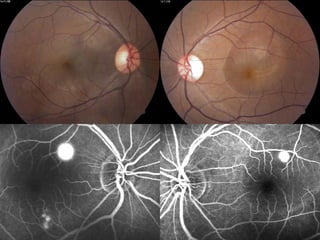
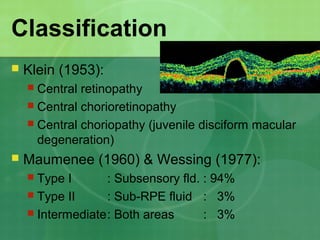
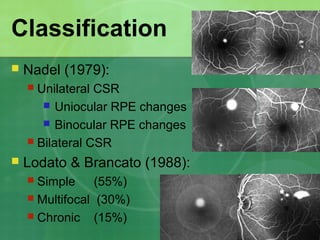
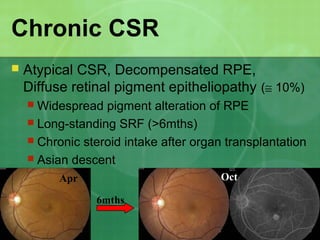
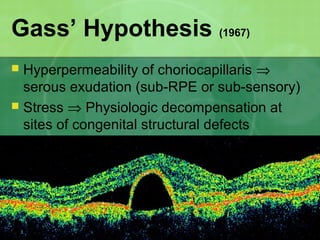
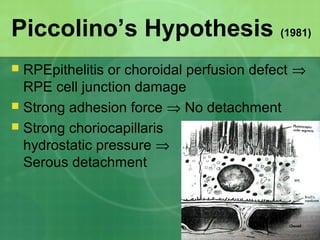
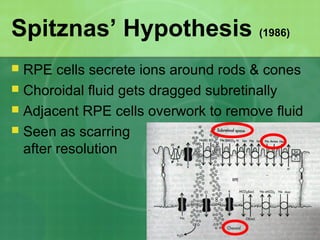
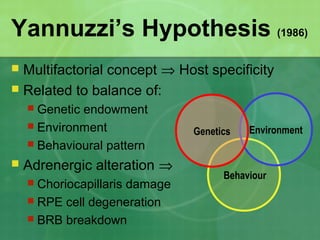
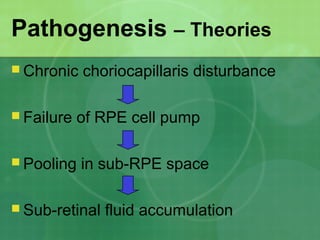
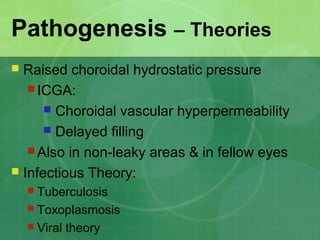
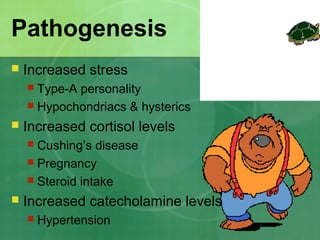
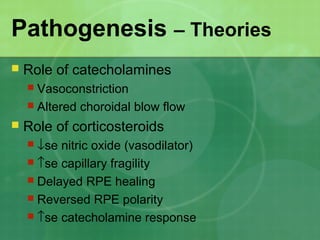
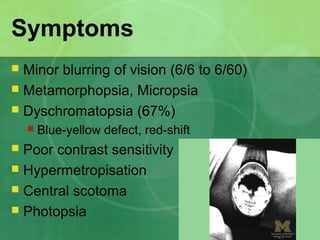
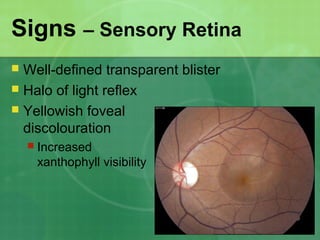
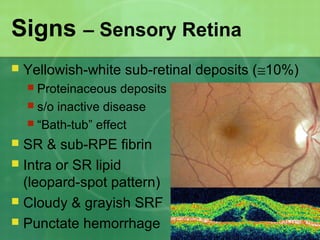
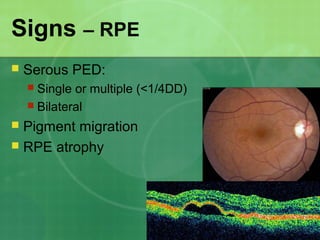
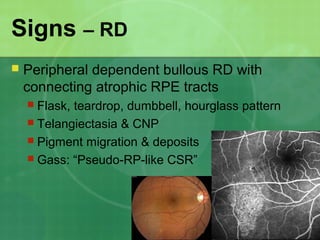
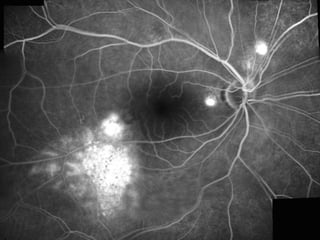
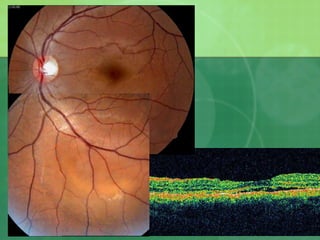
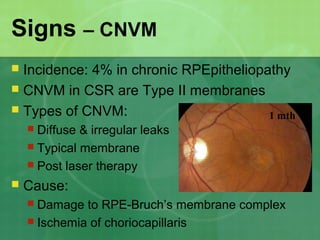
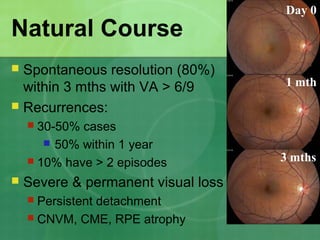
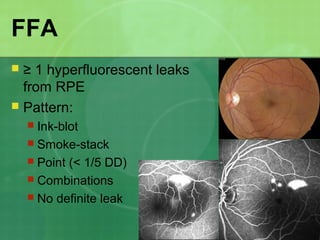
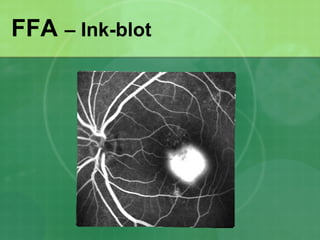
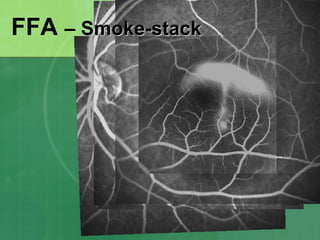
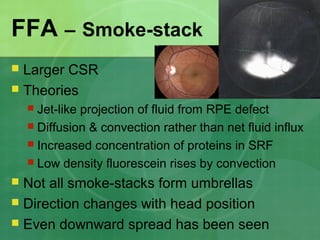
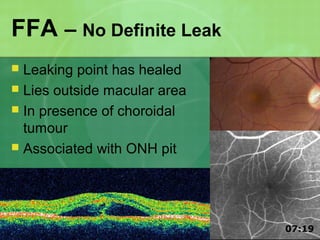
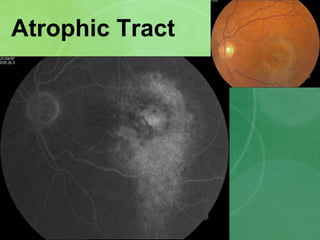
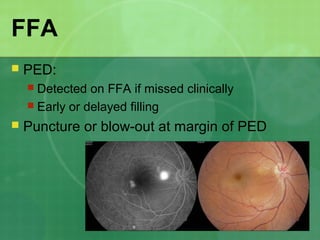
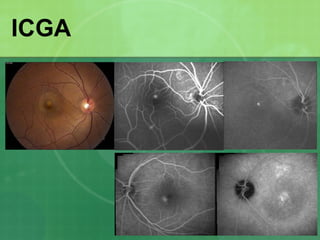
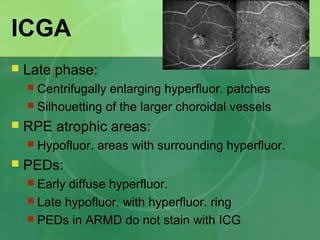
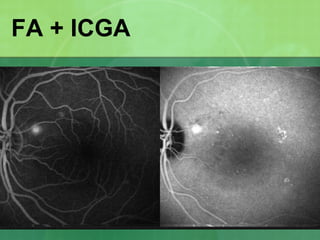
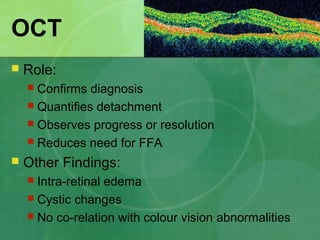
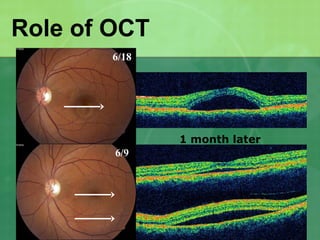
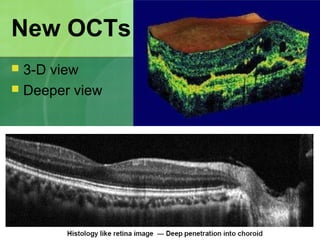
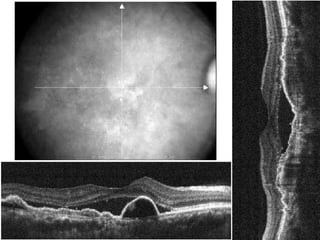
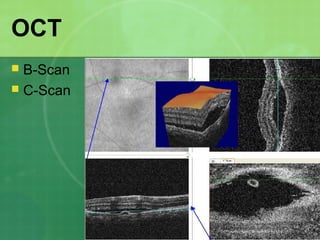
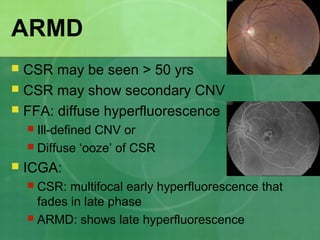
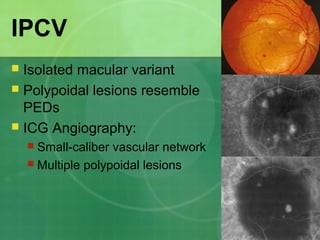
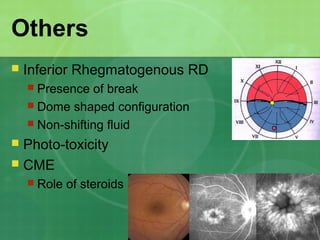
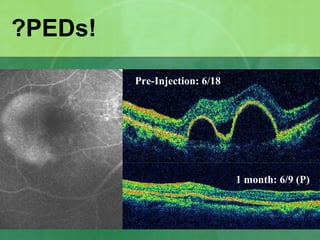
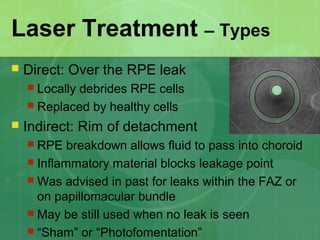
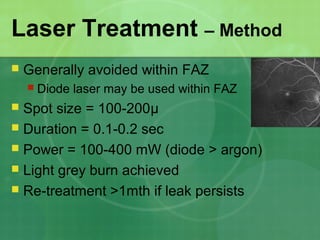
Central serous chorioretinopathy (CSC) is characterized by a collection of fluid at the posterior pole of the eye, causing a localized neurosensory retinal detachment. It typically affects young-to-middle aged males and presents with mild-to-moderate vision loss. The cause is believed to be a defect in the retinal pigment epithelium and choroidal vasculature that allows fluid to accumulate subretinally. Imaging such as fluorescein angiography and optical coherence tomography are useful for diagnosis and monitoring the condition. While often self-limiting, CSC can become chronic in some cases and lead to complications if not properly managed.