1) Tuberculosis of the knee joint is the third most common site of osteoarticular tuberculosis, accounting for around 10% of skeletal tuberculosis cases.
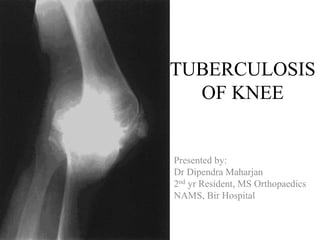
2) Initial pathology involves hematogenous spread to the synovium or subchondral bone, forming tubercles. Advanced cases involve erosion of joint surfaces and destruction of bones.
3) Clinical features include knee swelling, warmth, effusion, tenderness, and restricted painful movement. Advanced cases develop triple deformity of flexion, adduction, and internal rotation.