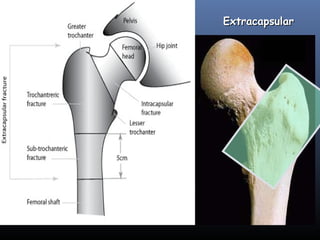
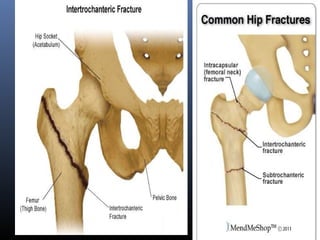
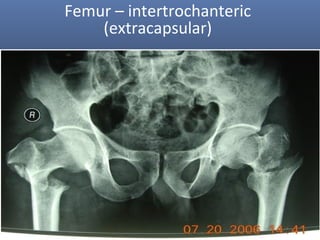
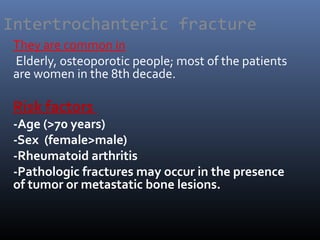
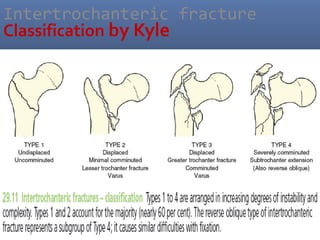
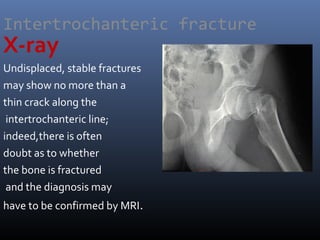
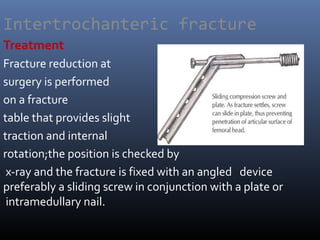
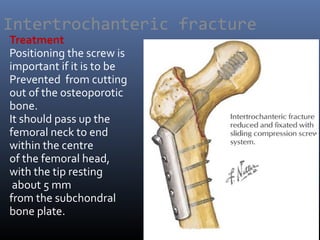
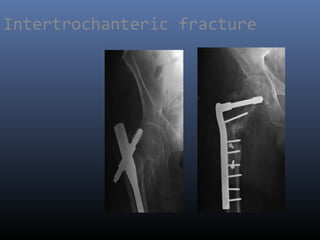
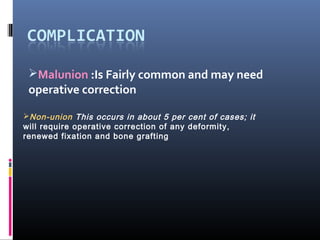
Intertrochanteric fractures are extracapsular femoral fractures common in elderly, especially women, due to falls or twisting injuries, often characterized by pain, inability to stand, and distinct leg positioning. Treatment typically involves early internal fixation to ensure proper positioning and reduce complications, with non-operative care reserved for those too ill for surgery. Complications can include non-union, malunion, and issues arising from postoperative care or implant failures.