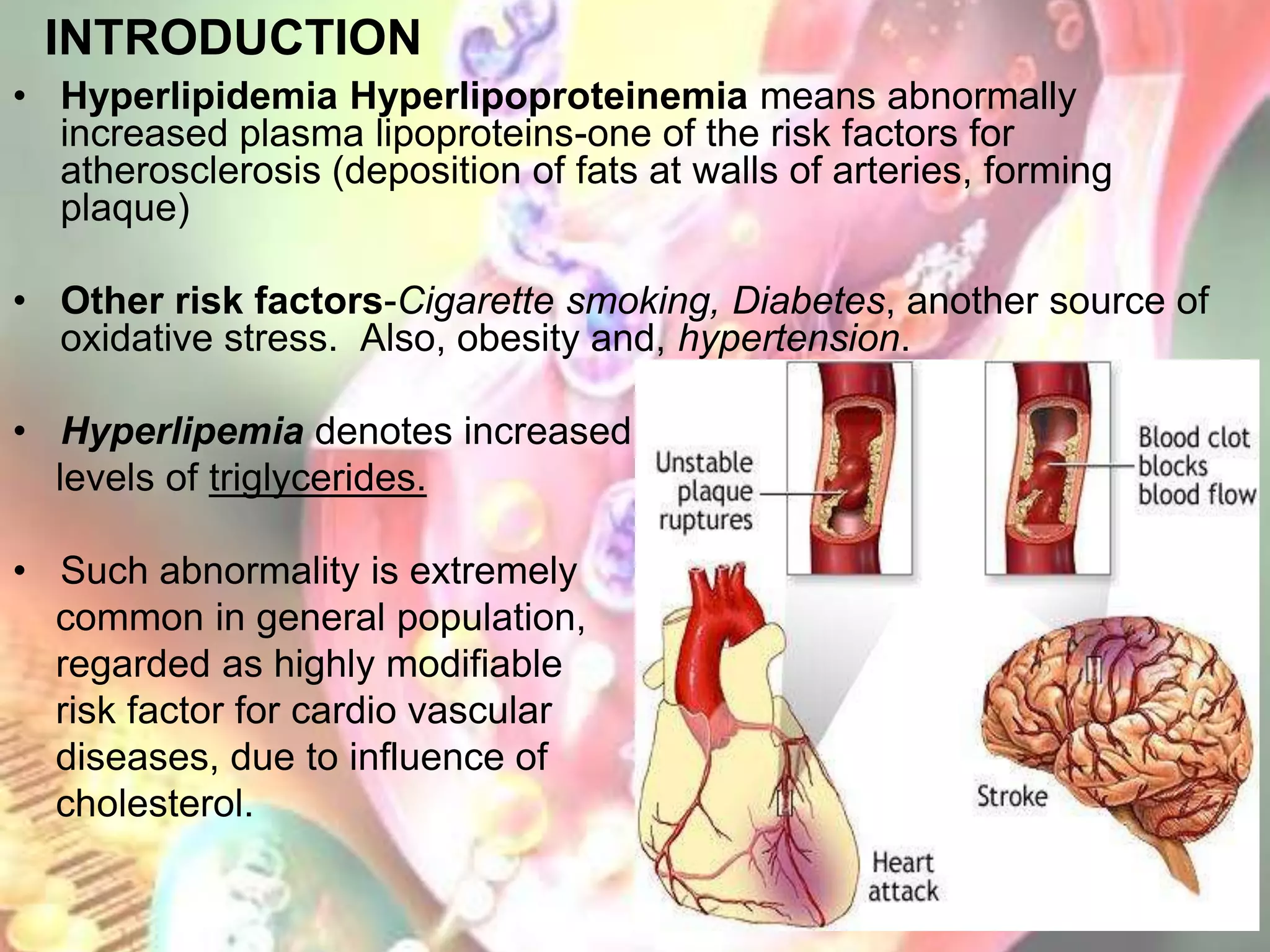
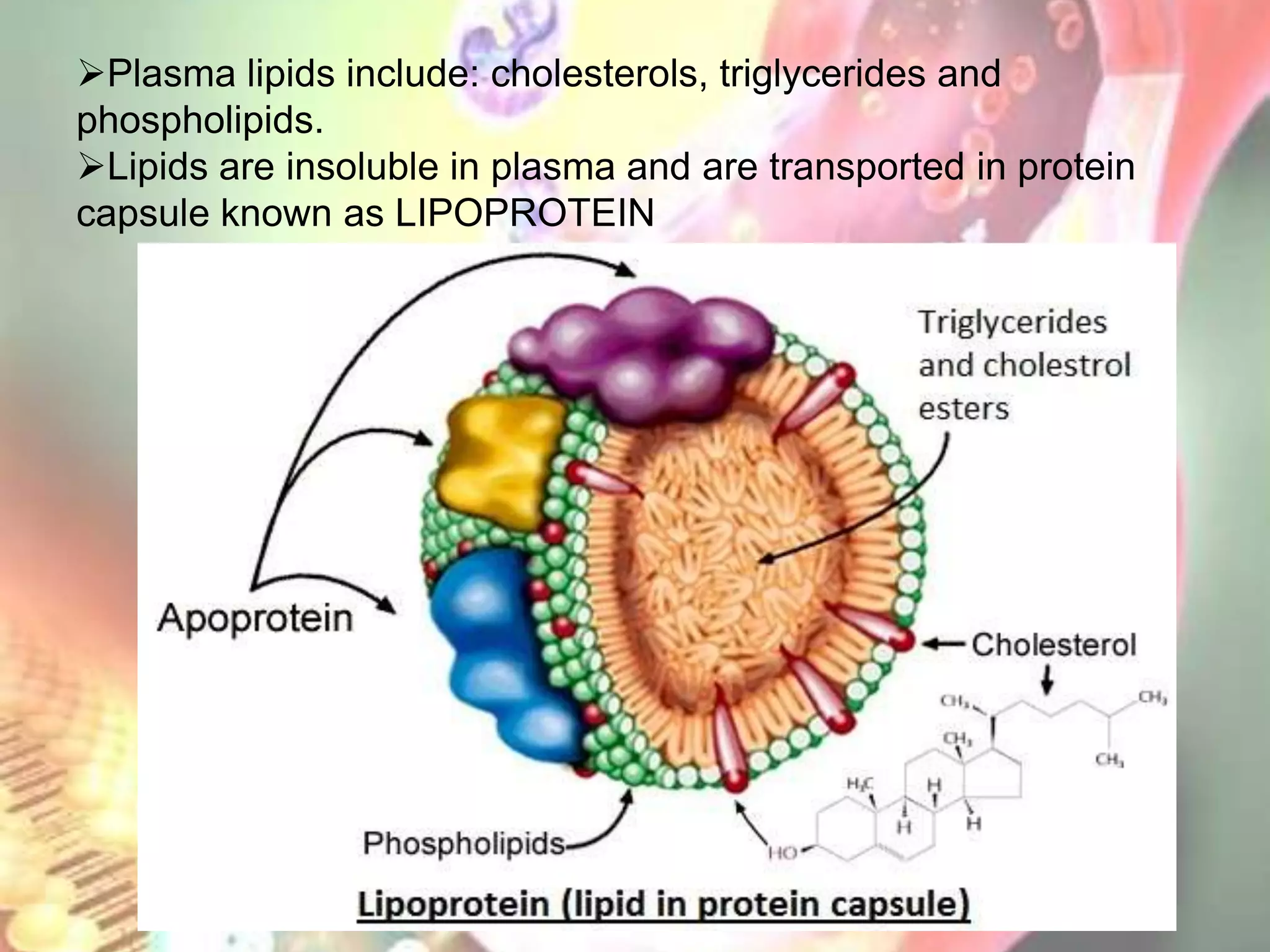
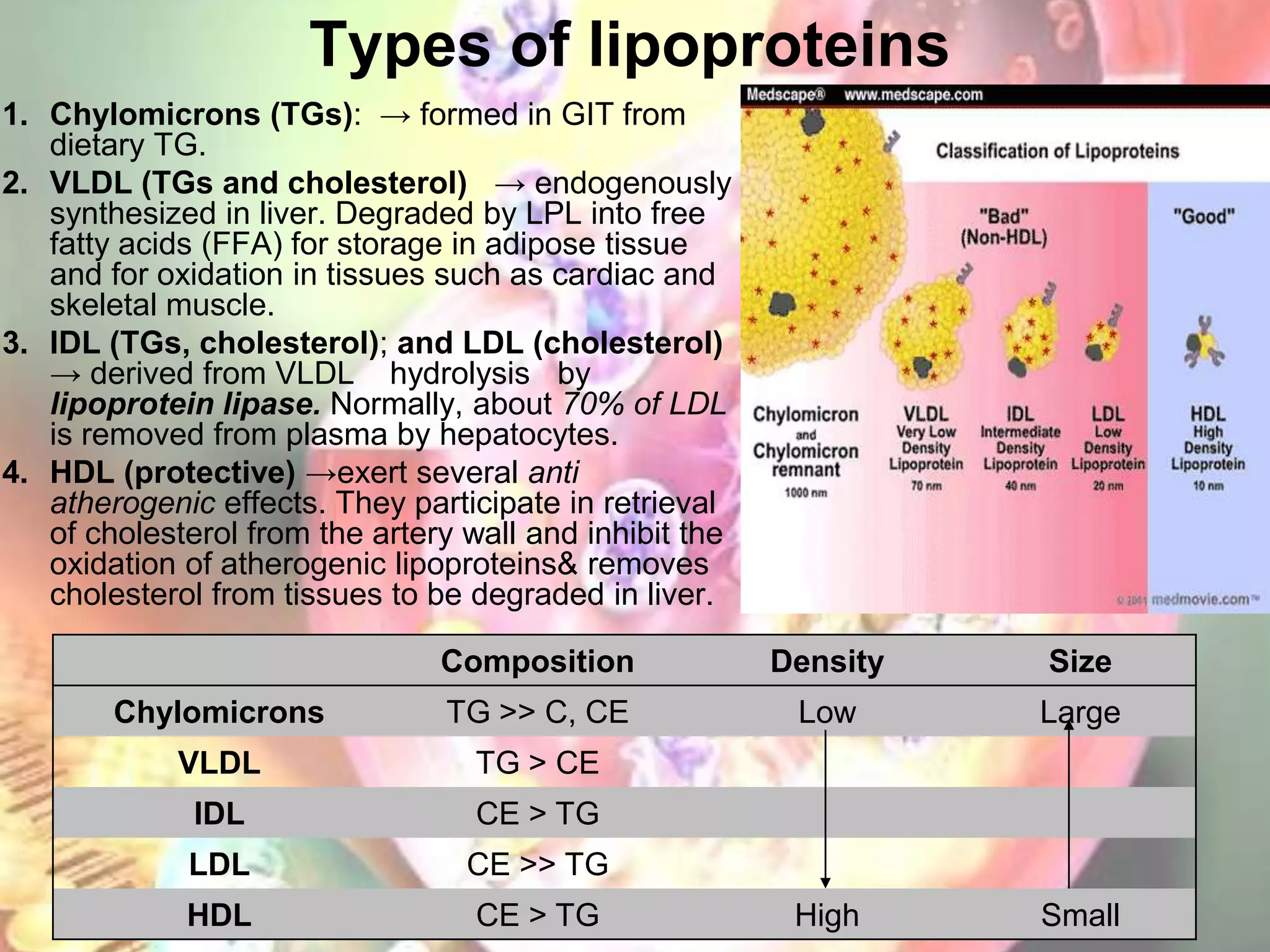
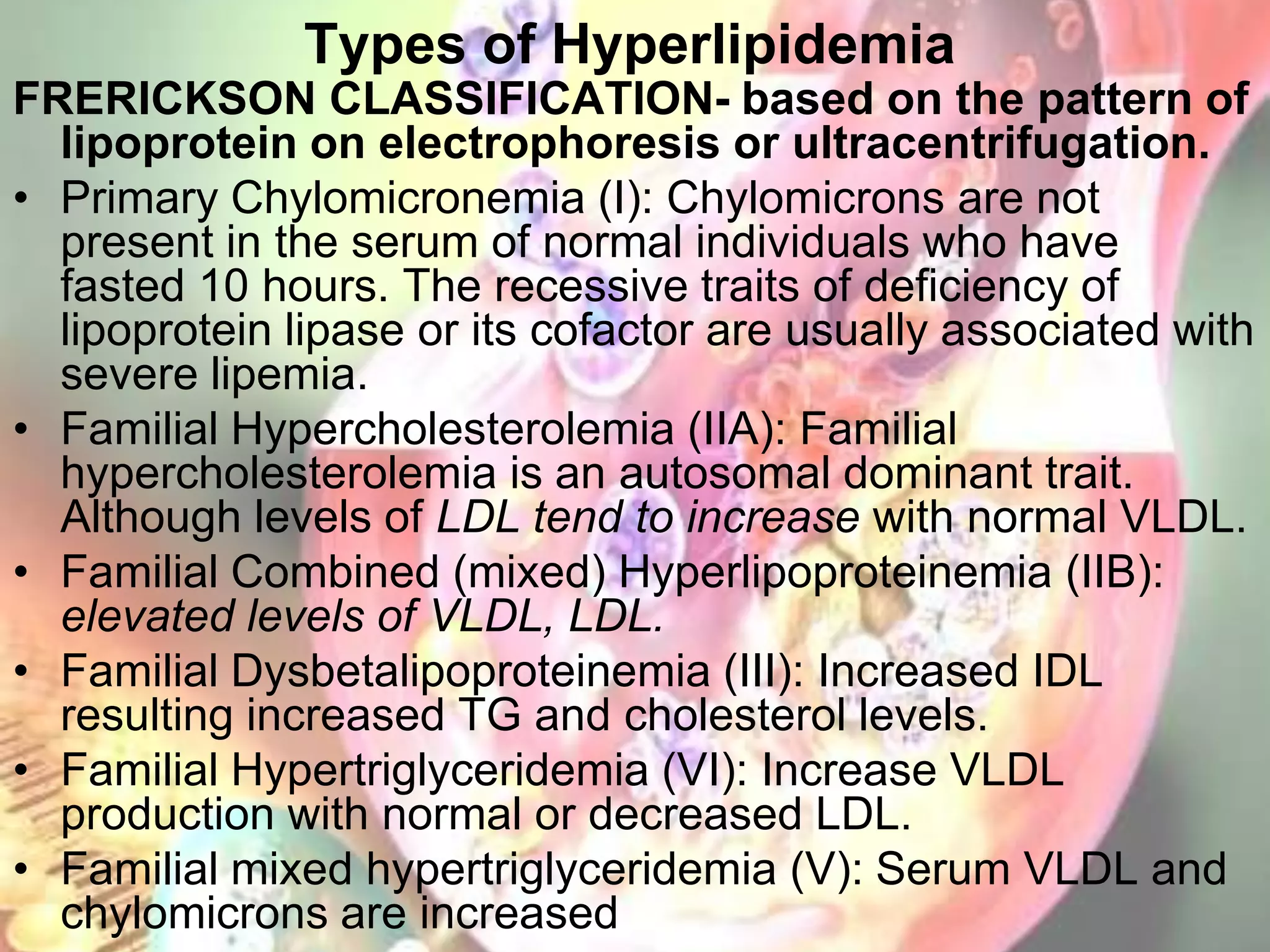
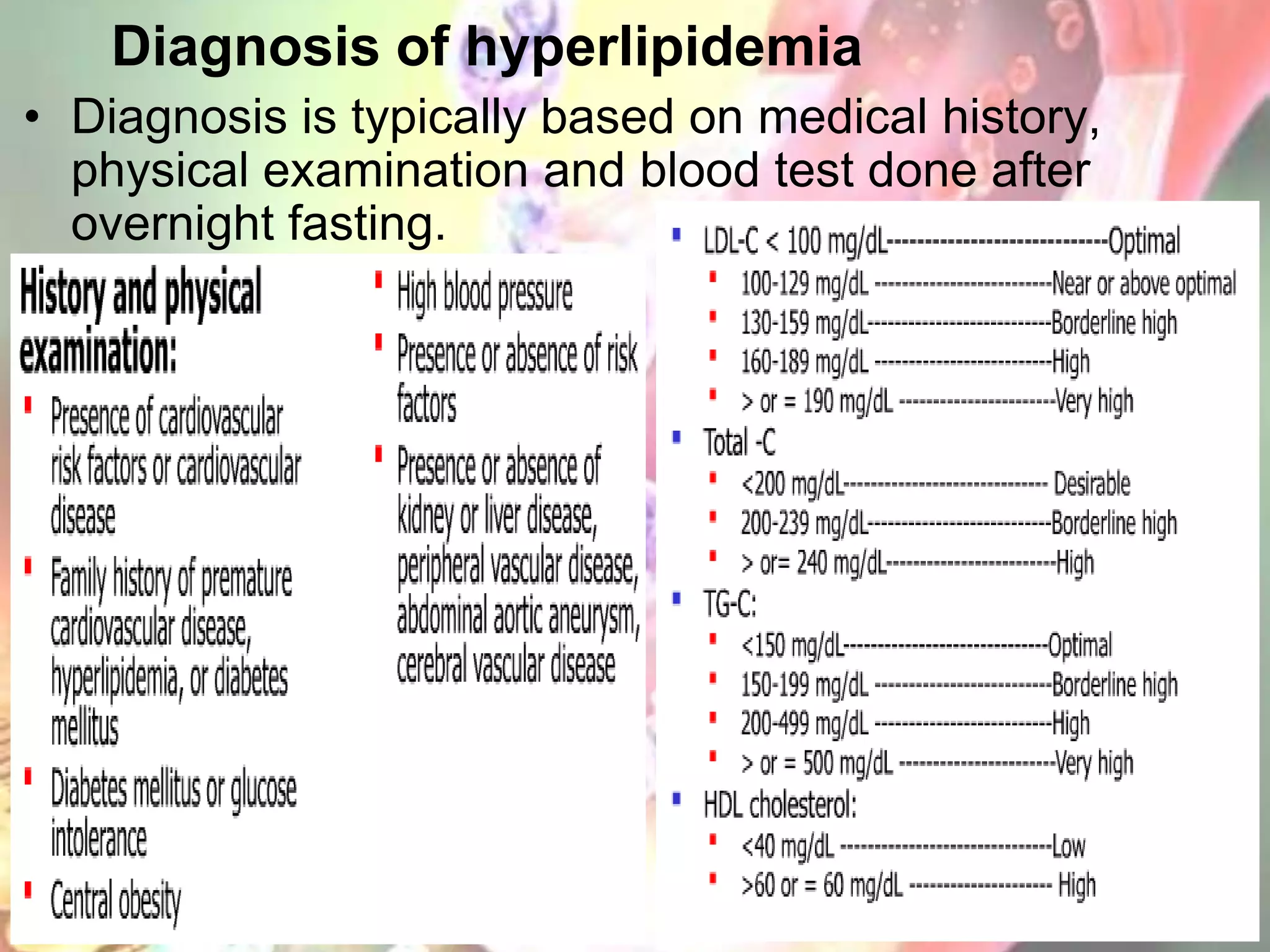
This document discusses hyperlipidemia and drug therapy for hyperlipidemia. It begins by defining hyperlipidemia and describing the main types of lipoproteins and their roles in cholesterol transport. It then discusses the diagnosis and management of hyperlipidemias, including lifestyle modifications like diet and exercise as well as the major classes of drug therapy like statins, fibrates, bile acid sequestrants, and nicotinic acid. The mechanisms of action, uses, and side effects of each drug class are summarized. Combination drug therapy is also addressed when single drug therapy is insufficient.