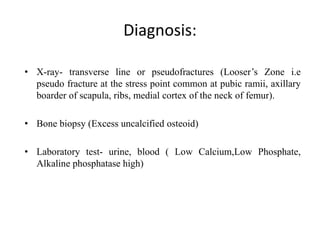
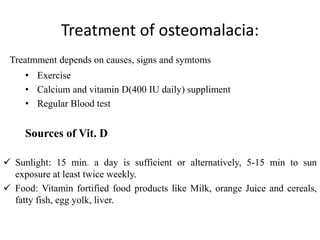
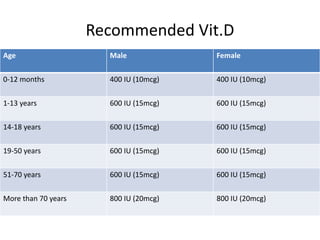
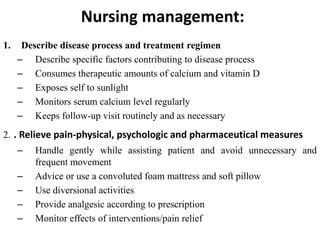
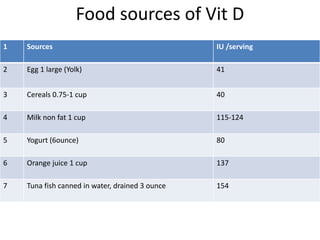
Osteomalacia is a bone condition caused by vitamin D deficiency or impaired mineralization. It results in soft, weakened bones due to incomplete mineralization of bone matrix. Symptoms include bone pain, tenderness, fractures, and muscle weakness. Diagnosis involves x-rays showing pseudofractures and bone biopsy showing excess osteoid tissue. Treatment focuses on calcium and vitamin D supplementation to promote bone mineralization. Nursing care includes education on diet, sunlight exposure, pain management, and monitoring for treatment effectiveness.