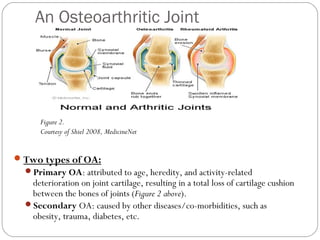
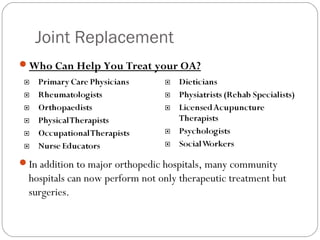
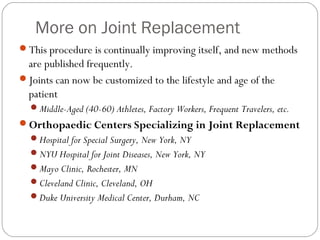
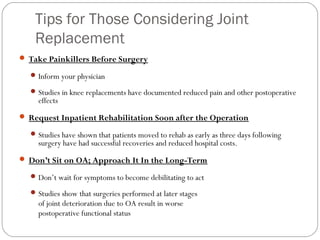
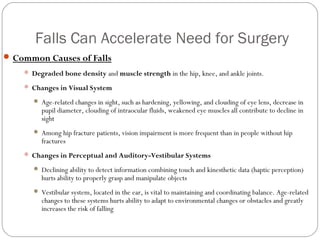
Osteoarthritis and Total Joint Replacement: Risk Factors, Prevention, and Treatment, and the Effects on Sensory Mechanisms Encountered by Osteoarthritic Total Joint Replacement Patients. This document discusses osteoarthritis, including risk factors like age and obesity, common symptoms like joint pain and stiffness, diagnostic methods like x-rays, and treatment options like physical therapy, medications, joint replacements and resurfacing. It also covers changes to sensory systems like vision and balance that can increase fall risks for osteoarthritic patients and accelerate the need for joint replacement surgery.