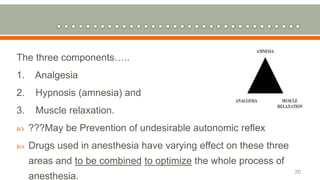
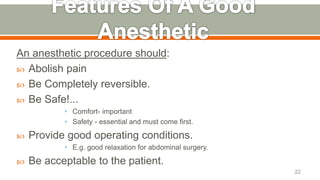
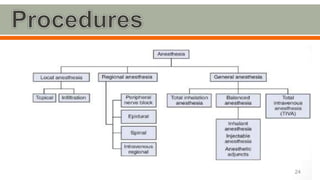
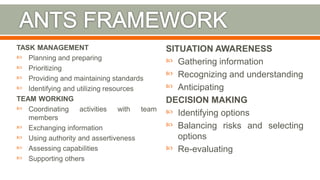
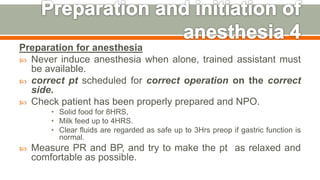
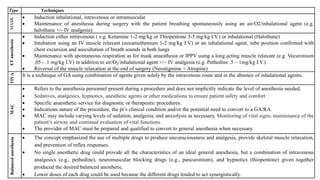
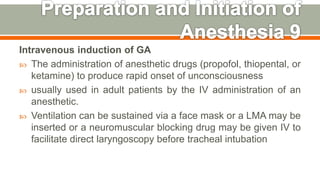
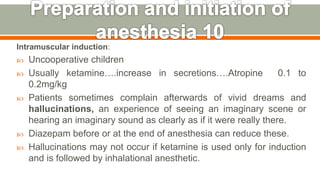
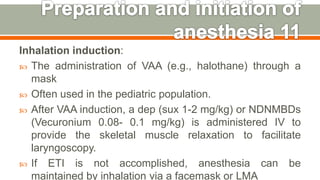
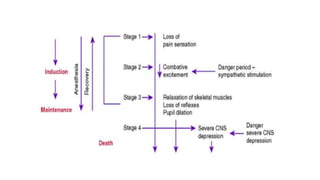
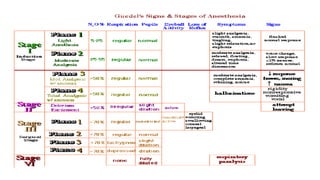
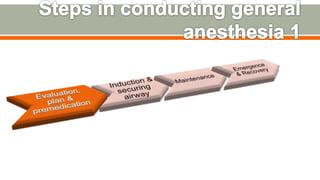
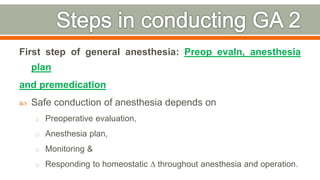
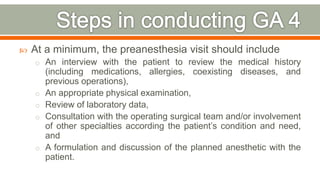
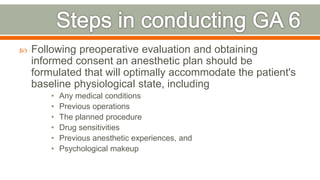
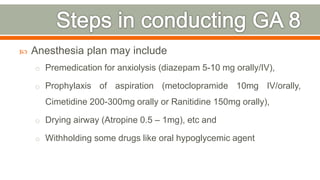
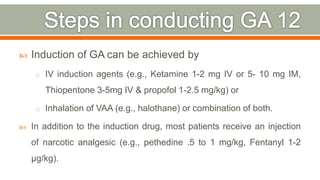
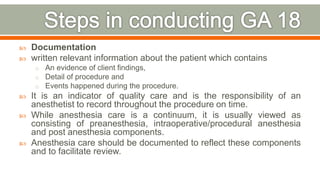
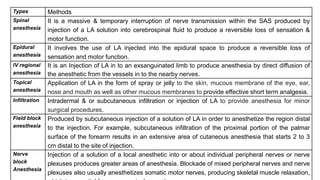
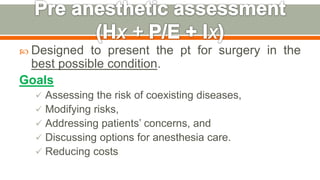
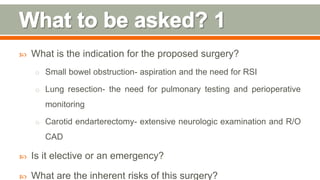
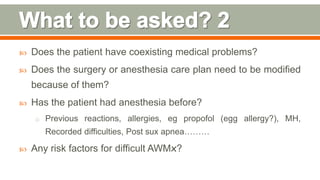
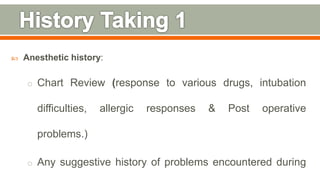
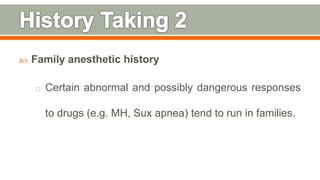
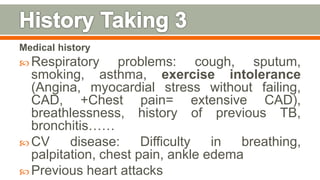
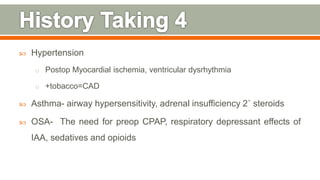
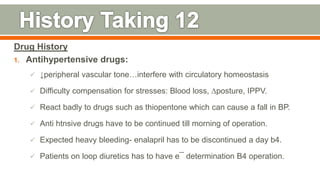
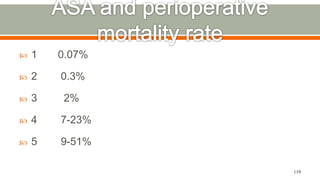
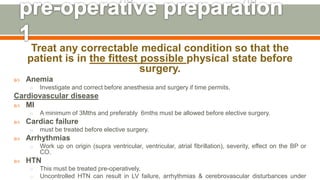
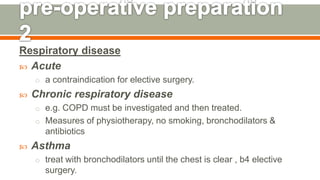
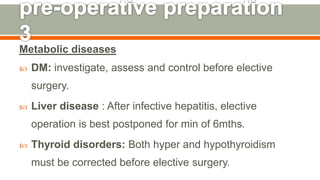
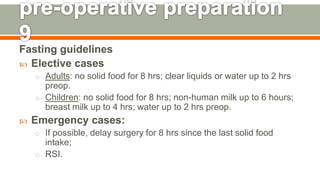
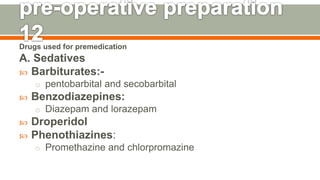
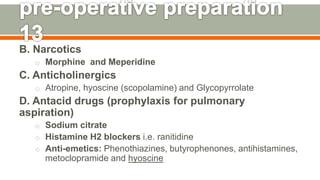
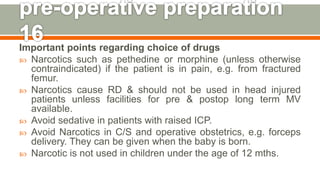
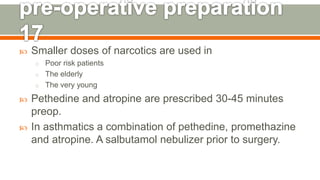
This document discusses the evolution and critical importance of anesthesia in surgical practice, emphasizing the need for anesthetists to have a strong foundation in medical science, physiology, and pharmacology. It details the historical development of various anesthetic agents and techniques, as well as the roles of anesthetists and nurse anesthetists in ensuring patient safety and comfort during procedures. The document also highlights best practices in anesthesia preparation, administration, and monitoring to optimize patient outcomes.