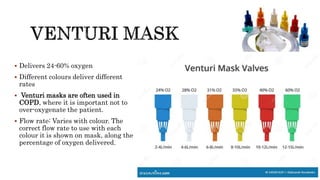
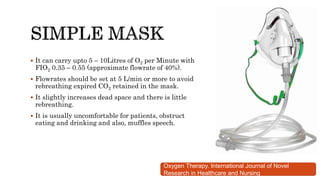
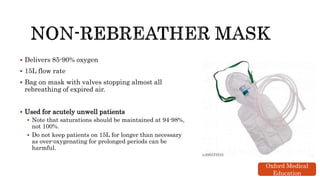
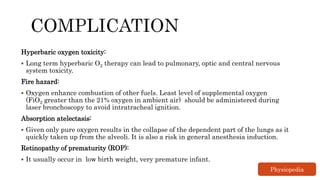
Oxygen therapy, or supplemental oxygen, is a medical treatment used for conditions such as hypoxemia and COPD, delivering oxygen through various methods including low and high flow administration. Acute care employs techniques like CPAP and ventilation for severe cases, while considerations must be made to avoid complications such as over-oxygenation and fire hazards. Proper monitoring and flow rate adjustment are essential to ensure effective treatment without adverse effects.