This document provides an overview of hallux valgus, including its anatomy, causes, symptoms, diagnosis, and treatment options. Key points include:
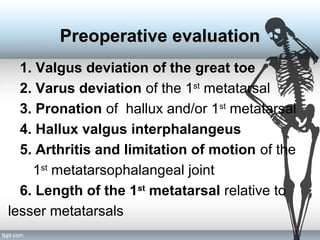
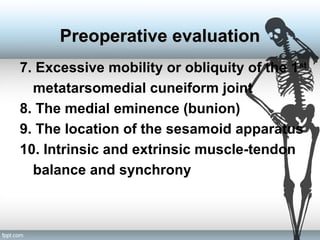
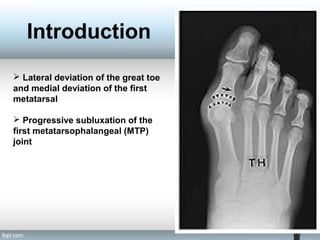
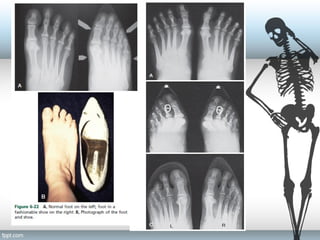
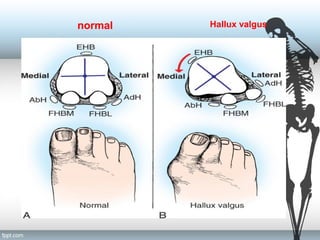
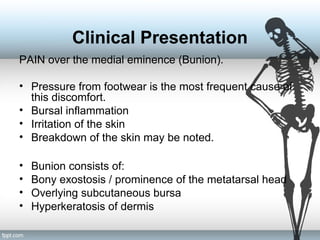
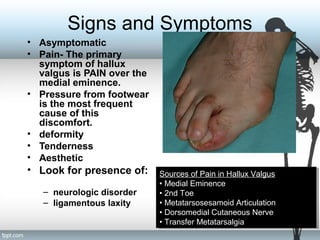
- Hallux valgus is a lateral deviation of the great toe and medial deviation of the first metatarsal. It can cause pain over the bunion.
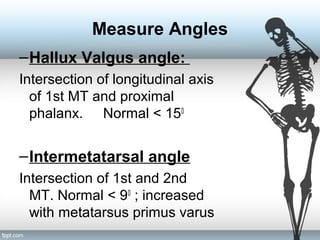
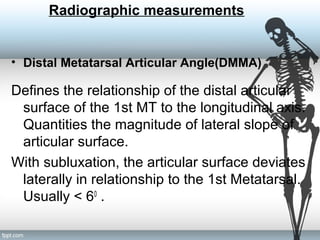
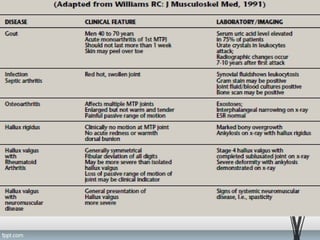
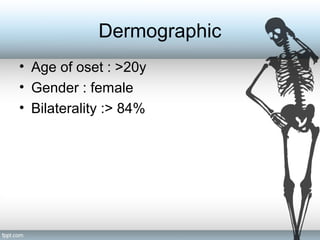
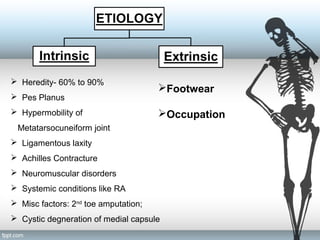
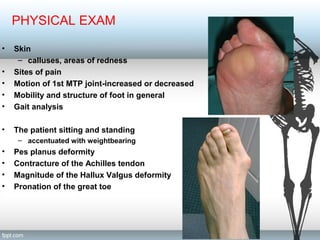
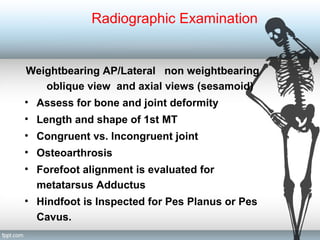
- Risk factors include heredity, footwear, ligament laxity, and pes planus. Diagnosis involves examining range of motion, deformity, and taking x-rays to measure angles.
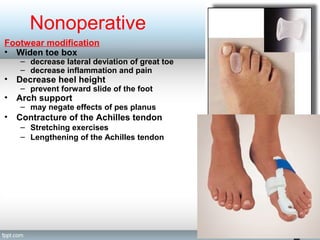
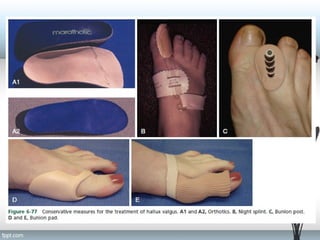
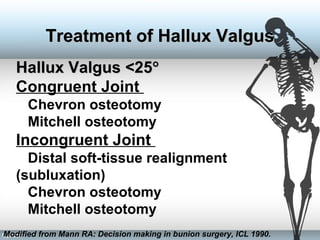
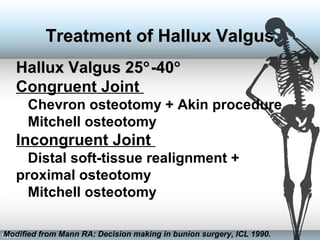
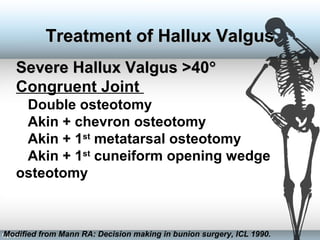
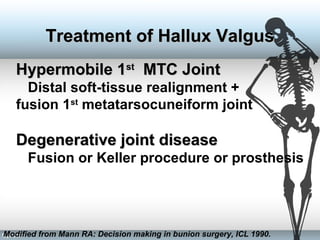
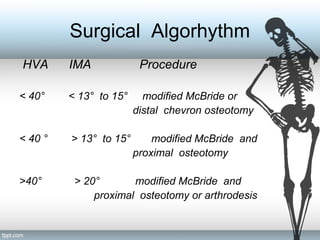
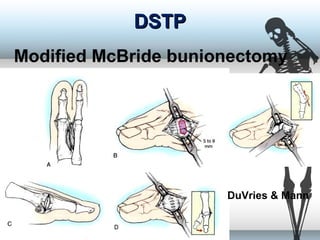
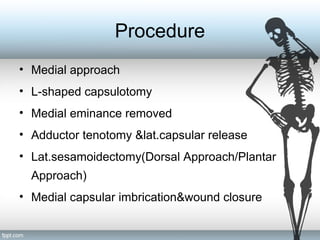
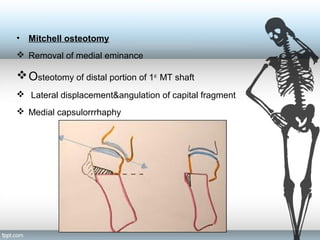
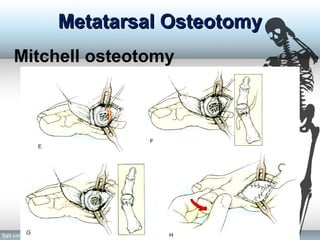
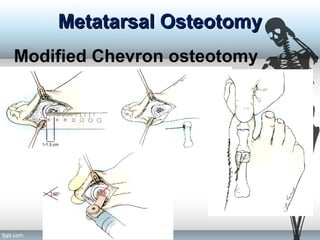
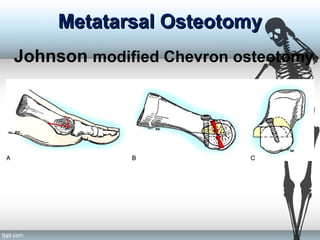
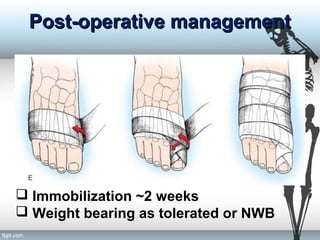
- Treatment progresses from footwear modifications and stretching to various surgical procedures depending on severity, including distal soft tissue procedures, osteotomies, and joint fusion or replacement in severe cases.
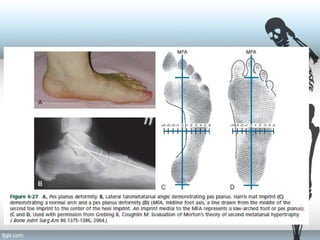
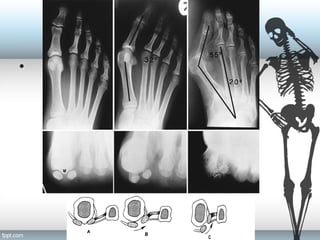

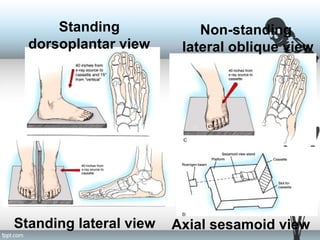
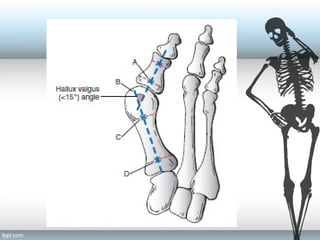
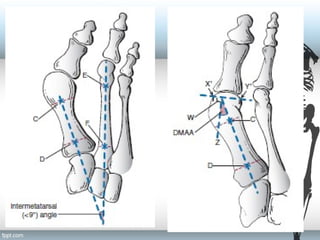
![IMA (normal <9°) [8-9]
HVA (normal <15°) [15-20]
DMAA (normal <10°) [10-15]
Hallux
valgus
angle
Intermetatarsal
angle
Distal
metatarsal
articular
angle](https://image.slidesharecdn.com/halluxvalgus-151218113622/85/Hallux-valgus-pptx-28-320.jpg)