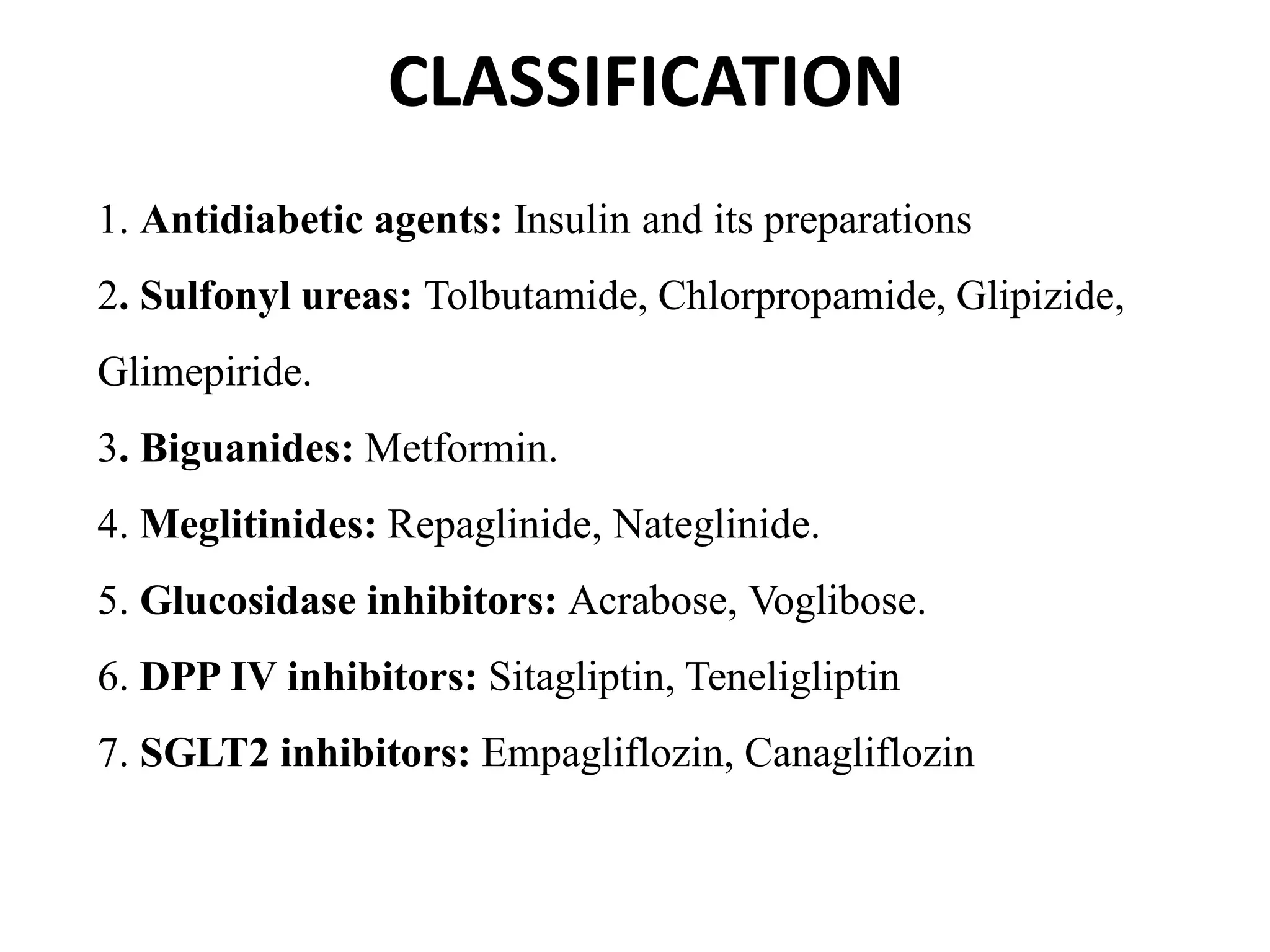
Diabetes is a condition where the body has trouble processing blood sugar. It is important to manage blood sugar levels to avoid complications like heart disease and nerve damage. Oral antidiabetic drugs are medications that can help lower blood sugar levels for people with diabetes.