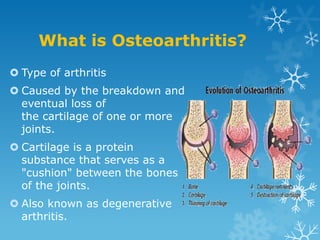
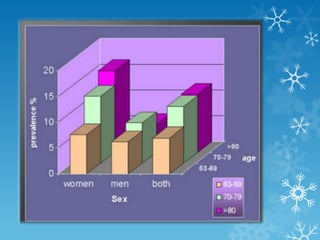
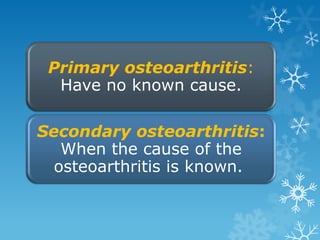
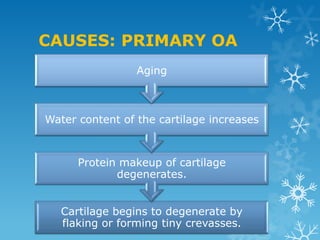
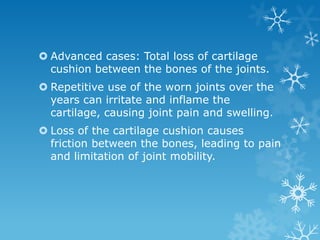
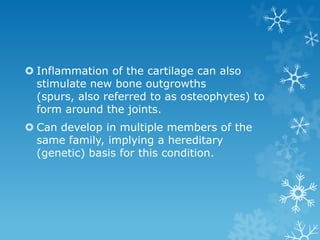
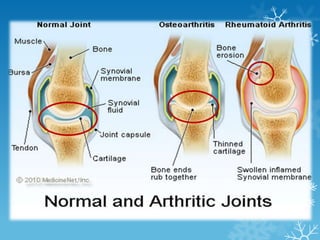
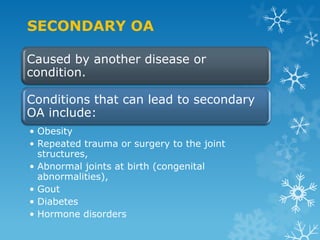
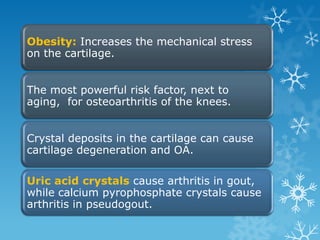
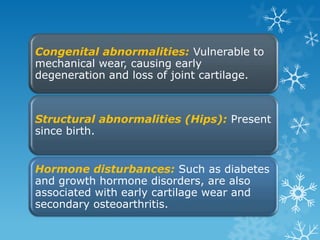
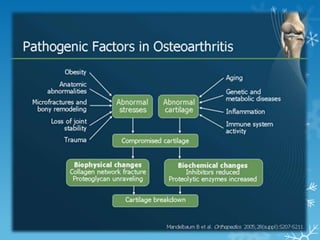
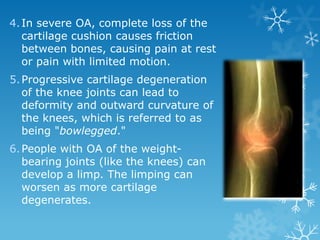
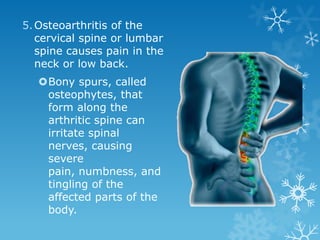
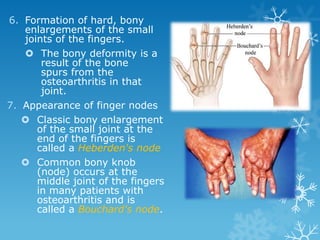
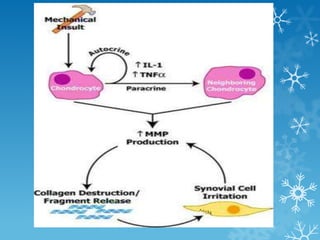
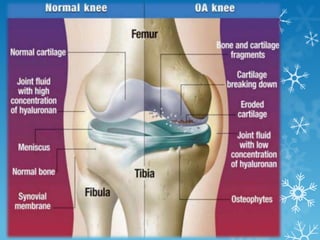
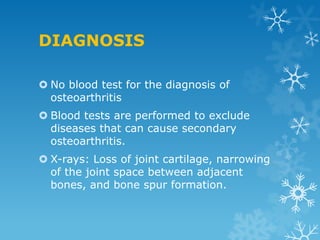
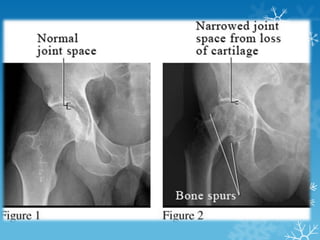
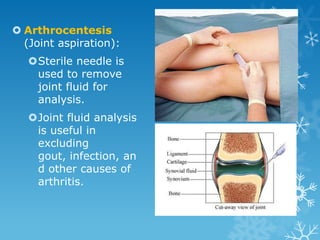
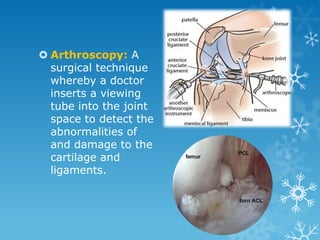
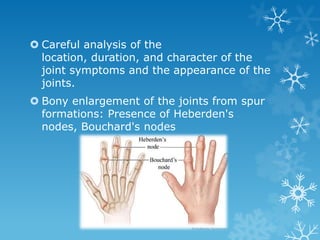
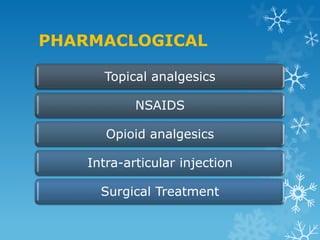
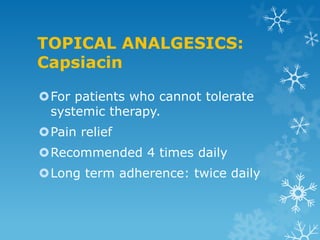
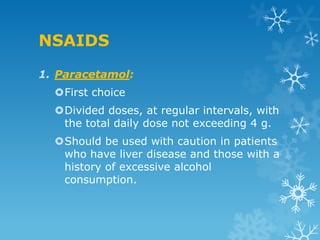
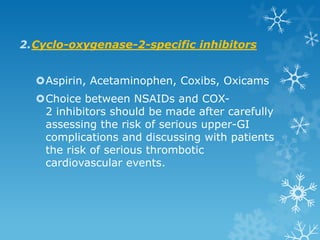
This document provides an overview of osteoarthritis. It begins by defining osteoarthritis as a type of arthritis caused by the breakdown of cartilage between bones in a joint. It then discusses the common joints affected, occurrences based on age and population, and primary versus secondary causes related to aging, injury, genetics, and other conditions. The document outlines symptoms, the etiopathogenesis of cartilage breakdown, diagnosis methods, and treatment options including non-pharmacological therapies, topical analgesics, oral medications, injections, and surgery.