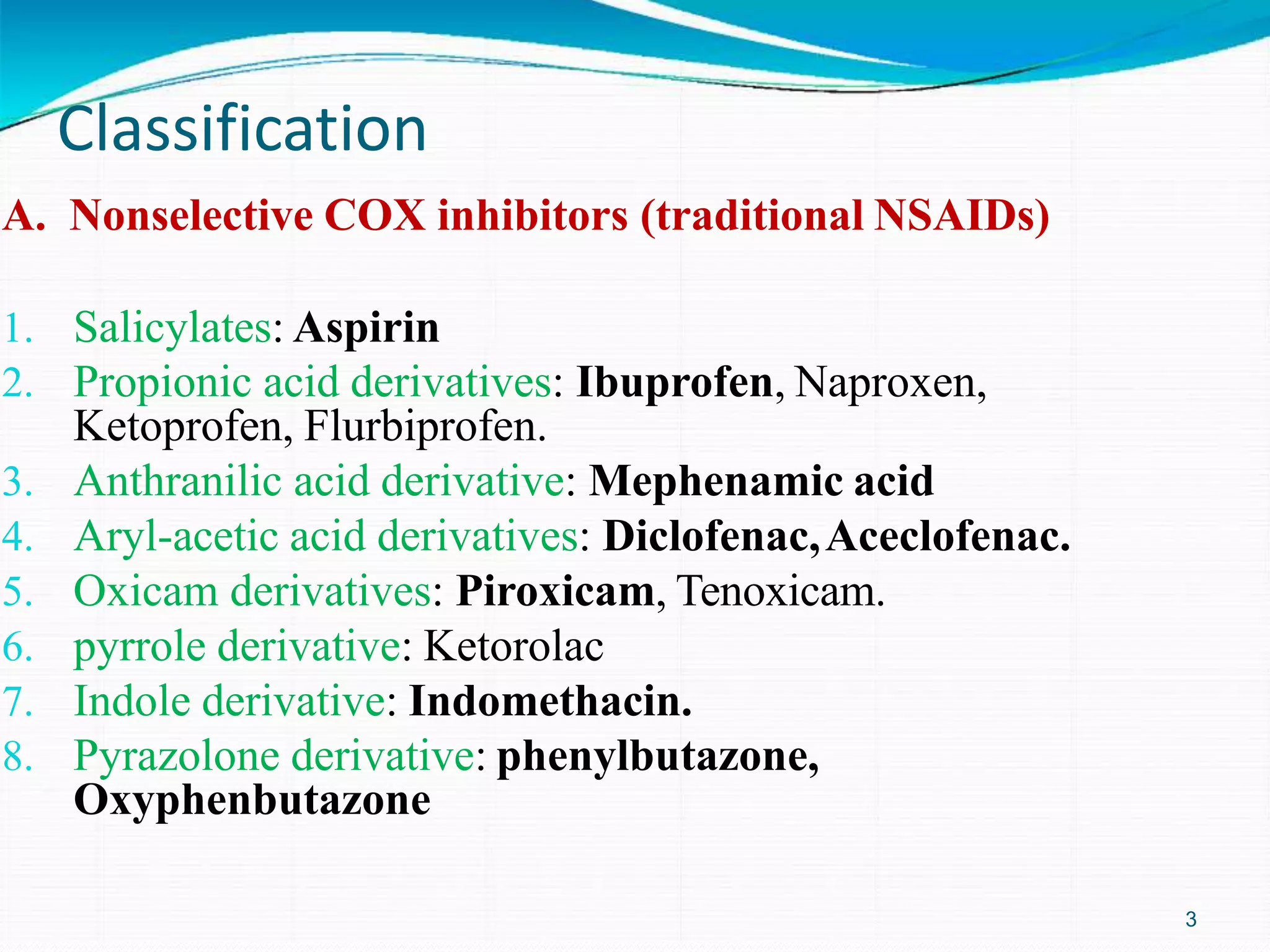
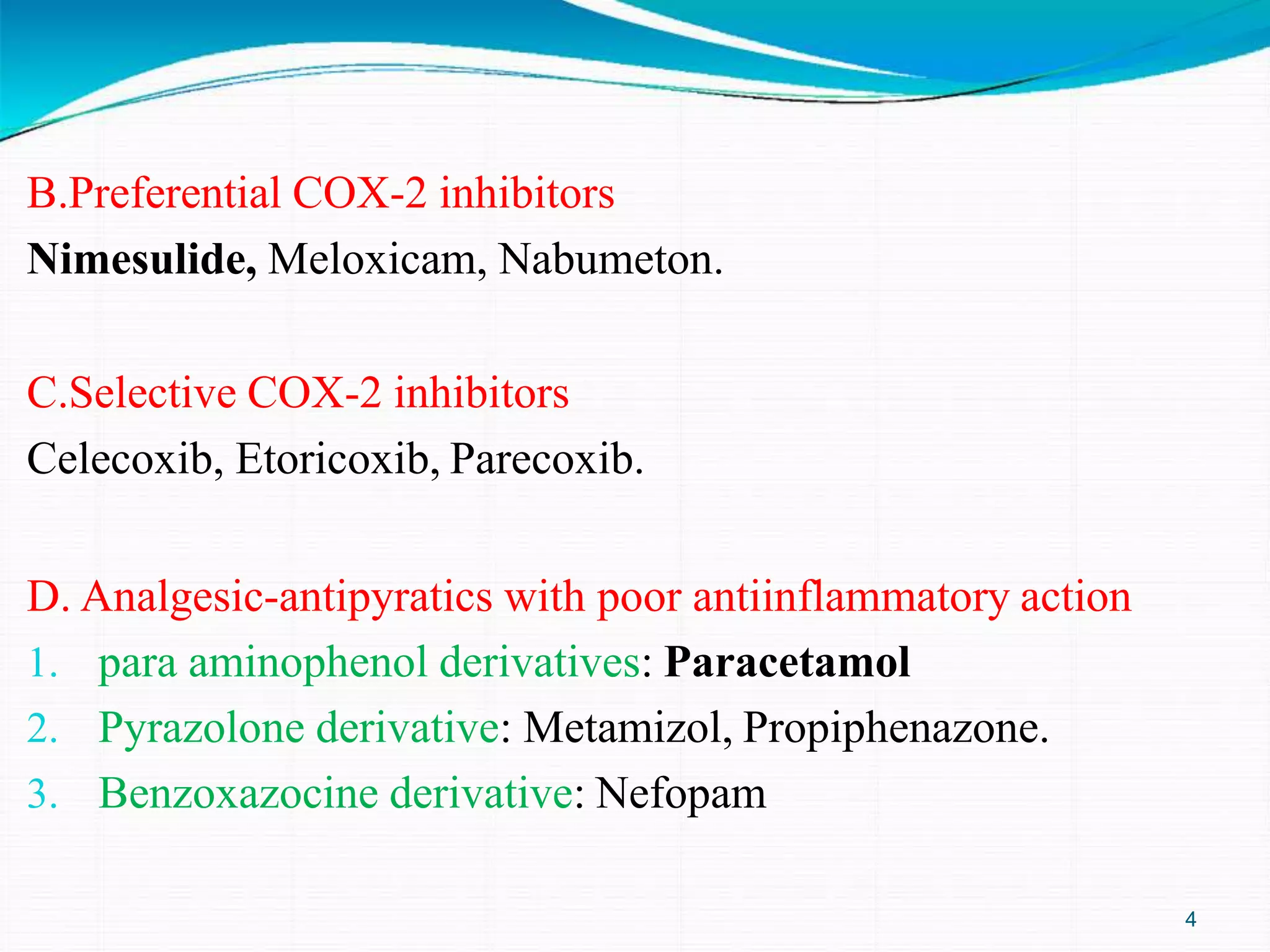
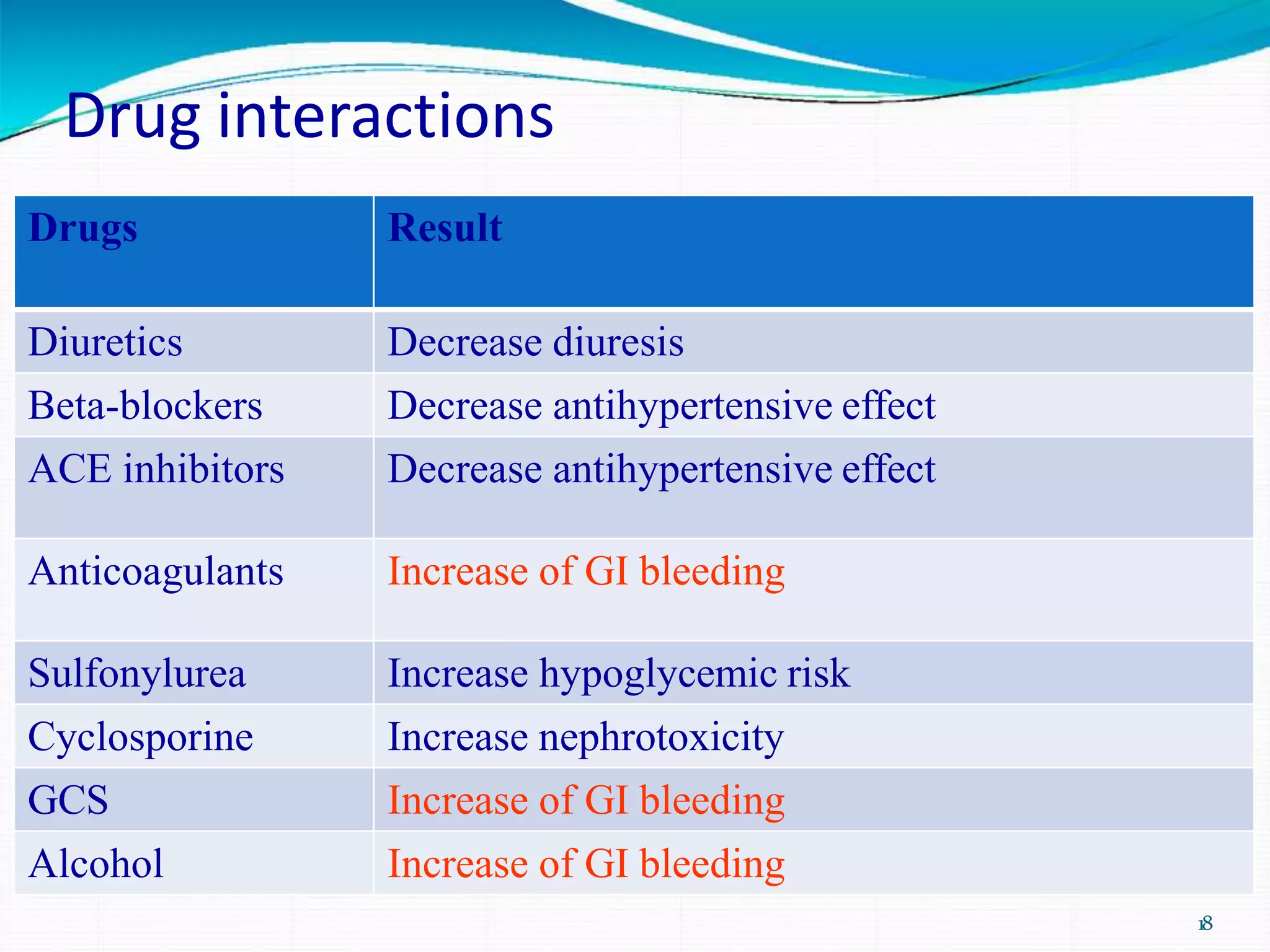
NSAIDs have analgesic, antipyretic and anti-inflammatory properties. They work by inhibiting cyclooxygenase (COX) enzymes and reducing prostaglandin production. NSAIDs are classified as nonselective COX inhibitors like aspirin, preferential COX-2 inhibitors like nimesulide, or selective COX-2 inhibitors like celecoxib. Common adverse effects include gastrointestinal irritation. NSAIDs are used to treat pain, fever, and inflammation conditions like arthritis.