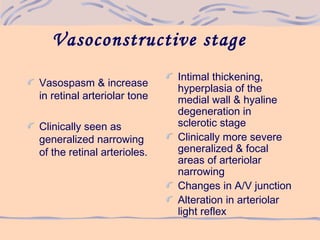
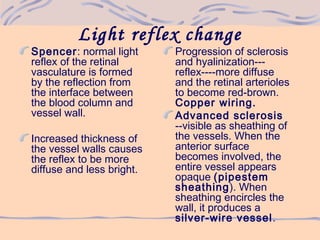
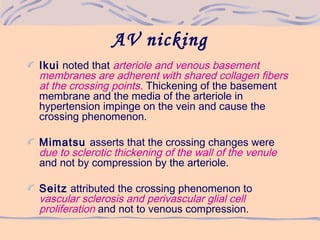
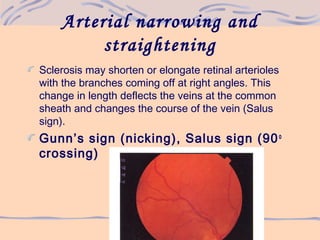
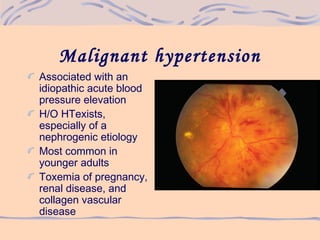
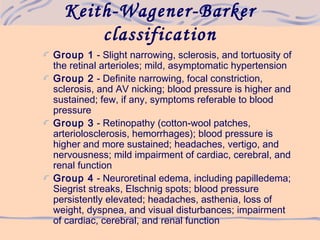
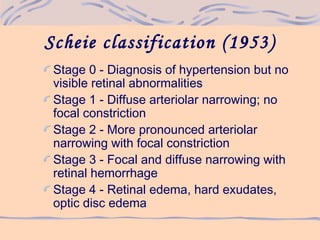
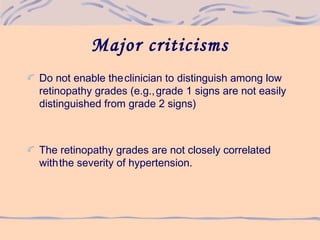
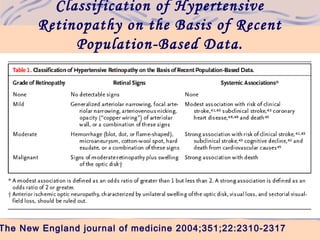
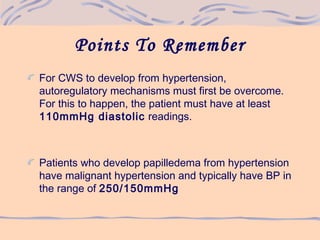
1) Hypertensive retinopathy involves vasoconstrictive and vasospastic responses in the retinal arterioles that can be classified into increasing stages of severity based on observed retinal changes.
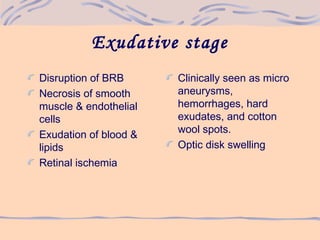
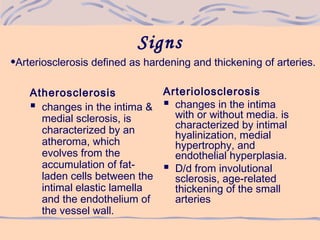
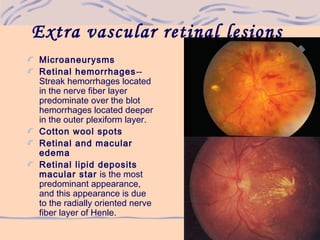
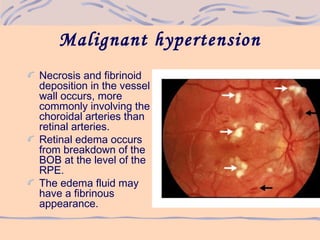
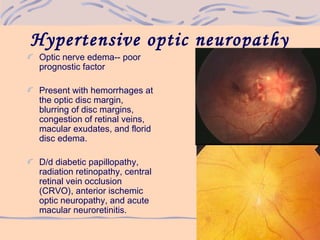
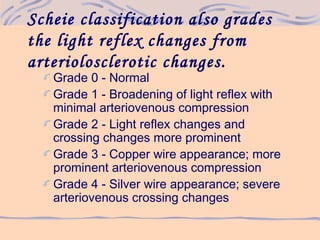
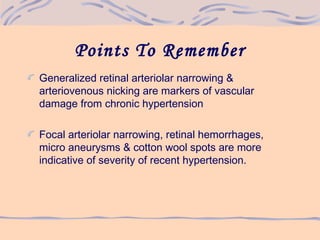
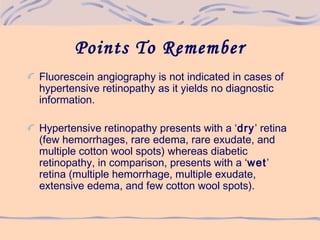
2) As hypertension progresses, it can cause narrowing and sclerosis of retinal arterioles, hemorrhages, exudates, microaneurysms, and cotton wool spots in more severe cases.
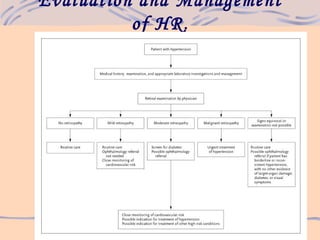
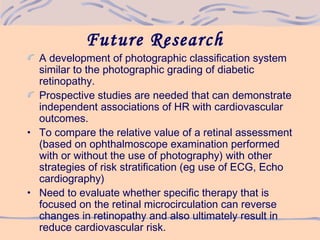
3) Evaluation of hypertensive retinopathy provides insight into the severity of hypertension and risk for end organ damage, with more advanced changes indicating poorly controlled blood pressure that threatens cardiac, cerebral and renal function.