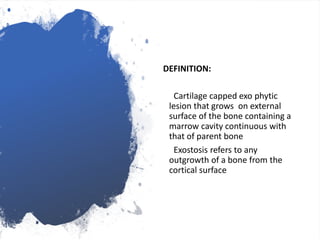
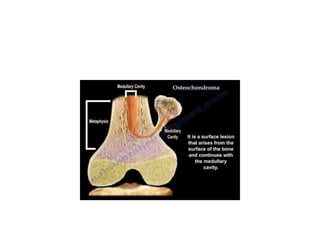
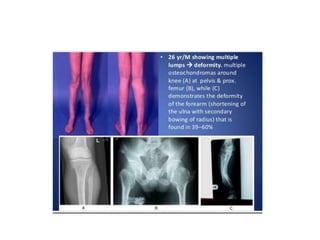
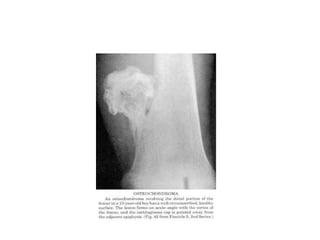
Osteochondroma is a benign bone tumor that presents as a cartilage-capped bony projection on the external surface of bones. It is caused by aberrant growth plate development and is associated with mutations in EXT1 and EXT2 genes. Osteochondroma typically presents in childhood as multiple lesions near joints and can cause deformities. Complications include fractures, bursa formation, arthritis and rare malignant transformation into chondrosarcoma. Diagnosis involves radiology and biopsy. Treatment involves surgery to remove painful or deforming lesions. It has an autosomal dominant inheritance pattern and carriers have a 50% risk of passing the condition to offspring.