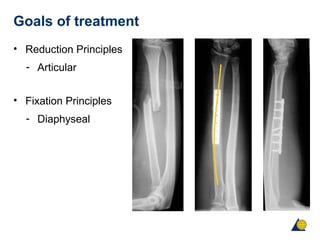
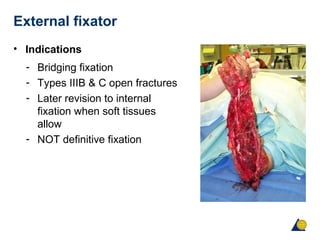
The document discusses fractures of the forearm and their treatment. It summarizes that the forearm functions as a joint with six articulations. Forearm fractures can result in deformities like shortening, angulation, and loss of alignment if not treated properly. Treatment goals are anatomical reduction, restoration of length and rotation, and early return of function. Plate fixation is the gold standard and provides stable fixation, allowing early motion to restore function with high union rates over 95%.