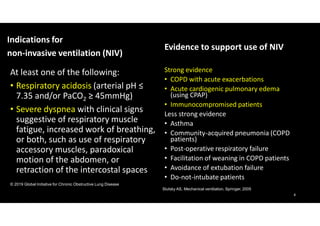
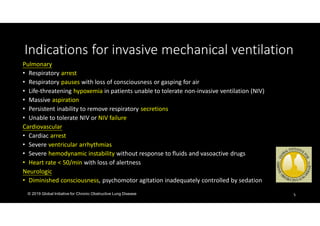
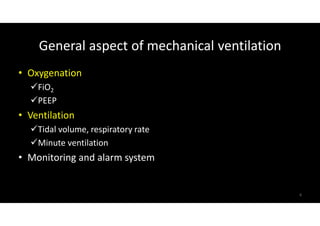
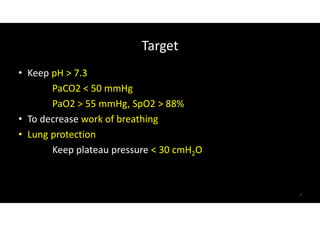
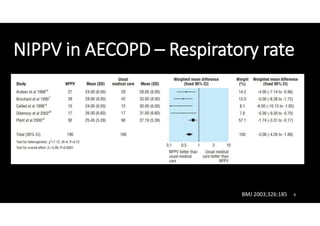
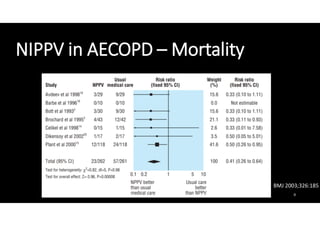
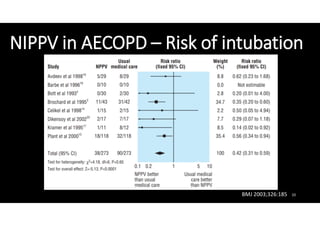
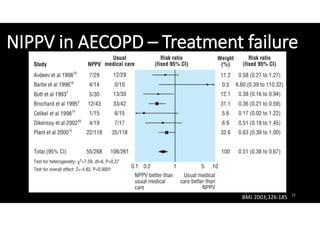
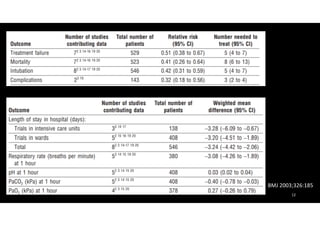
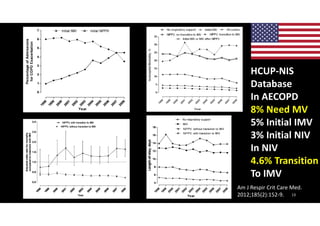
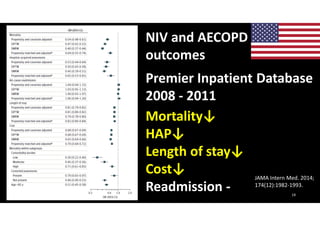
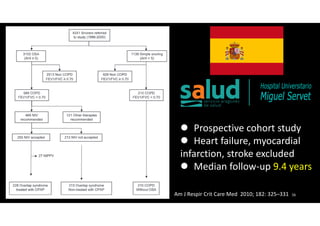
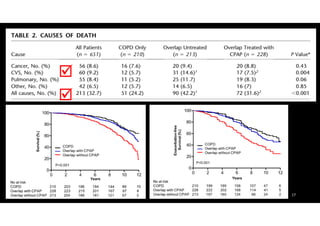
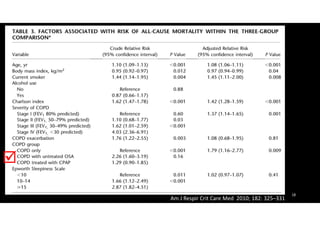
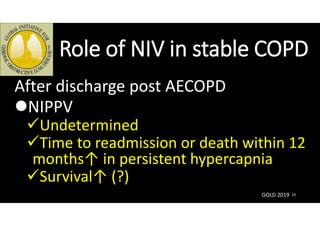
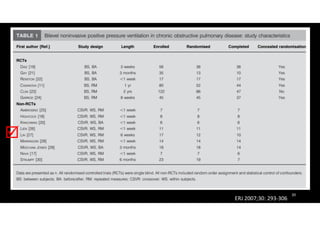
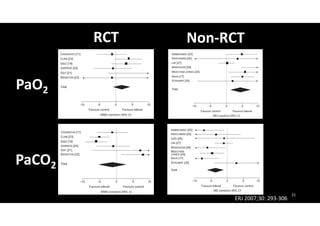
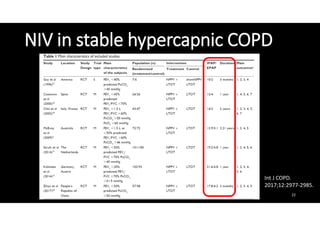
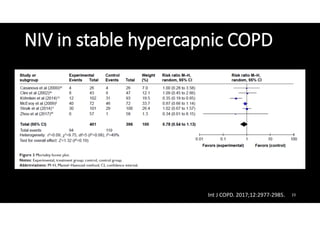
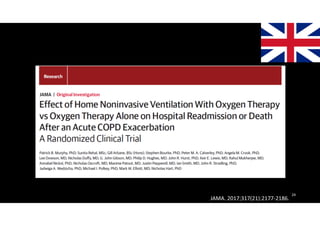
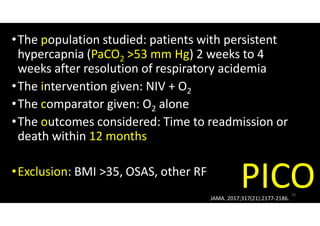
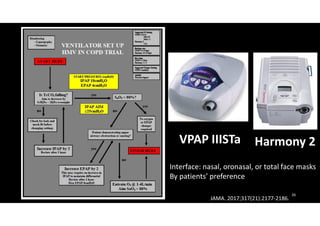
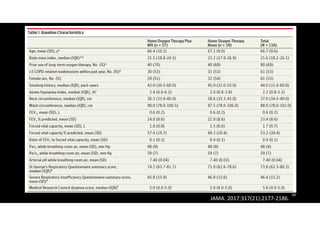
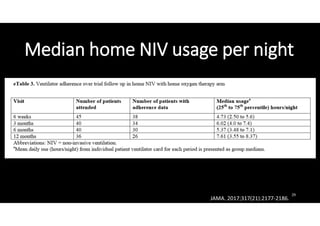
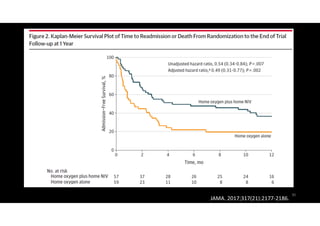
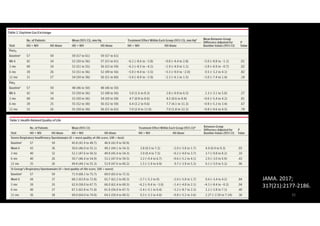
This document discusses the use of noninvasive ventilation (NIV) in patients with chronic obstructive pulmonary disease (COPD). It finds that NIV is the standard of care for COPD patients experiencing acute respiratory failure during acute exacerbations, as it can reduce mortality and morbidity. For stable COPD patients with persistent hypercapnia after an exacerbation, adding NIV to supplemental oxygen may prolong the time to readmission or death compared to oxygen alone. NIV may also provide benefits for some stable COPD patients with hypercapnia or who have both COPD and obstructive sleep apnea.