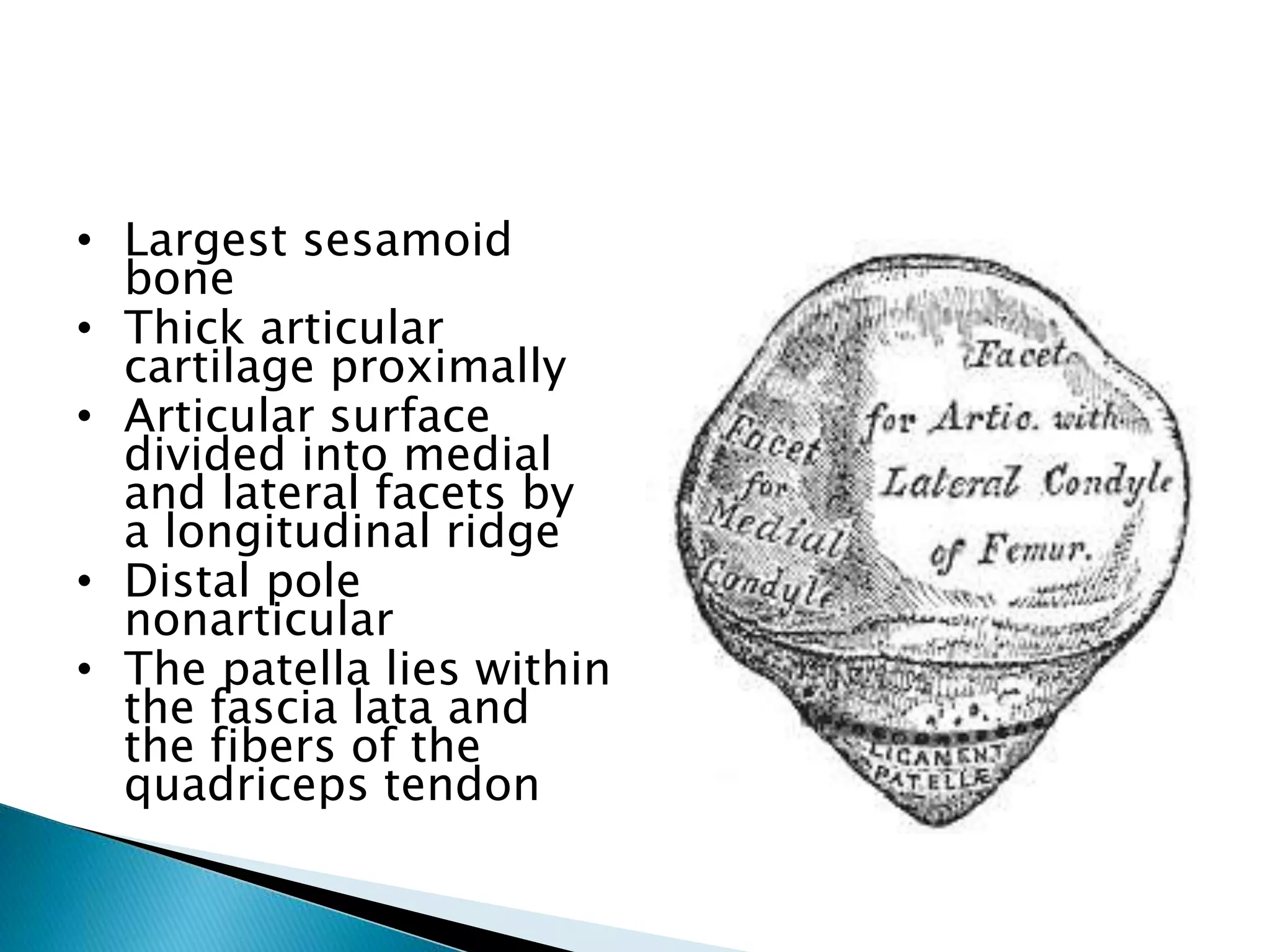
The patella is the largest sesamoid bone in the body located within the quadriceps tendon. It articulates with the femur and is supplied by vessels from the geniculate arterial system. The patellar retinaculum connects the patella to the tibia and is formed by fascia and fibers from surrounding muscles. The patella can displace in various directions from its normal position. Lateral dislocation is most common due to anatomical and biomechanical factors that influence the patellofemoral joint. Evaluation and treatment depends on the nature and chronicity of the injury.