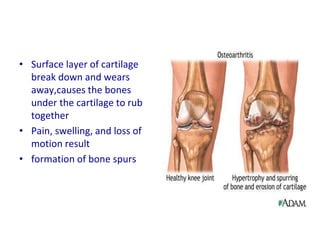
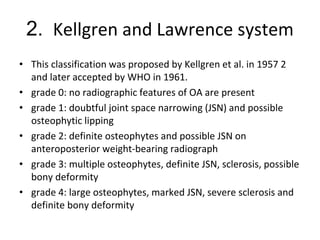
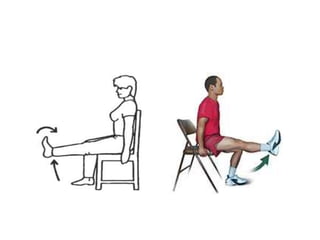
This document summarizes osteoarthritis of the knee. It describes OA as a degenerative joint disease characterized by loss of cartilage and bone changes. Risk factors include age, obesity, joint injury, and genetics. Symptoms include pain and stiffness that worsen with use. Diagnosis is based on symptoms and x-rays showing cartilage loss, bone spurs, and bone changes. Treatment focuses on reducing pain and inflammation, maintaining joint motion, and may include medications, injections, exercise, or surgery like knee replacement for severe cases.