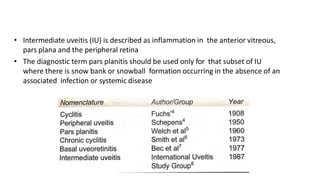
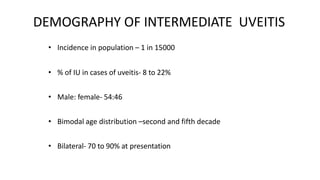
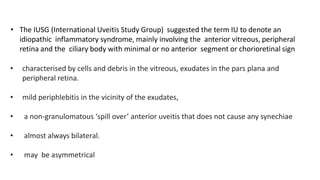
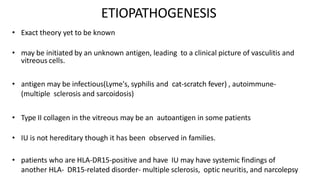
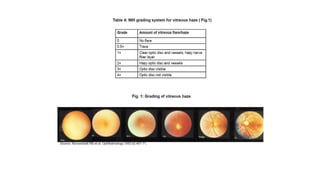
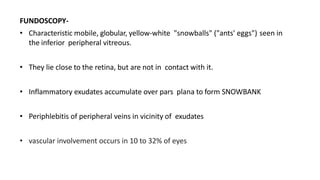
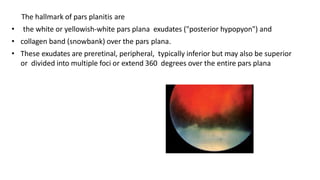
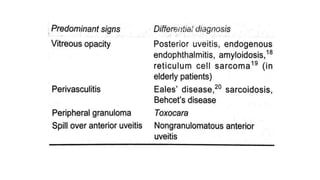
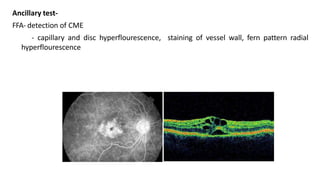
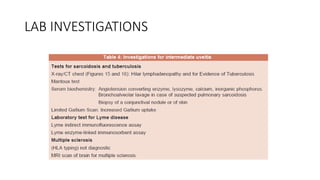
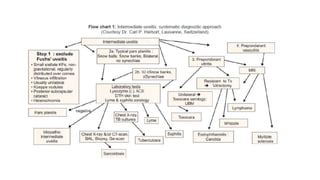
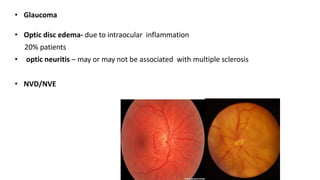
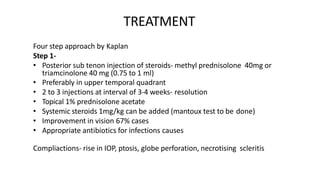
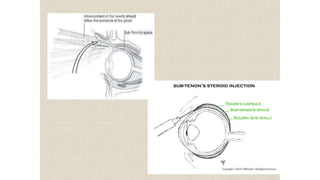
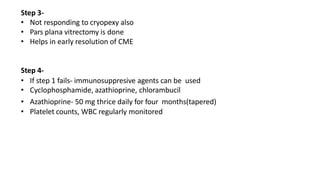
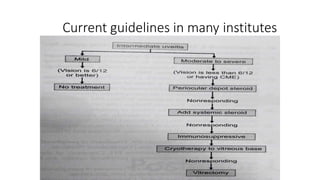
Intermediate uveitis (IU) is an idiopathic inflammatory syndrome involving the anterior vitreous, peripheral retina, and ciliary body, characterized by vitreous cells and debris, pars plana exudates, and mild periphlebitis. The hallmark findings are white or yellowish exudates ("snowballs" or "snowbank") in the pars plana region. Treatment involves a stepwise approach starting with periocular or systemic corticosteroids, then cryotherapy or laser, vitrectomy if needed, and finally immunosuppressants. Complications can include cystoid macular edema, cataracts, glaucoma, and retinal detachment if left untreated. Dif