This document provides an overview of sarcoidosis, with a focus on its ocular manifestations and diagnosis. Some key points:
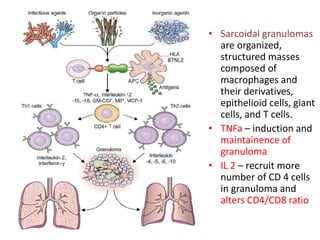
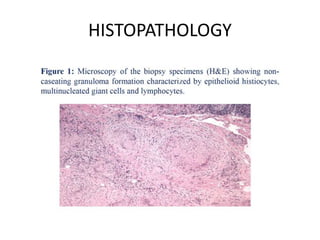
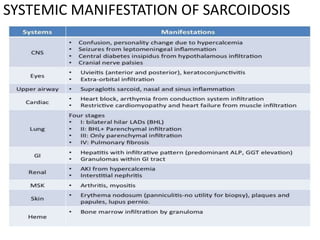
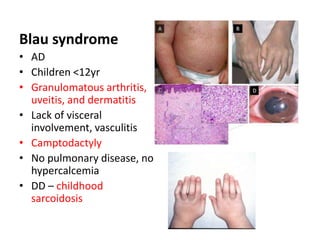
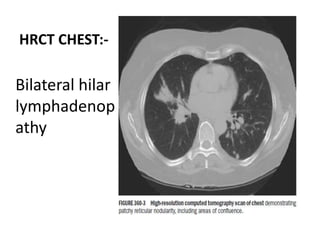
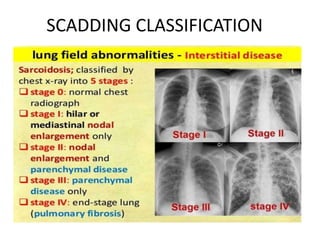
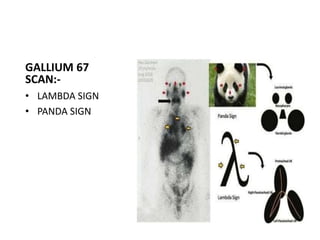
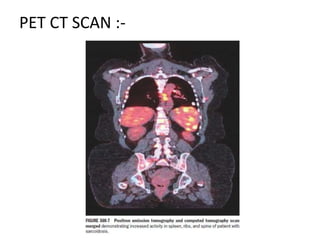
- Sarcoidosis is a chronic inflammatory disease characterized by non-caseating granulomas that commonly affect the lungs, lymph nodes, eyes, and skin.
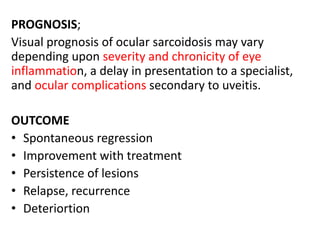
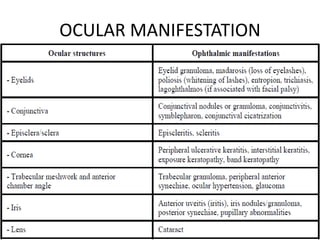
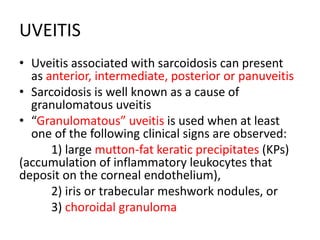
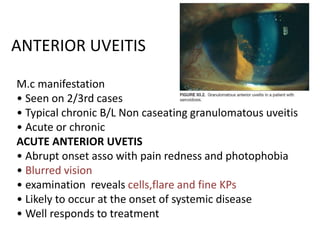
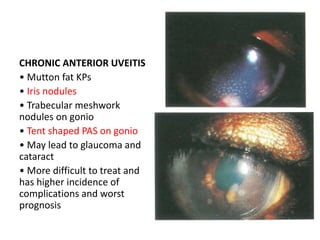
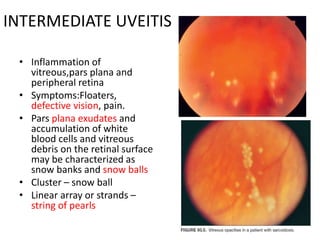
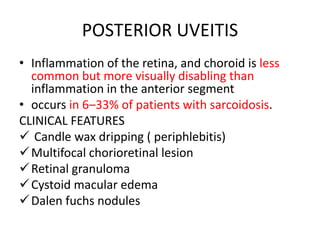
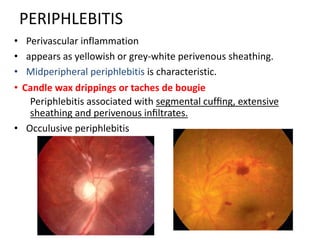
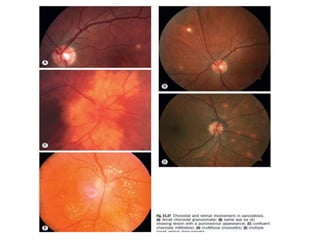
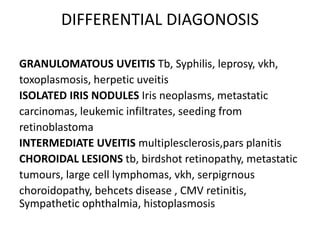
- Ocular involvement occurs in 40% of sarcoidosis patients, usually presenting as chronic, bilateral granulomatous uveitis. This can manifest as anterior uveitis, intermediate uveitis, posterior uveitis, or a combination.
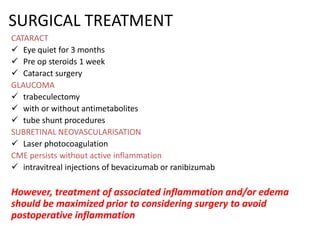
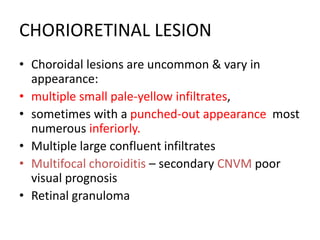
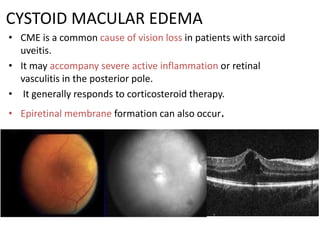
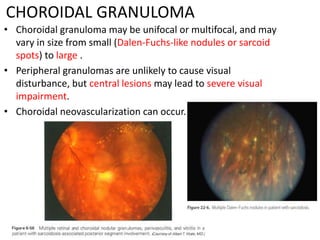
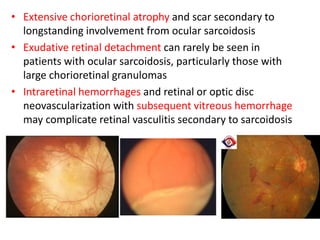
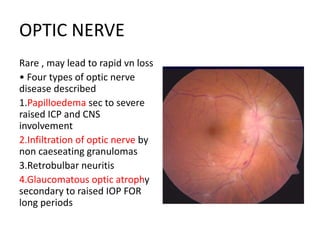
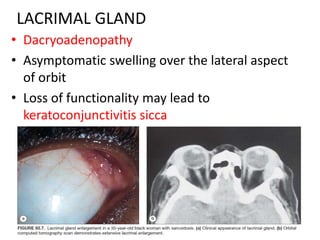
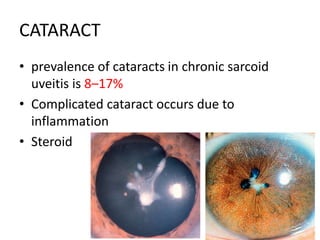
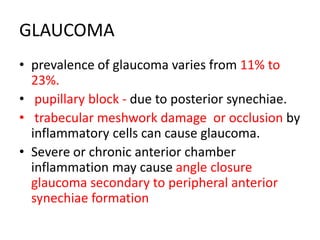
- Complications of ocular sarcoidosis include glaucoma, cataracts, cystoid macular edema, choroidal granulo
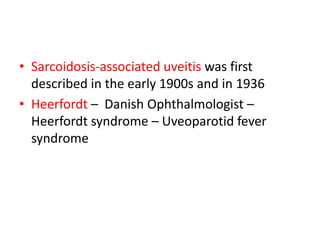
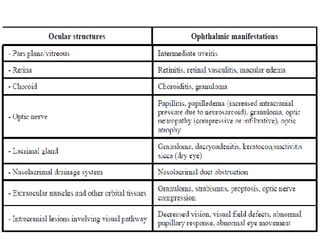

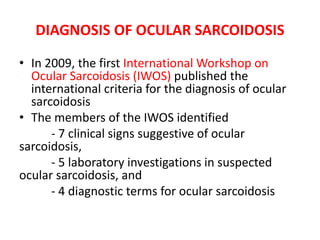
![• Br J Ophthalmol. 2019 Feb 23. pii: bjophthalmol-2018-313356. doi:
10.1136/bjophthalmol-2018-313356. [Epub ahead of print]
• Revised criteria of International Workshop on Ocular Sarcoidosis (IWOS)
for the diagnosis of ocular sarcoidosis
Results The survey and subsequent workshop reached
consensus agreements of the revised criteria for the
diagnosis of OS as follows:
(1) other causes of granulomatous uveitis must be ruled
out;
(2) seven intraocular clinical signs suggestive of OS;
(3) eight results of systemic investigations in suspected
OS and
(4) three categories of diagnostic criteria depending on
biopsy results and combination of intraocular signs and
results of systemic investigations.](https://image.slidesharecdn.com/sarcoidosis-190903151724/85/Sarcoidosis-52-320.jpg)