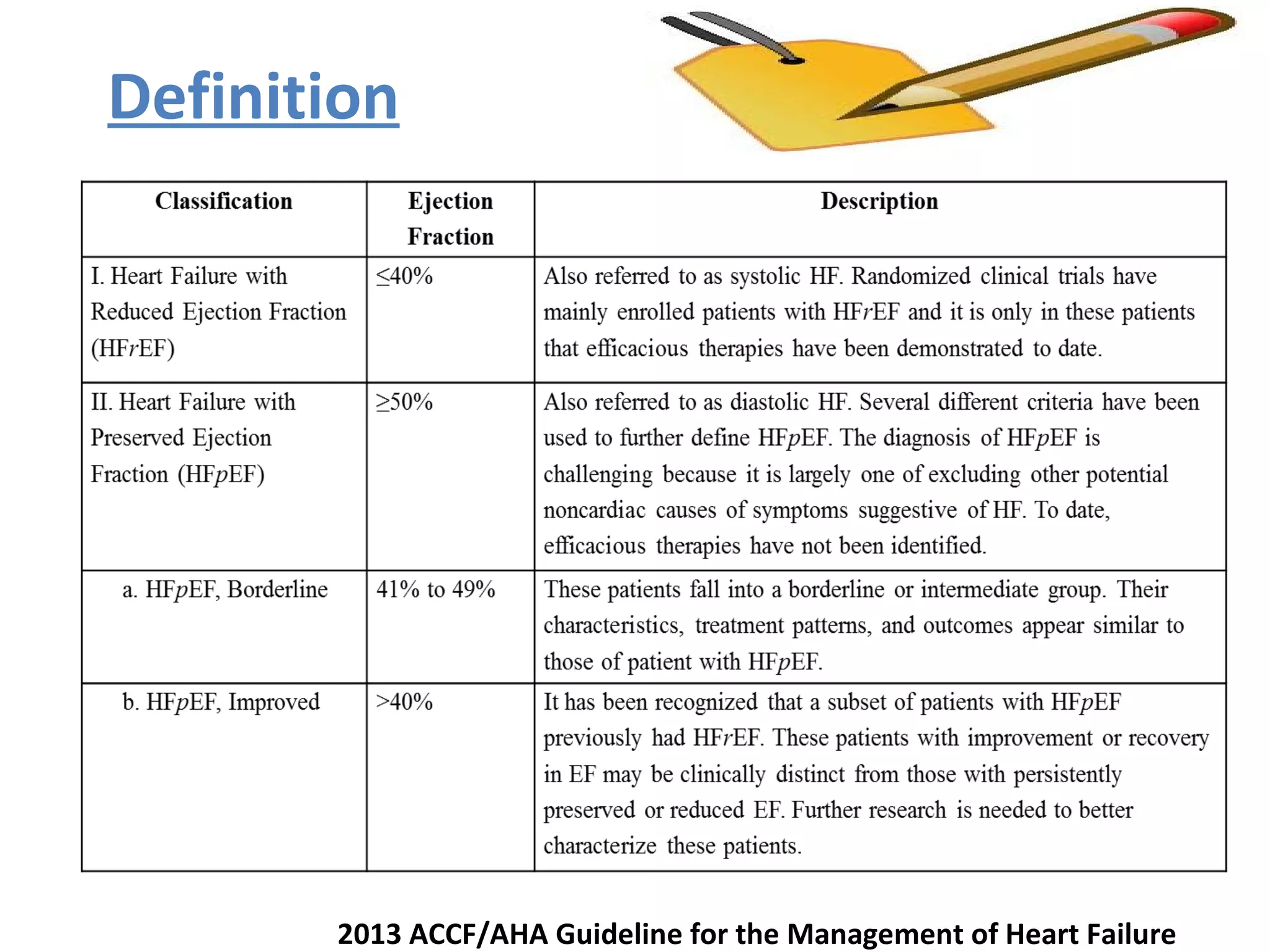
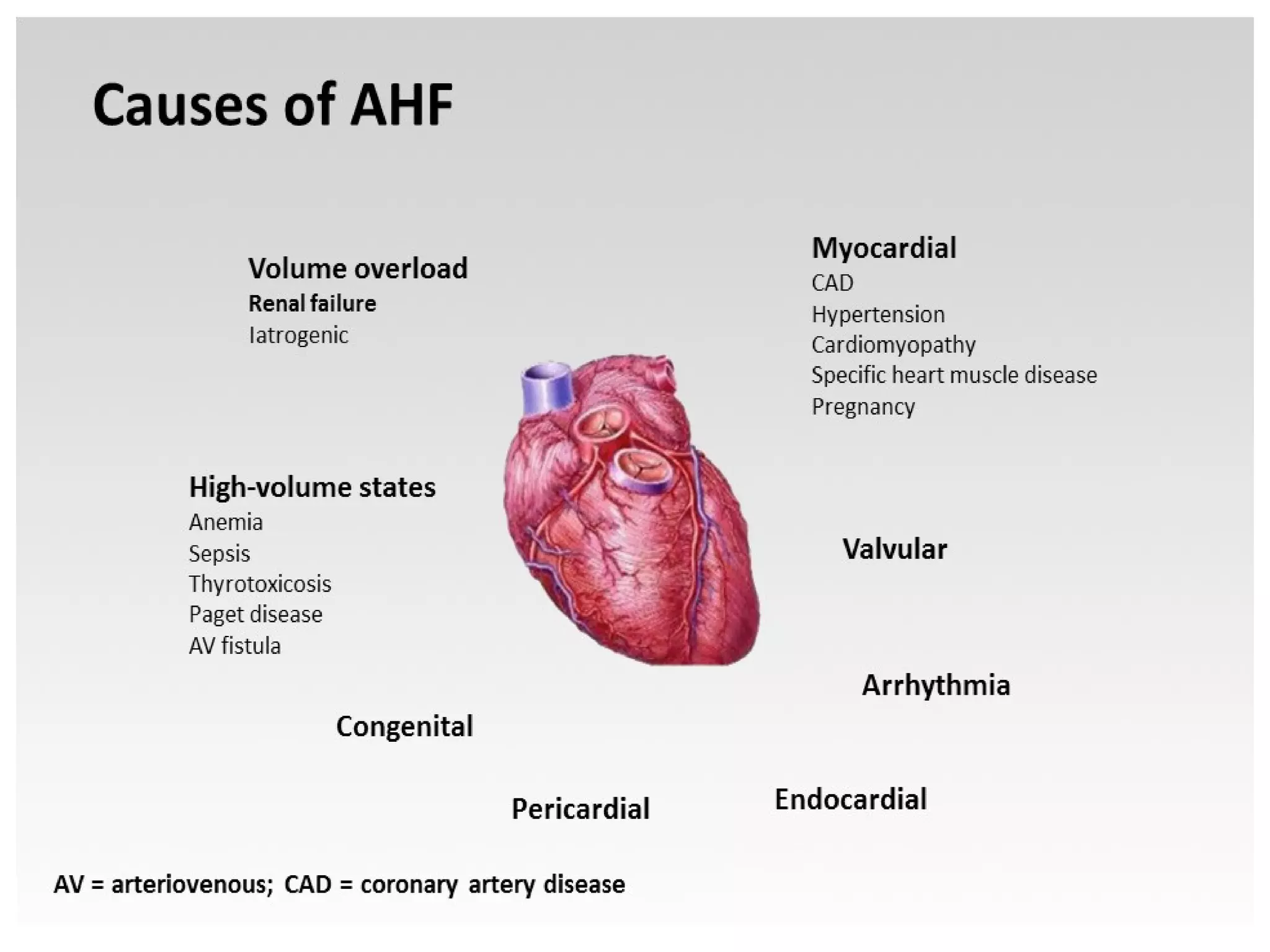
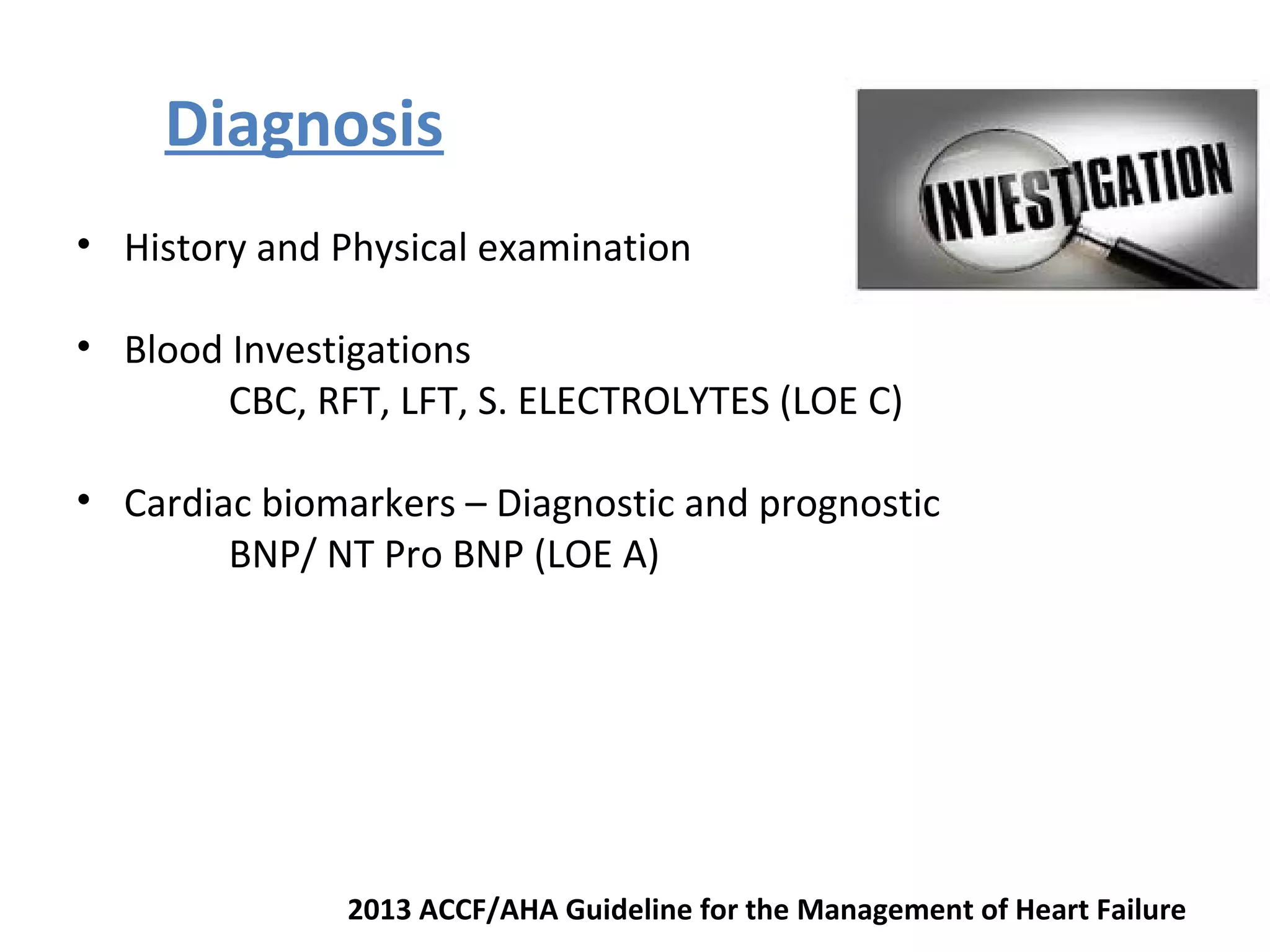
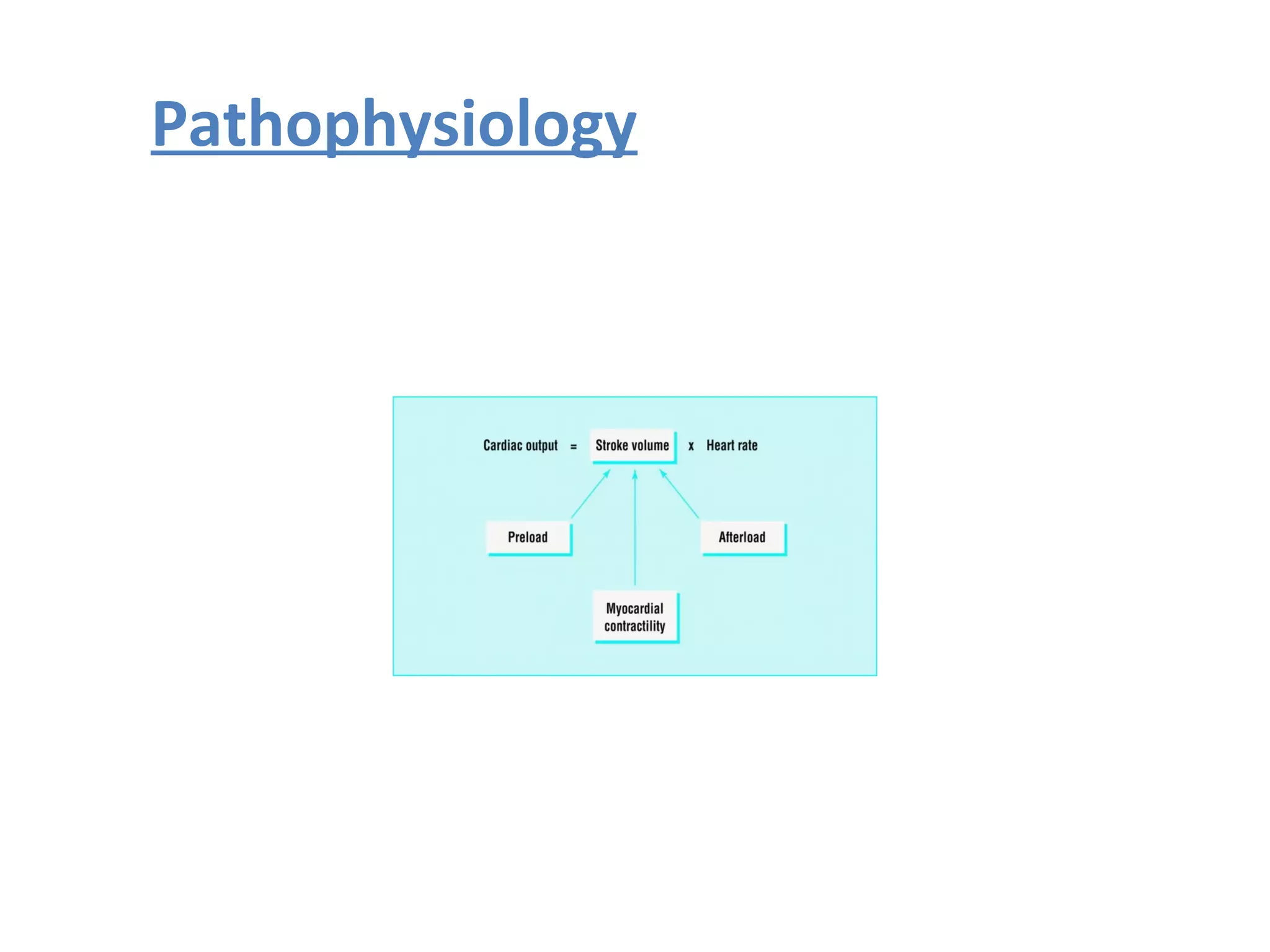
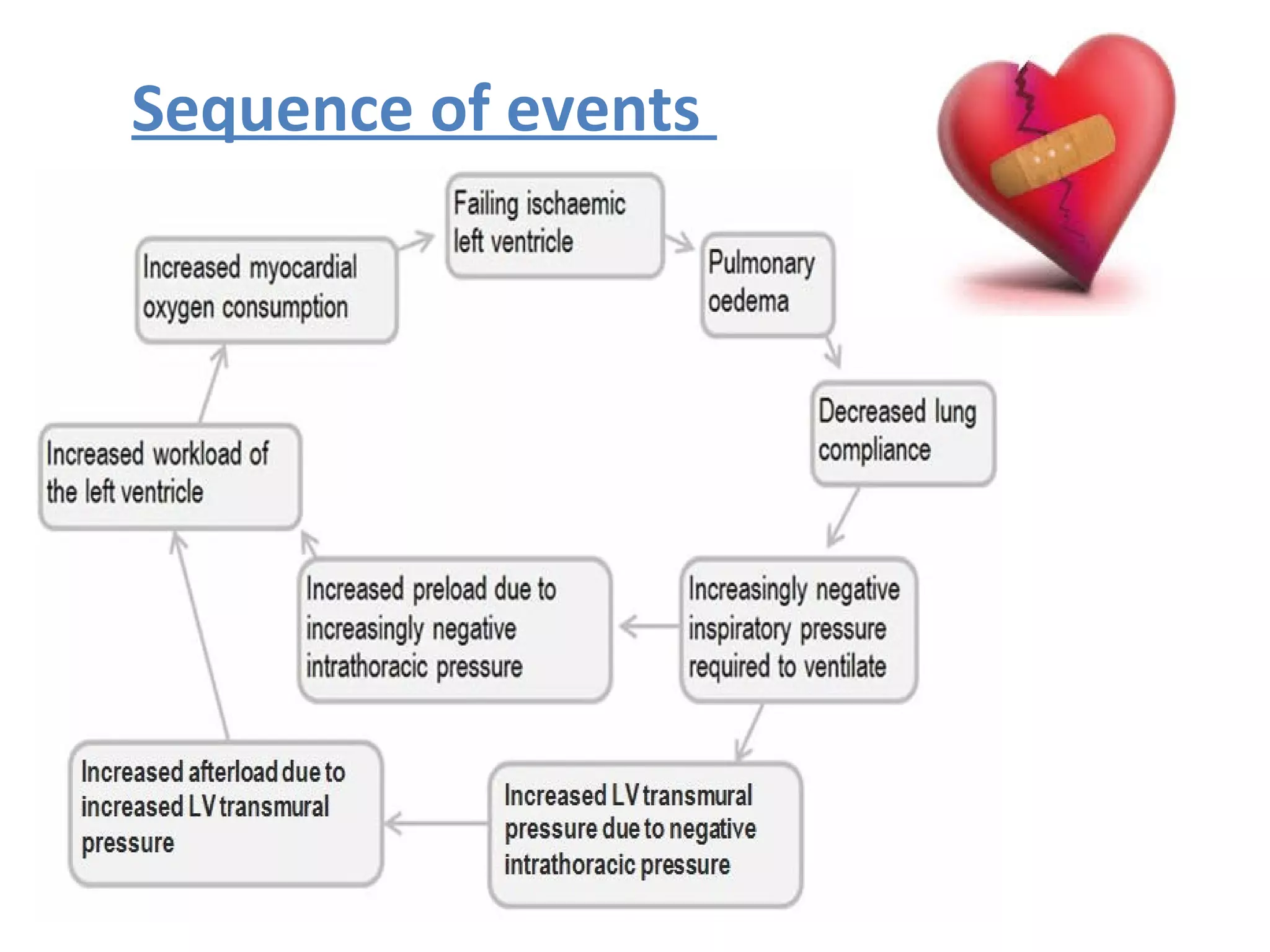
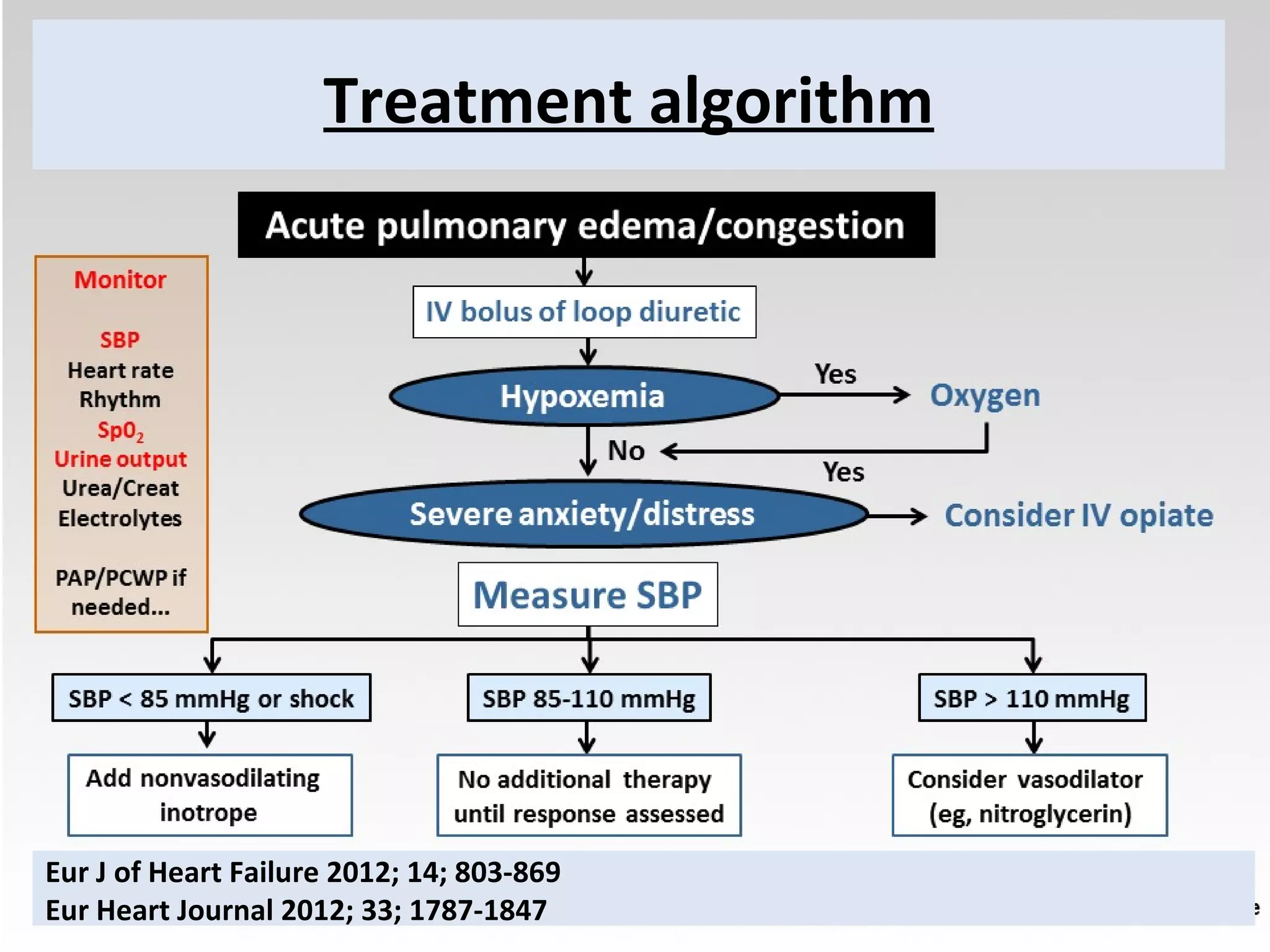
This document discusses ventilation in acute heart failure. It defines key terms like classification of heart failure and diagnostic criteria. It describes the pathophysiology and goals of treatment. Non-invasive ventilation with CPAP or BiPAP is indicated for cardiogenic pulmonary edema to improve oxygenation and reduce workload. Settings, monitoring, complications and indications for invasive ventilation are reviewed. The effects of weaning and NIV for chronic heart failure are also summarized.