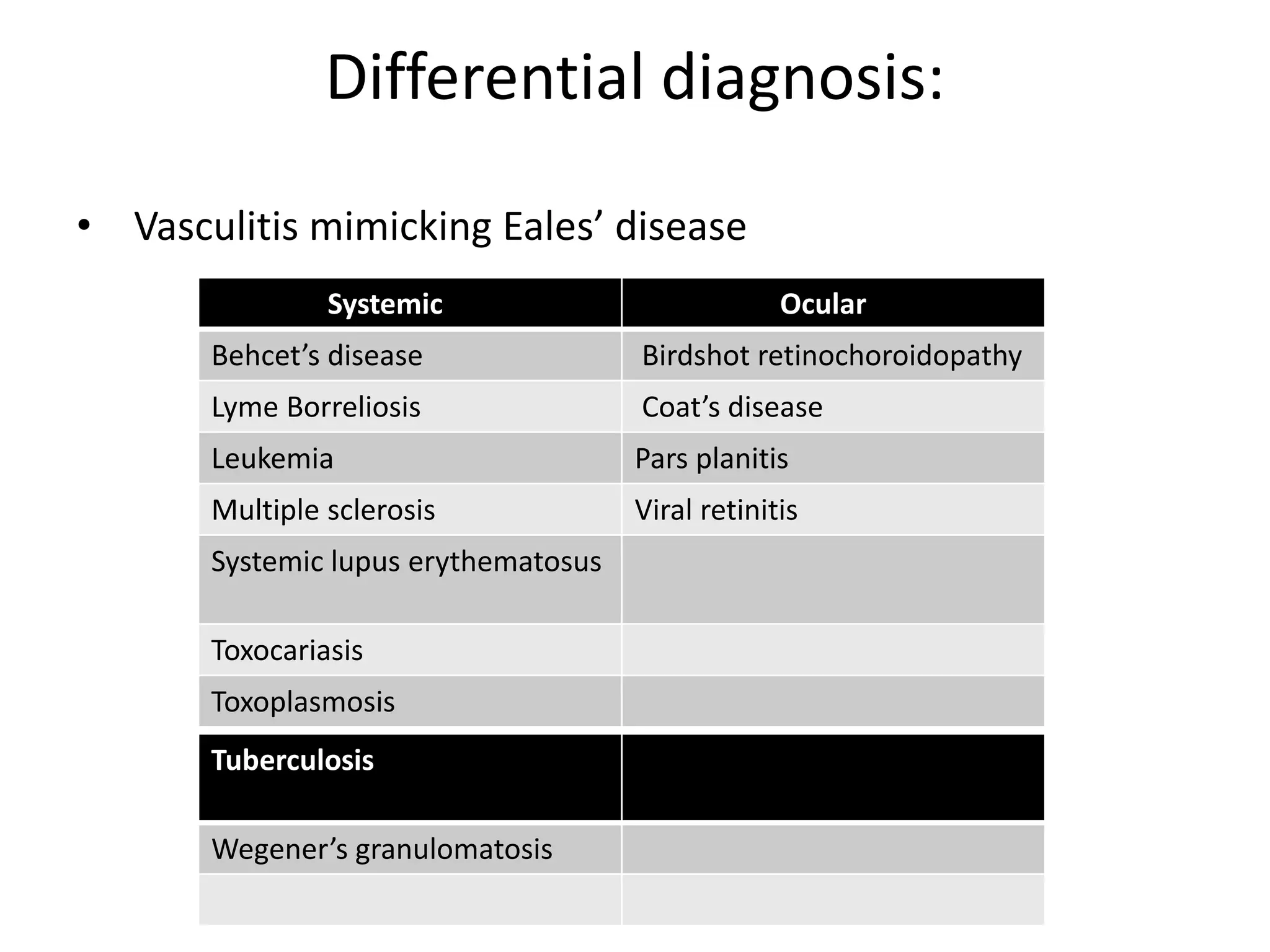
Eales disease is an idiopathic inflammatory retinal condition characterized by peripheral retinal vasculitis and neovascularization. It primarily affects young males in India and presents with recurrent vitreous hemorrhage. The etiology is unclear but may involve hypersensitivity to tuberculosis. Treatment involves corticosteroids for active vasculitis, laser photocoagulation for neovascularization, and vitrectomy for non-resolving hemorrhage or retinal detachment. While the disease course can be prolonged with vision loss, appropriate medical and surgical management provides satisfactory outcomes.