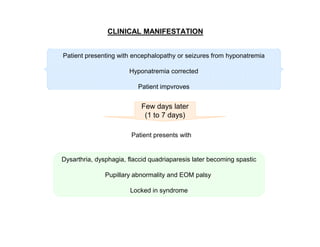
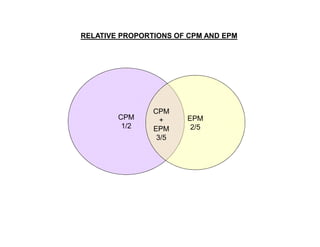
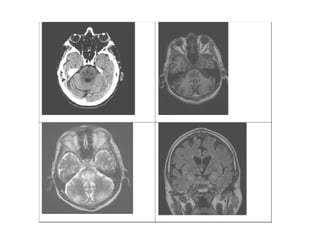
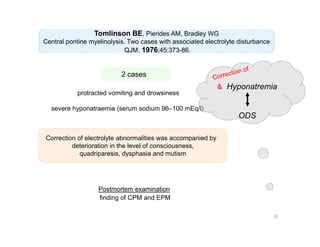
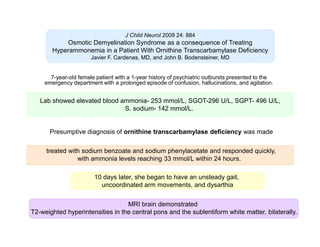
1) A 58-year old male developed central pontine myelinolysis (CPM) and extrapontine myelinolysis (EPM) four days after being discharged from the ICU following treatment for hyponatremia.
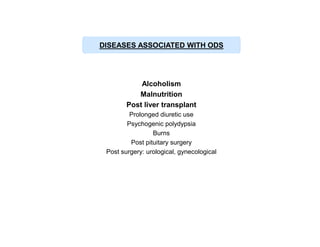
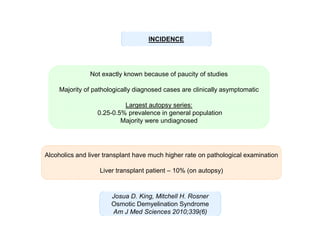
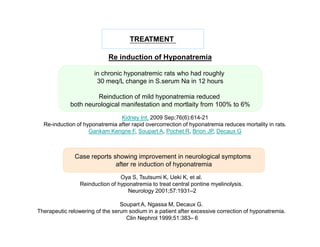
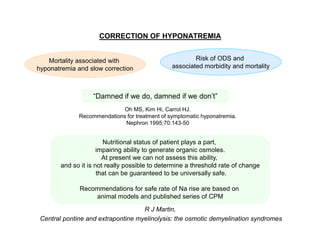
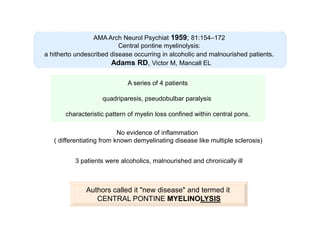
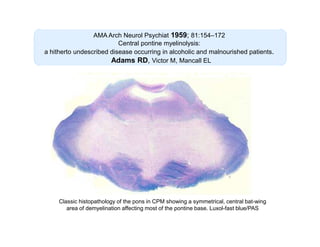
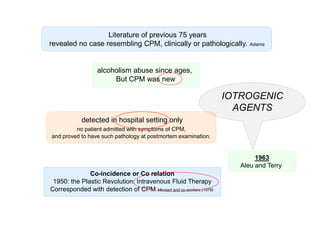
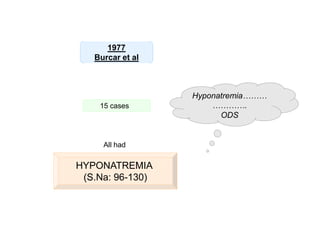
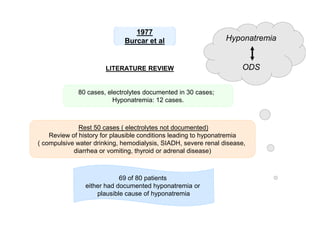
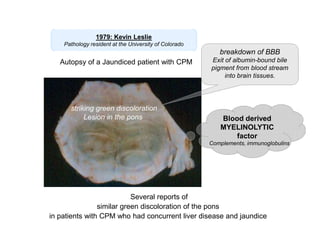
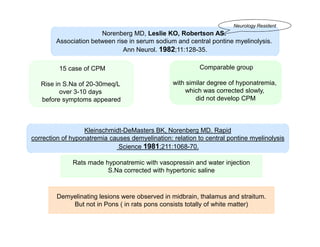
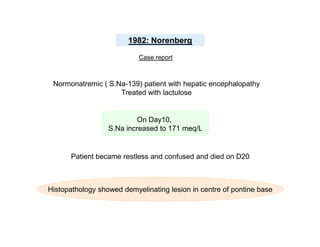
2) CPM was first described in 1959 as a demyelinating condition affecting the pons seen in alcoholic and malnourished patients. Subsequent studies found it can result from rapid correction of hyponatremia.
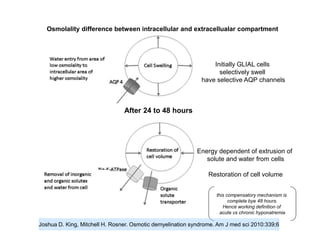
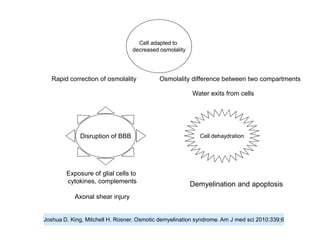
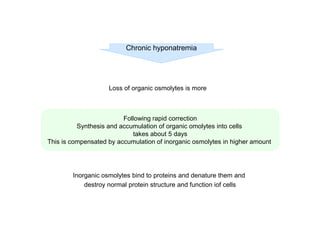
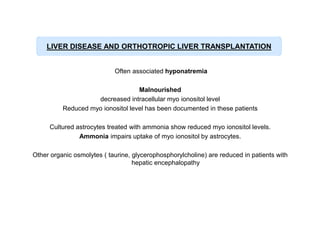
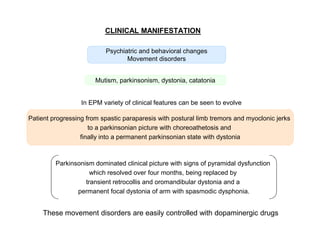
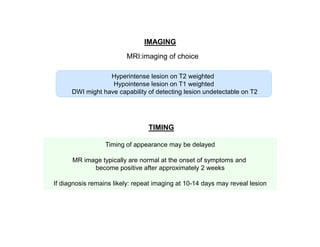
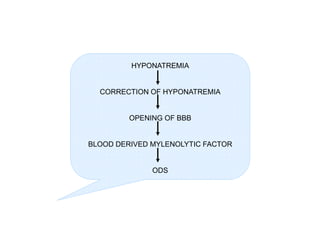
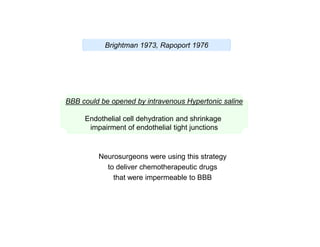
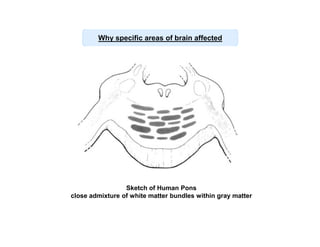
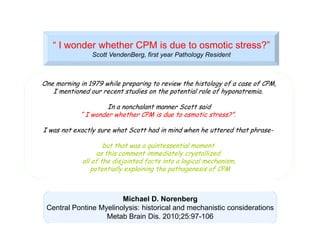
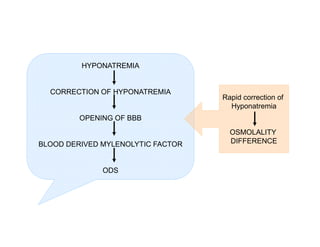
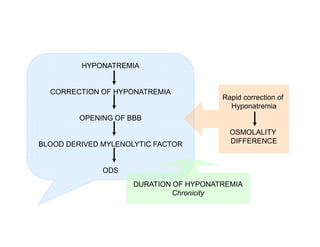
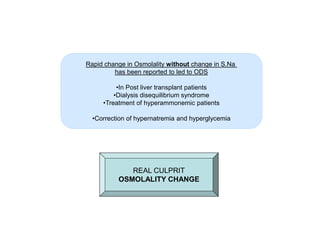
3) The pathogenesis of CPM/EPM involves rapid correction of hyponatremia causing an osmotic gradient that opens the blood-brain barrier, allowing blood factors to enter and cause demyelination. The specific







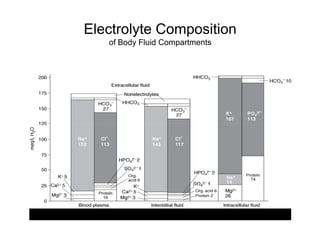
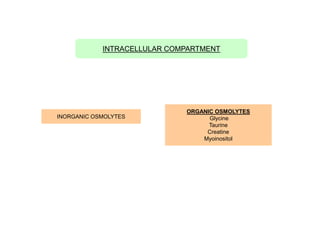
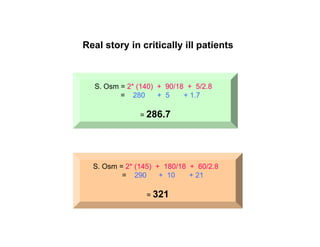
![Na is the most abundant molecule in ECF
Na is the most osmotically active molecule ( Osmolytes) in ECF
Contribution of Gluc and BUN is
5 mOsm/L
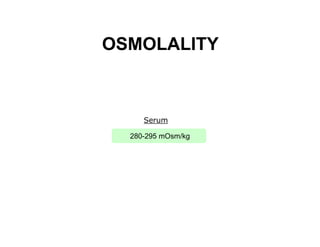
S. Osm ( mOsm/kg of water)
(2*[Na] + [Glucose/18] + [BUN/2.8]
(Na in meq/L, Glucose in mg/dL, BUN in mg/dL)
Osmotic pressure and osmolality determines
distribution of fluid in body compartments](https://image.slidesharecdn.com/osmoticdemyelinationsyndrome-140209021155-phpapp01/85/Osmotic-demyelination-syndrome-35-320.jpg)