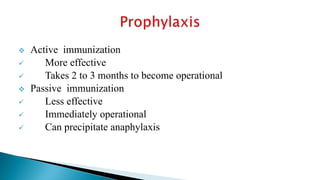
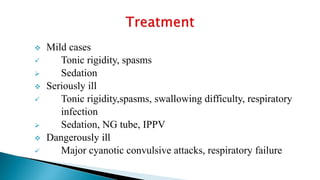
Tetanus is caused by Clostridium tetani bacteria and is characterized by painful muscle spasms. It is spread through contamination of wounds, especially those exposed to dirt or manure. The document discusses the microbiology, types, pathogenesis, prophylaxis with tetanus toxoid immunization, and management of tetanus which involves wound debridement, antibiotics, antitoxin administration, and supportive care. Prognosis depends on immune status and wound severity, with mortality rates as high as 50-60% without treatment.