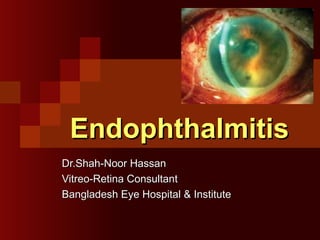
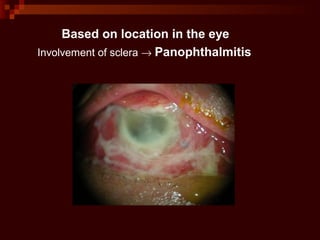
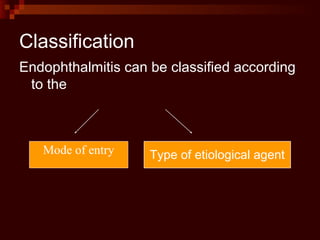
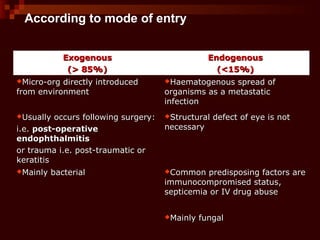
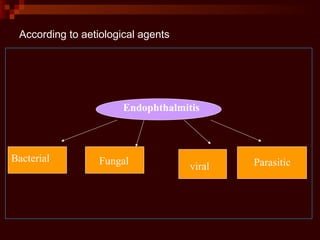
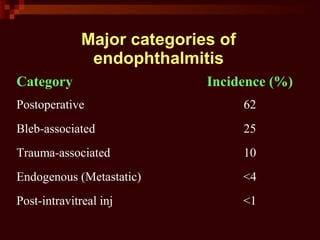
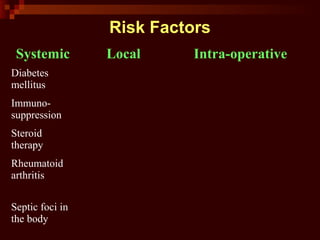
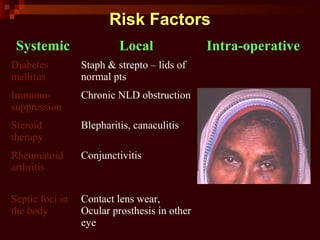
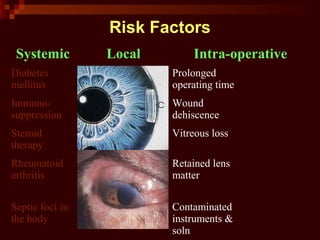
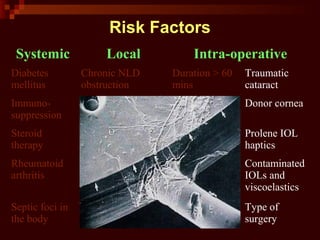
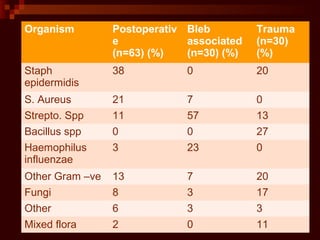
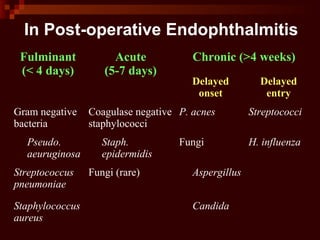
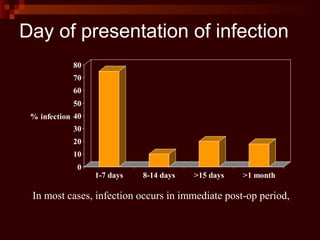
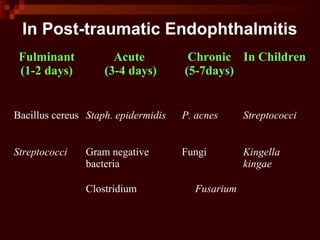
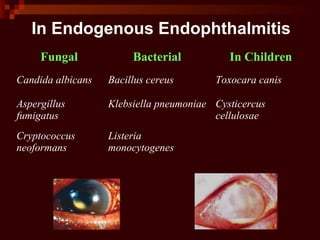
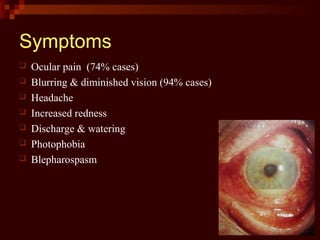
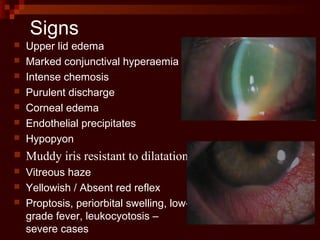
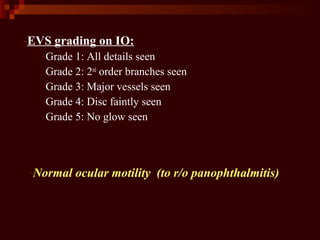
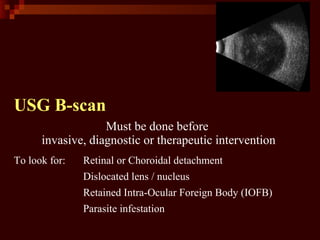
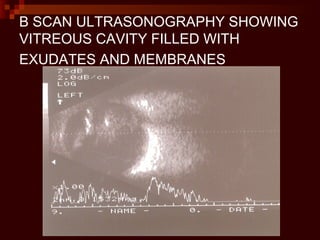
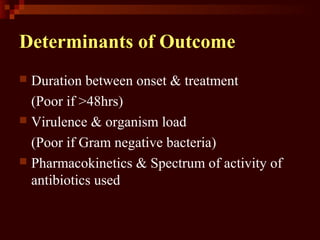
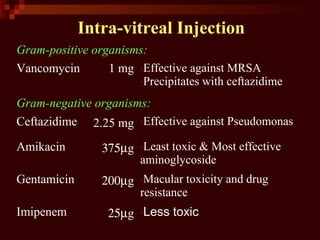
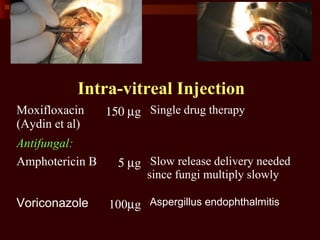
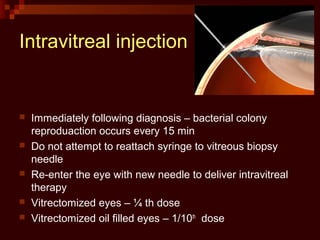
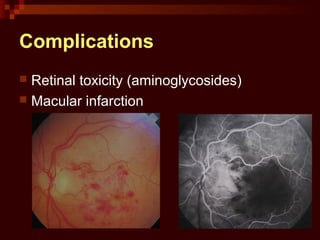
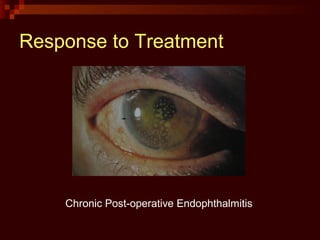
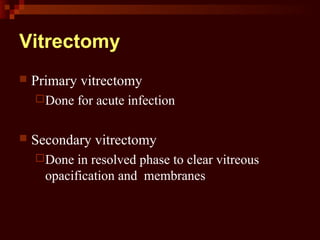
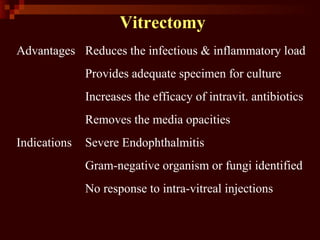
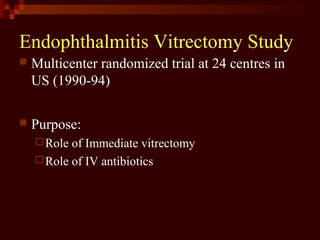
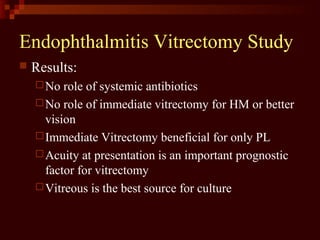
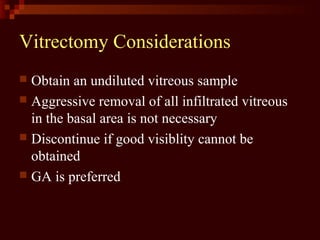
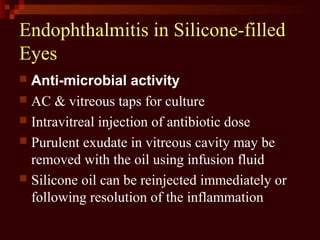
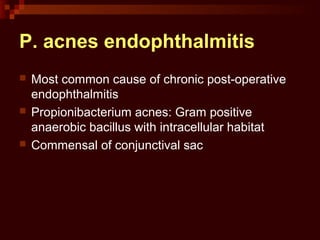
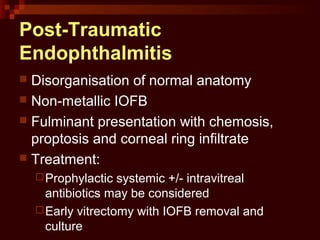
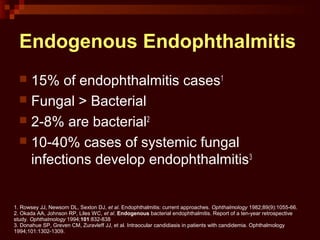
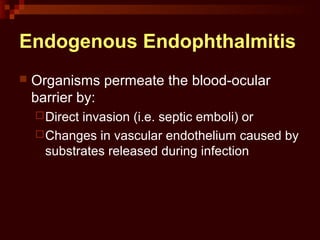
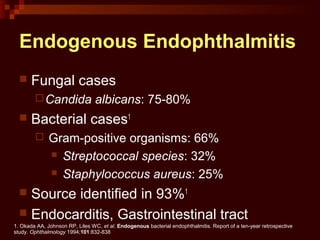
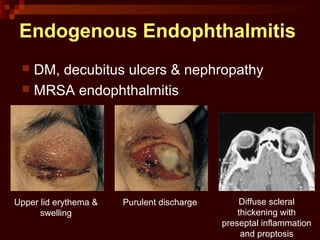
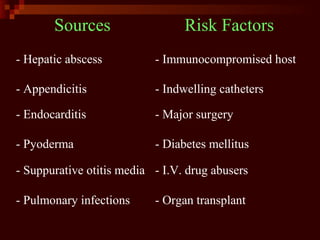
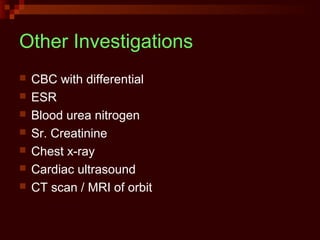
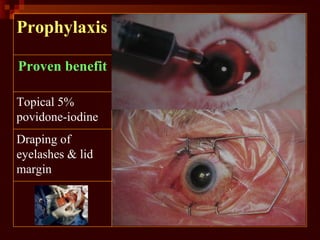
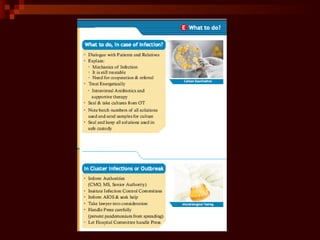
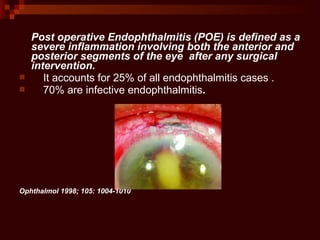
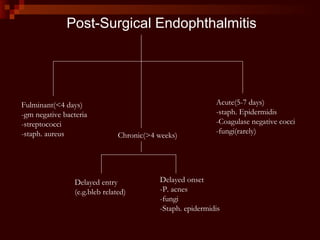
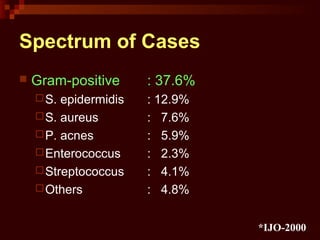
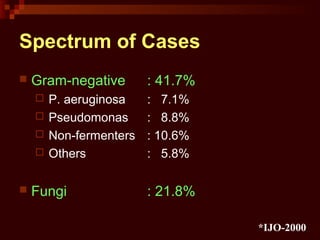
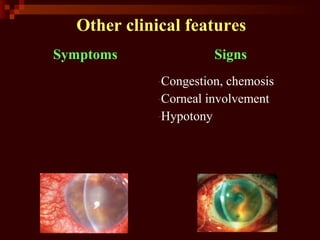
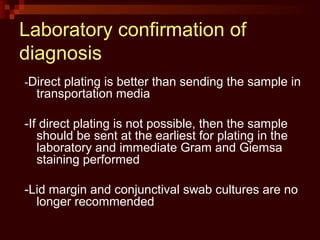
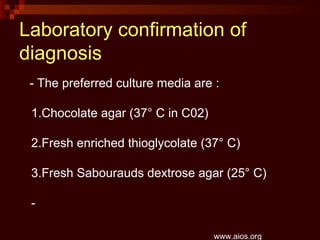
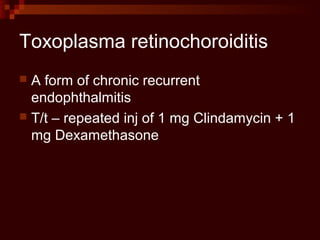
Endophthalmitis is defined as inflammation of the vitreous and inner eye coats, often classified as exogenous (common post-surgery) or endogenous due to hematogenous spread. The document outlines various risk factors, clinical features, diagnostic methods, and treatment modalities, emphasizing the importance of early intervention to prevent complications. It also discusses specific types of endophthalmitis, including post-operative and traumatic cases, along with differential diagnoses and management strategies.