1) Intramedullary nailing has evolved over the past 75 years from early wooden and ivory implants to modern interlocking nails made of titanium.
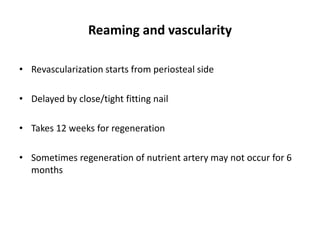
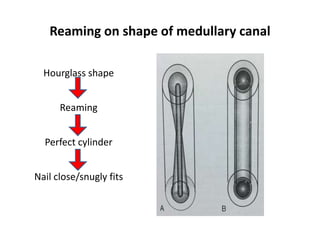
2) Reaming improves nail stability and increases the use of larger nails but also disrupts endosteal blood supply, so newer reamer designs like the Reamer-Irrigator-Aspirator aim to minimize this.
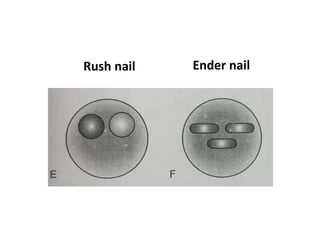
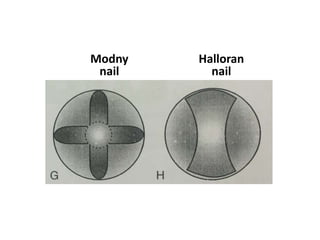
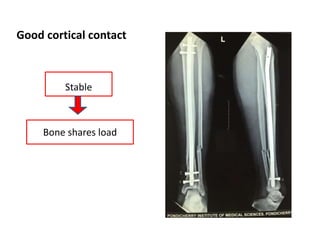
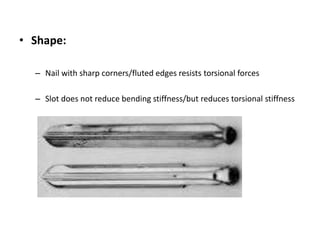
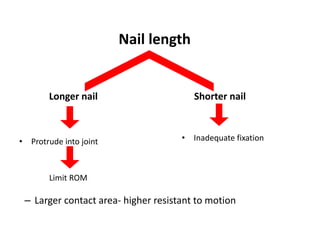
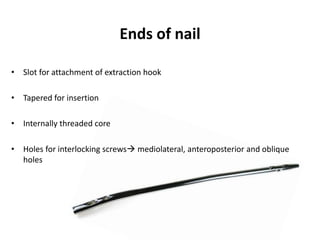
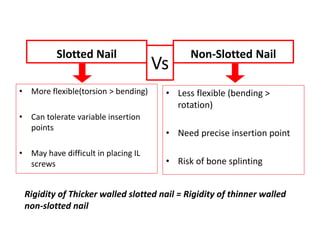
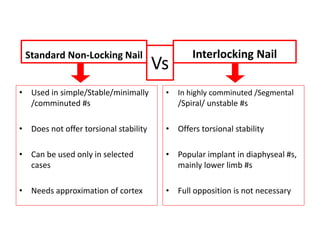
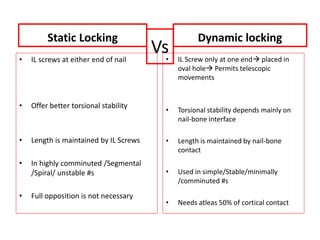
3) Nail characteristics like diameter, length, curvature and interlocking screws influence stability, with larger diameter nails providing greater bending stiffness and interlocking screws enhancing torsional stability.