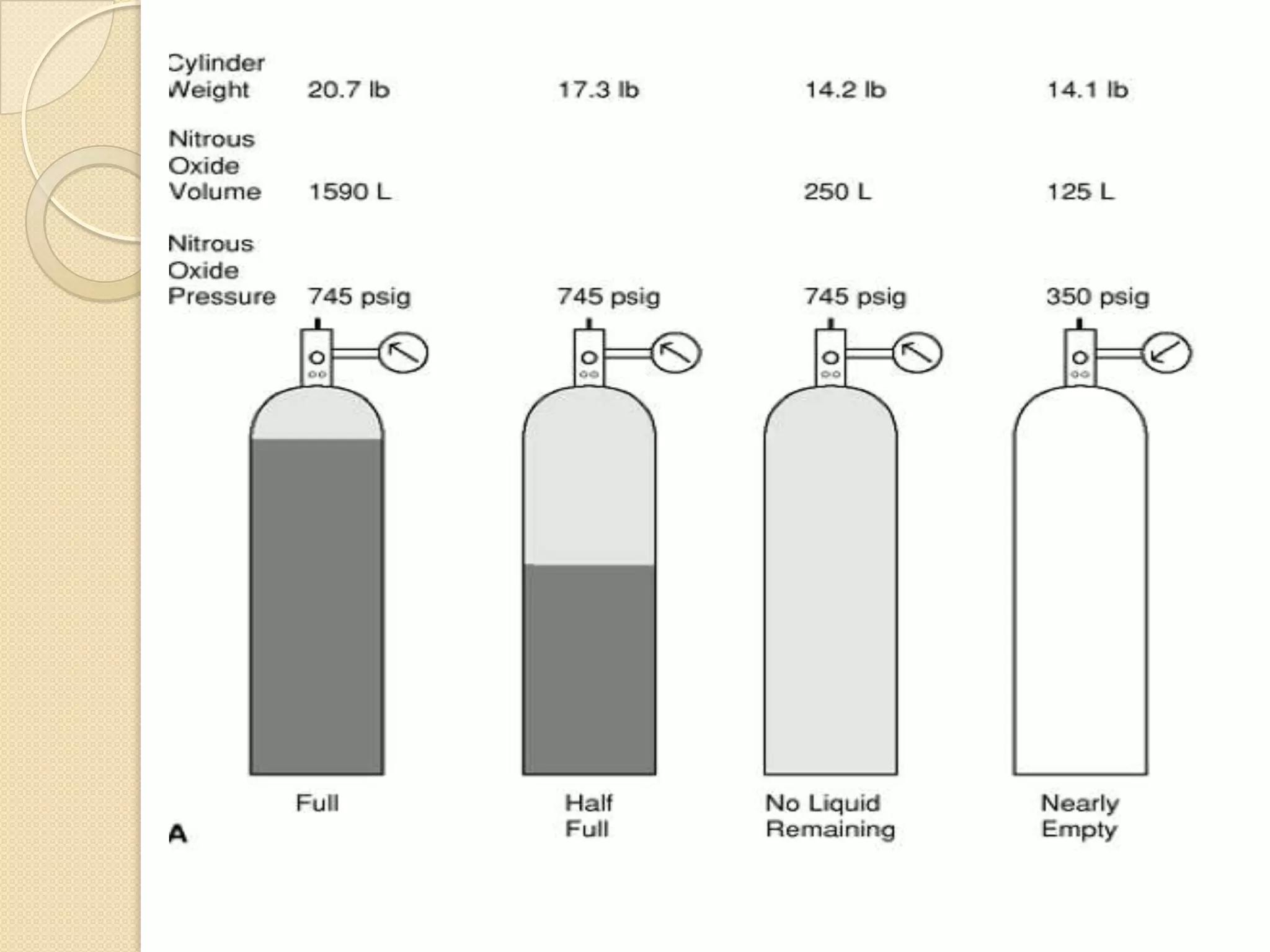
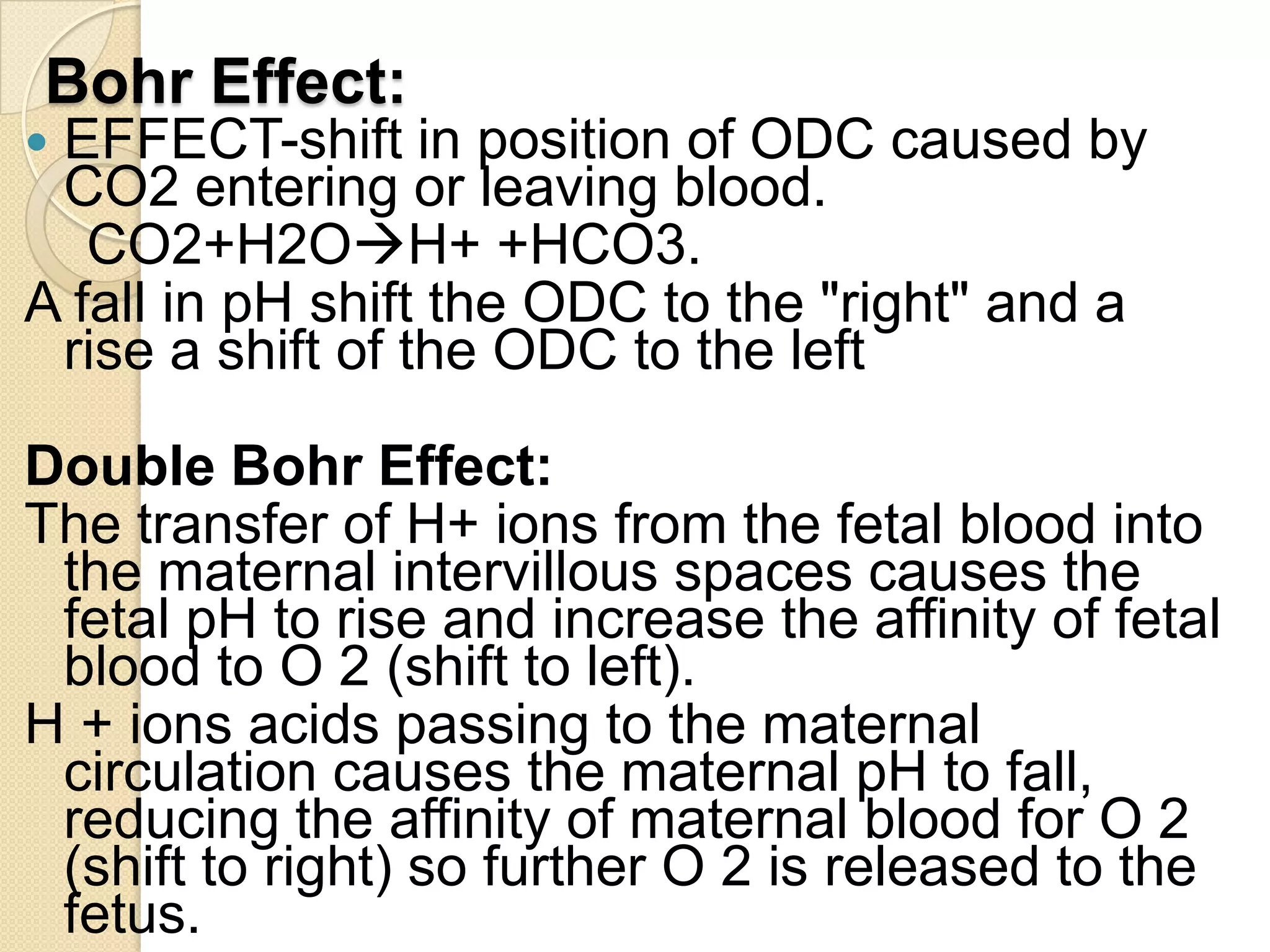
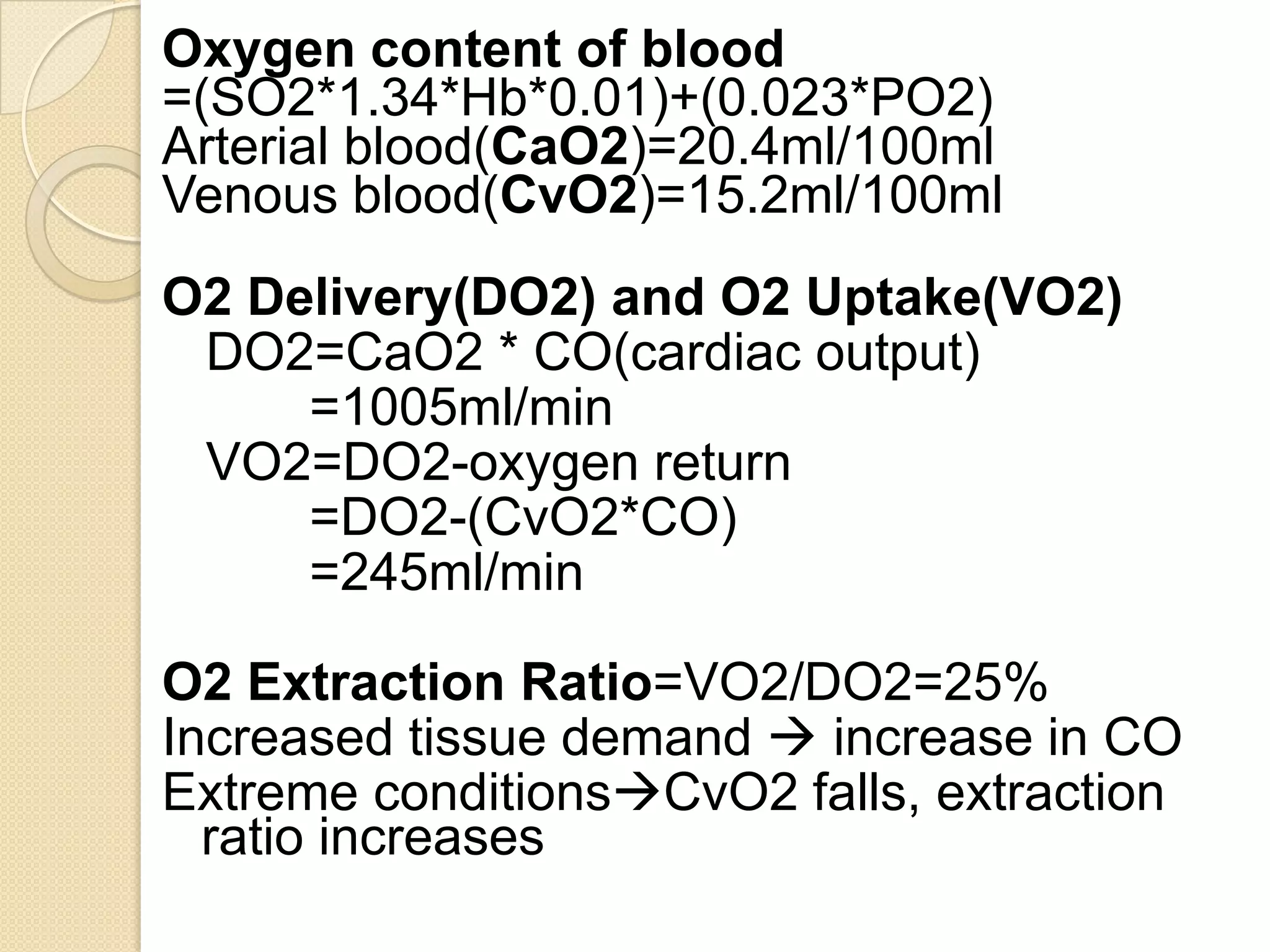
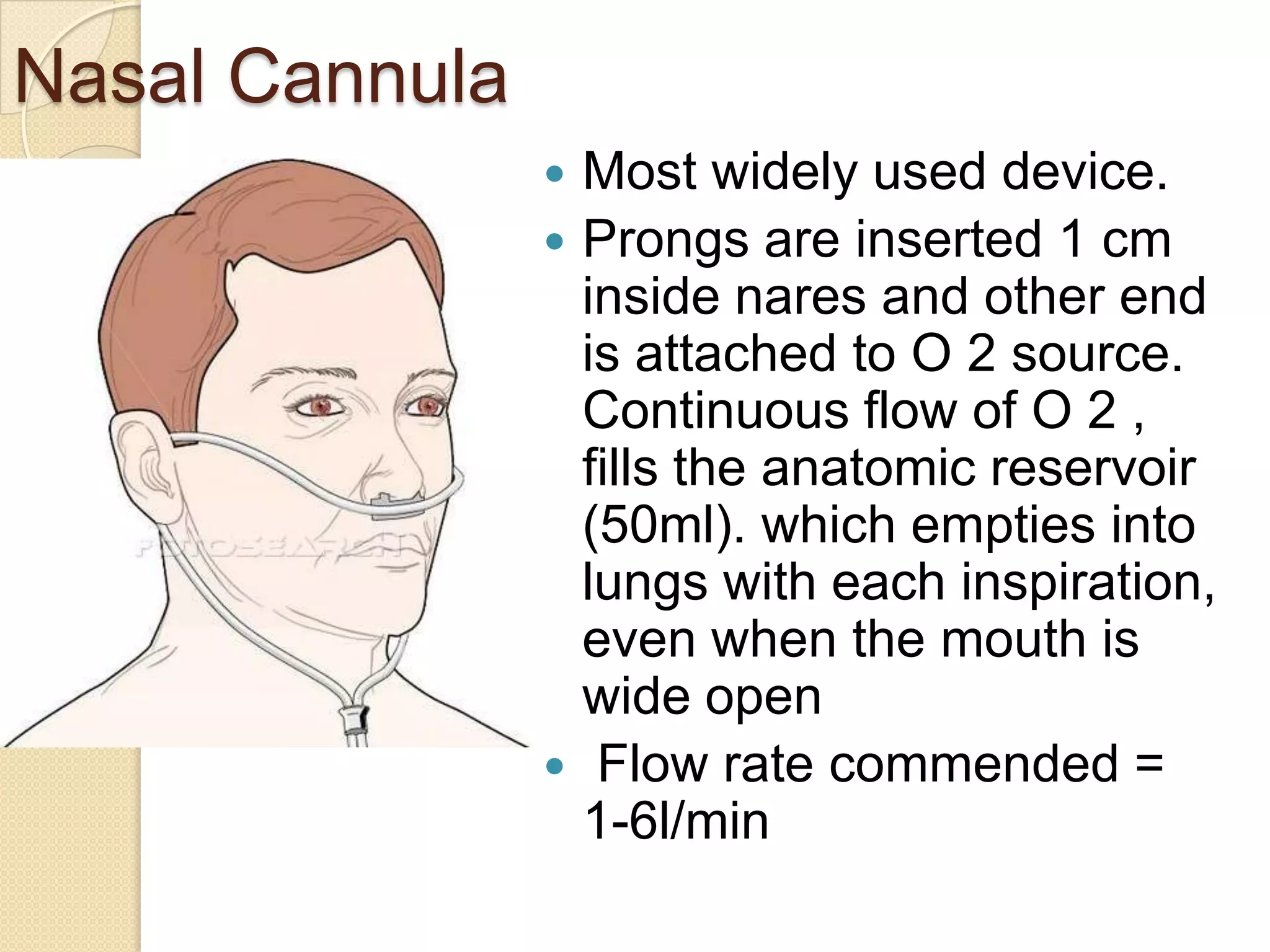
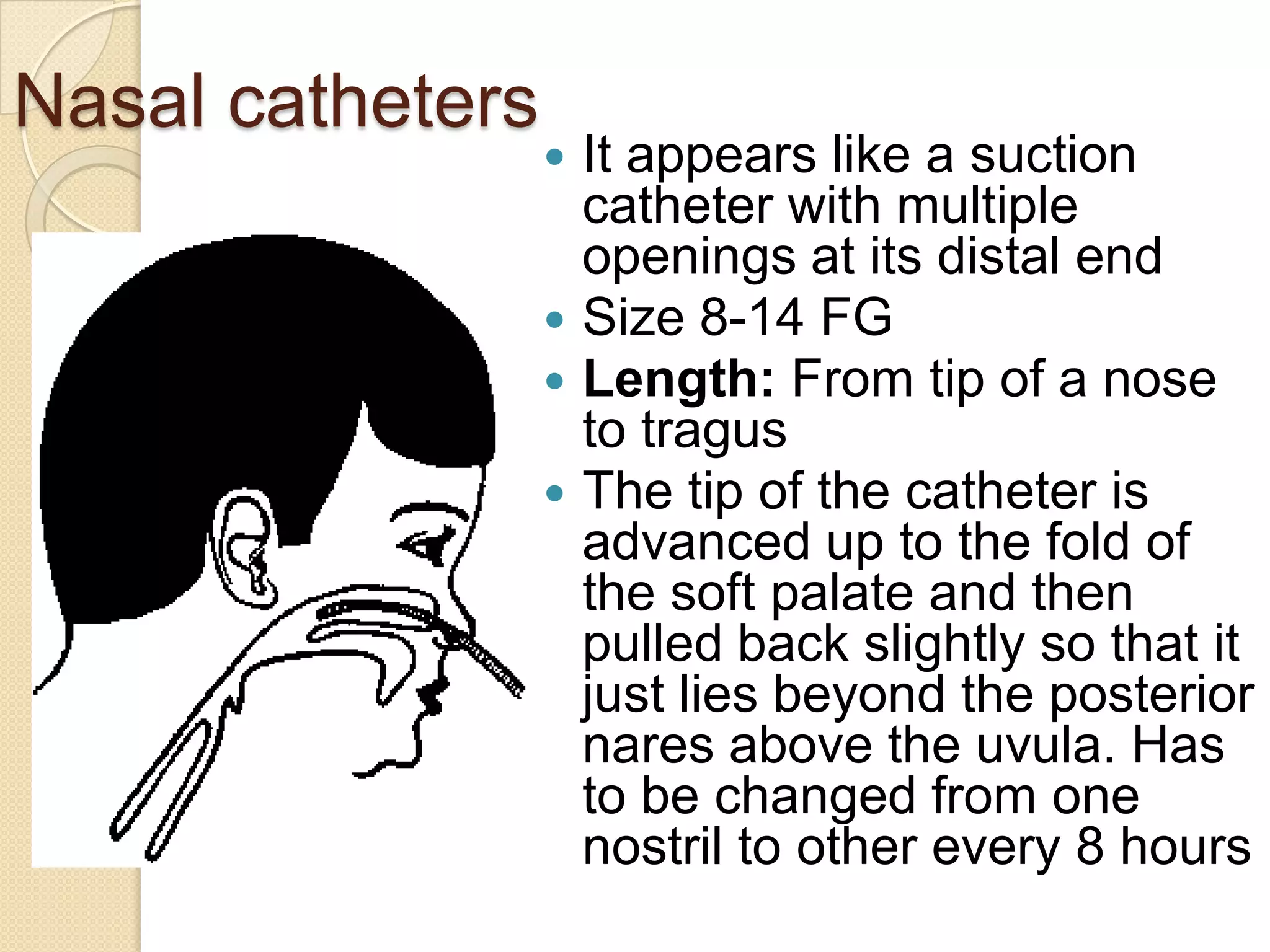
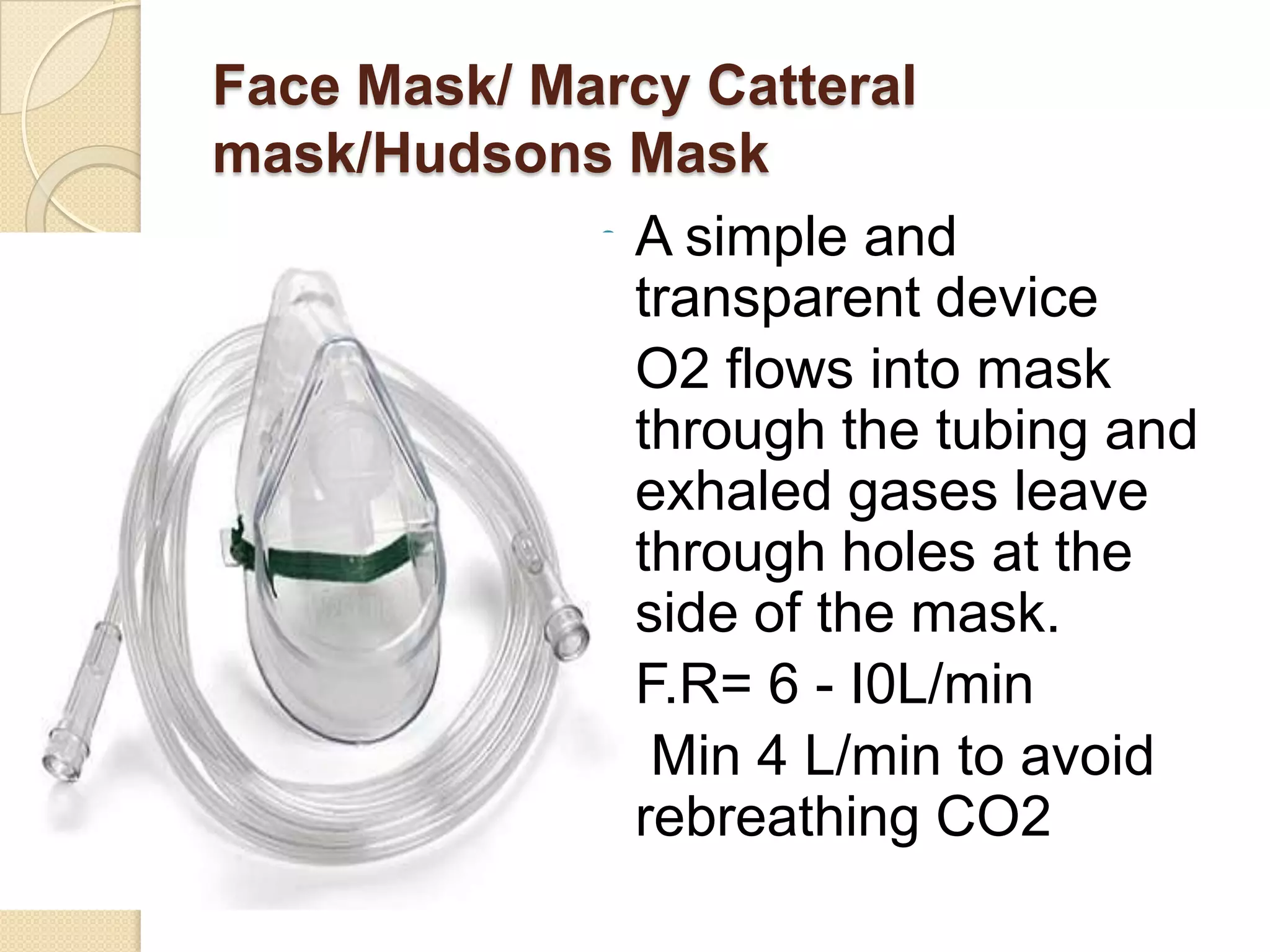
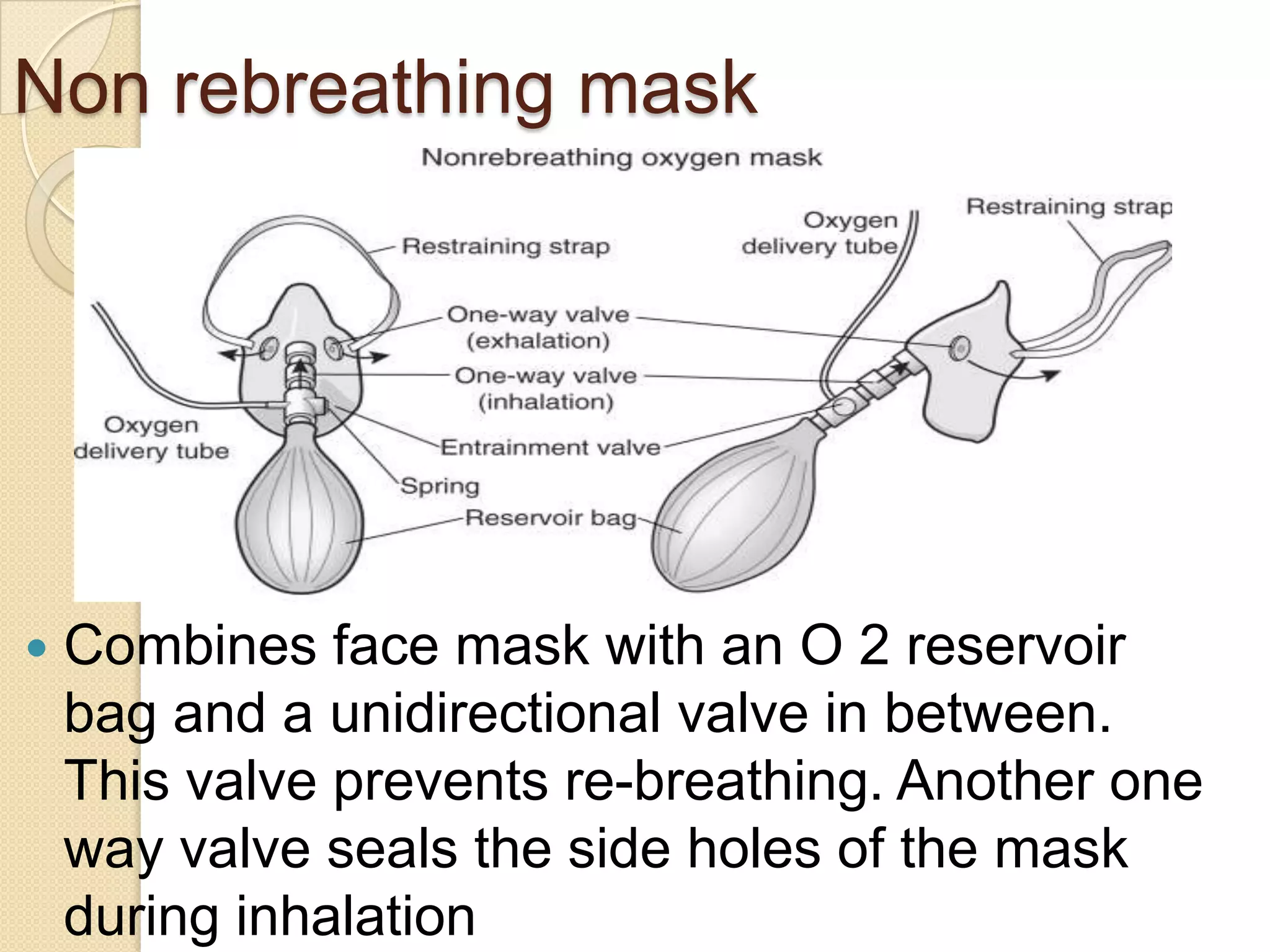
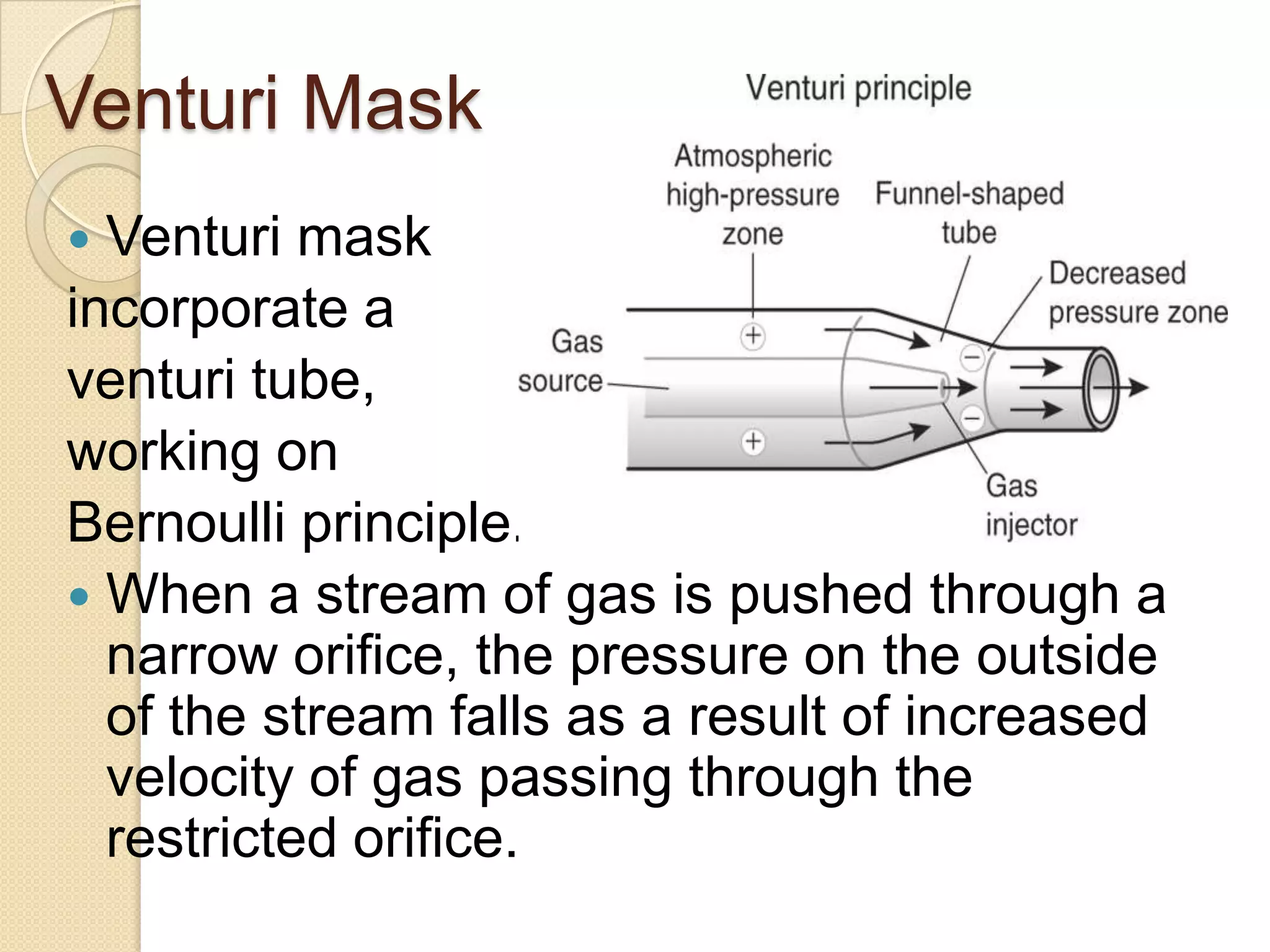
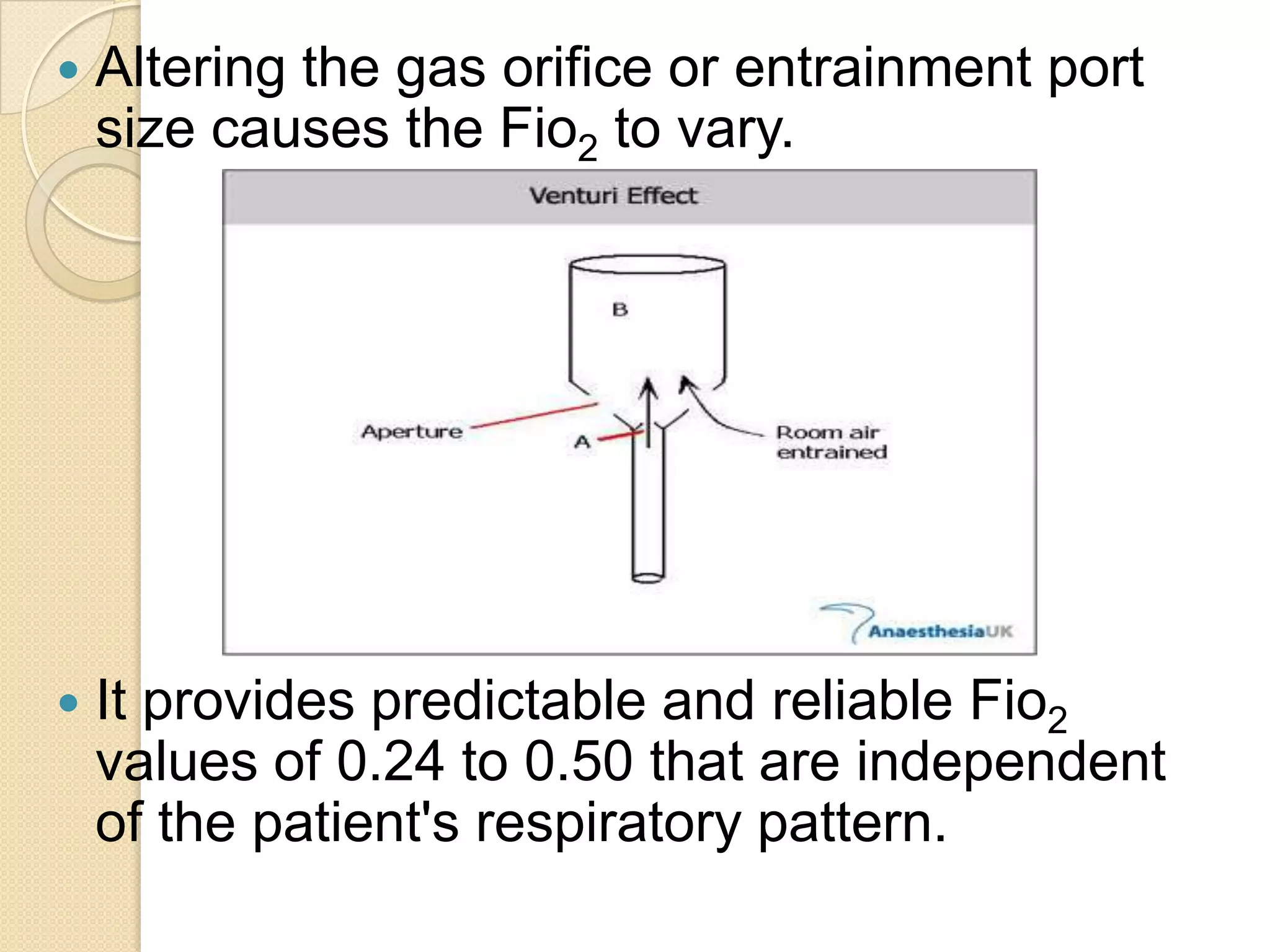
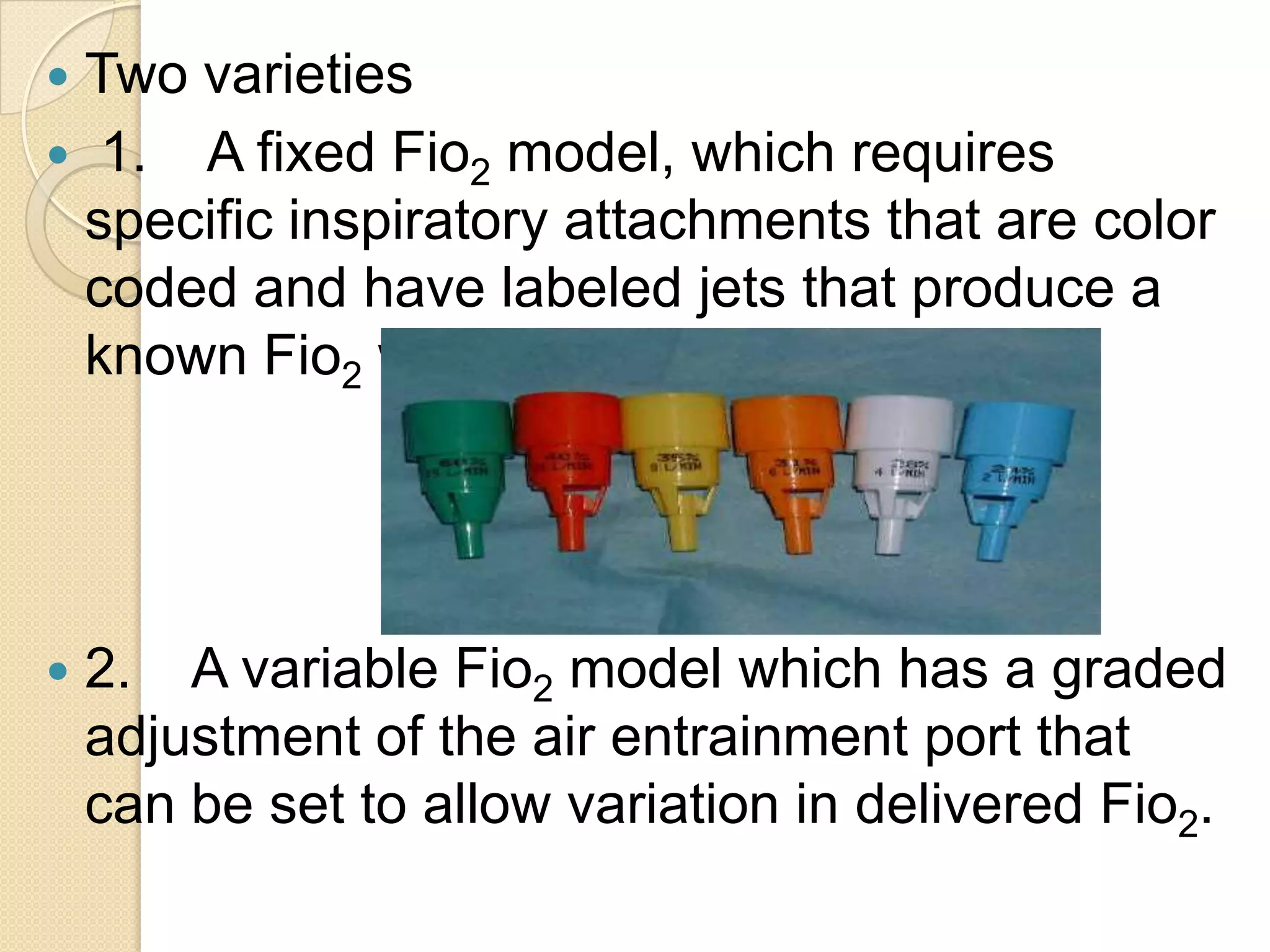
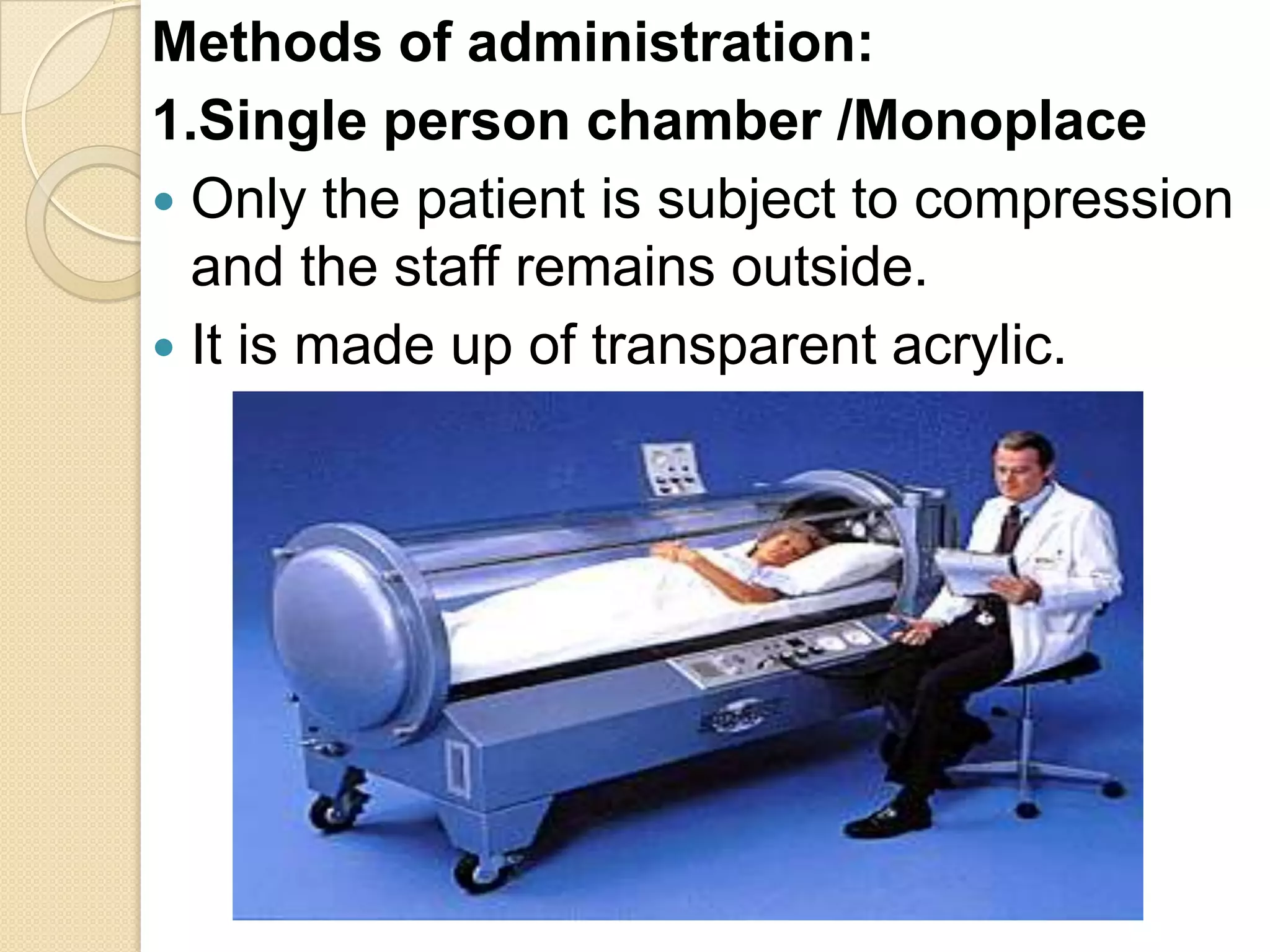
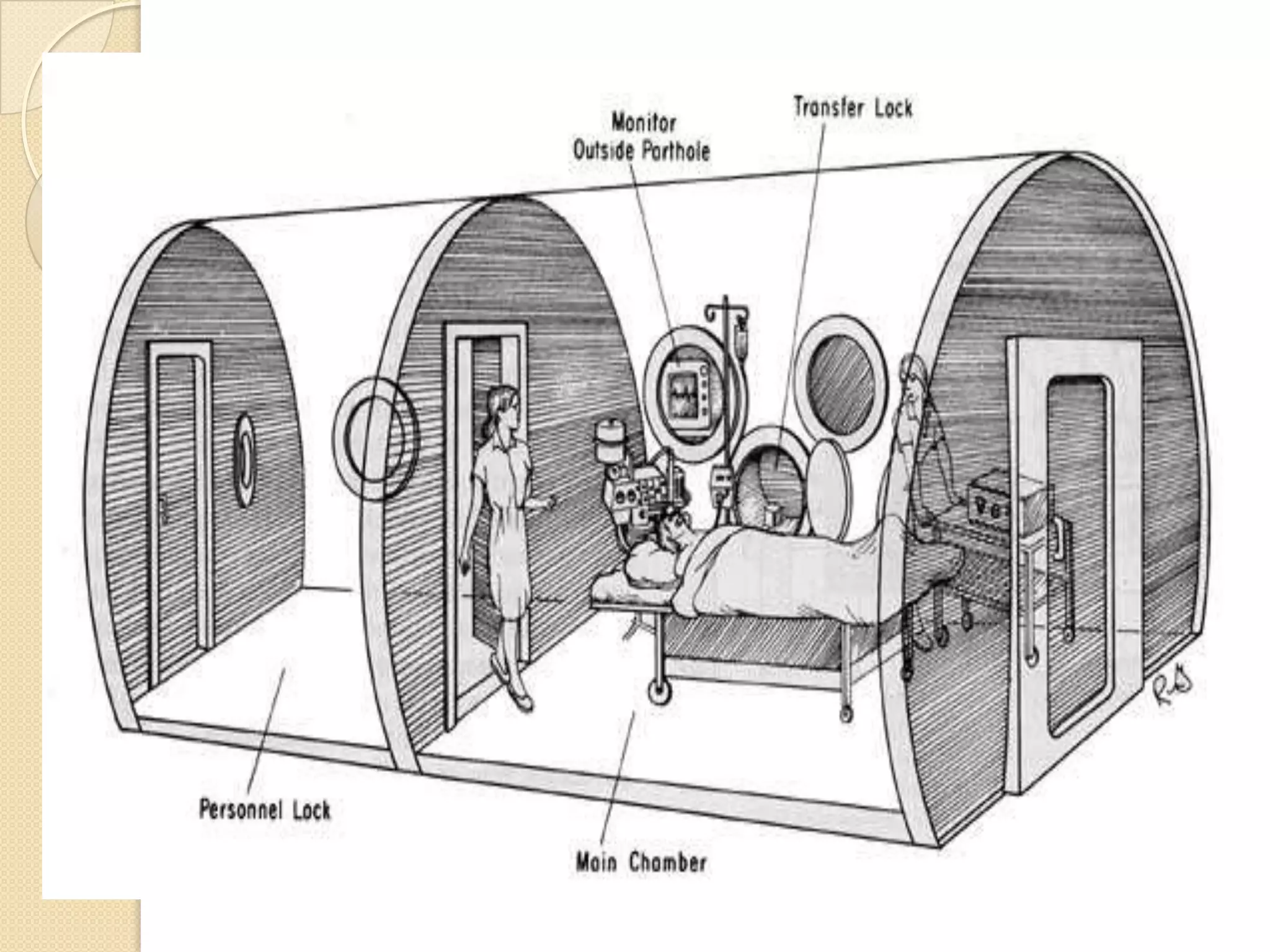
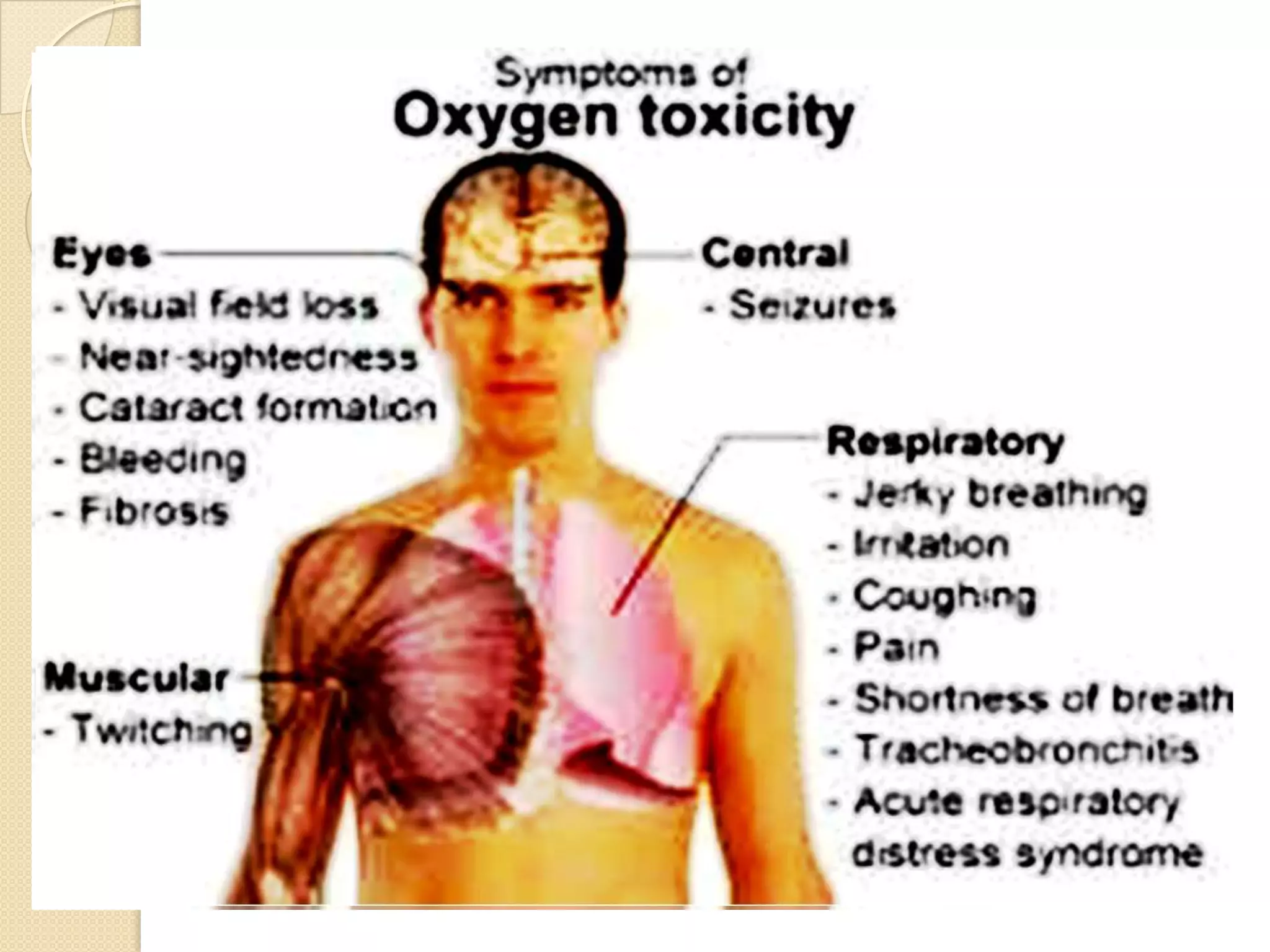
This document provides information on nitrous oxide, oxygen, and hyperbaric oxygen. It discusses the discovery and early uses of nitrous oxide as an anesthetic. It describes the preparation, properties, administration and physiological effects of nitrous oxide. Potential side effects are outlined including effects on the central nervous system, circulation, ventilation, and bone marrow. The document also discusses the discovery, production, transport and cascade of oxygen in the body. Various methods of oxygen therapy are described.