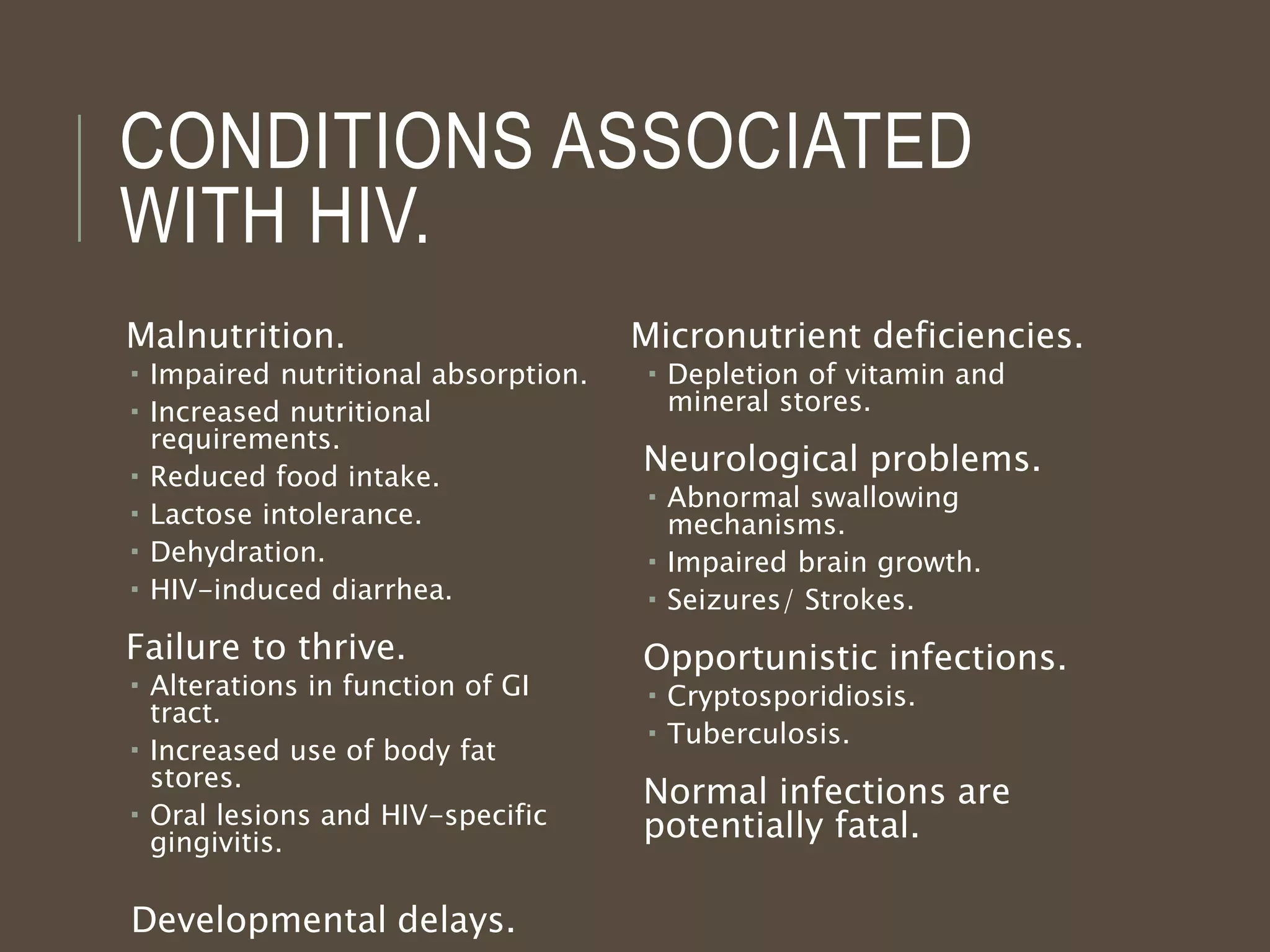
Around 40 million people globally are living with HIV/AIDS, including 3 million children. Without interventions, 35% of infants born to HIV-positive mothers will become infected, with transmission occurring during pregnancy, delivery, and breastfeeding. Proper nutrition management is important for pediatric HIV patients, who may experience malnutrition, opportunistic infections, developmental delays, and other conditions. Aggressive treatment including antiretroviral drugs and management of opportunistic infections can lead to improved outcomes, though the child's nutritional status and viral control are also factors.