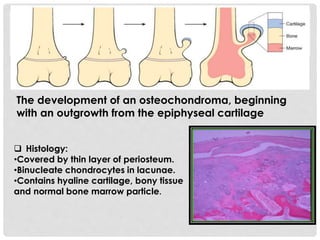
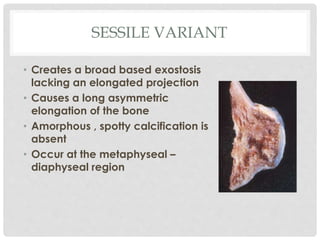
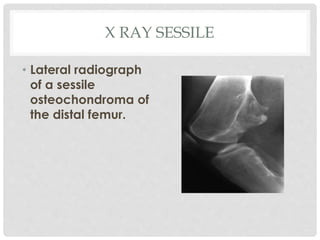
Osteochondroma is a benign bone tumor that projects from the external surface of bones. It consists of a cartilage cap and bony projection. Solitary osteochondroma involves one bone, while multiple osteochondromas can involve several bones and are associated with hereditary multiple exostosis. Osteochondromas are most common in children and adolescents, usually causing no symptoms, though sometimes pain or pressure on nearby tissues. While usually benign, osteochondromas have a small risk of malignant transformation. Diagnosis involves x-ray, CT or MRI to identify the connection to the underlying bone and cartilage cap structure. Symptomatic osteochondromas may require surgical excision to relieve symptoms.