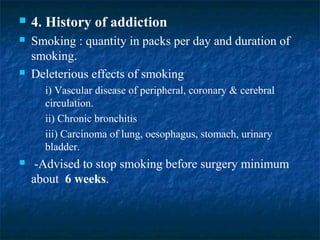
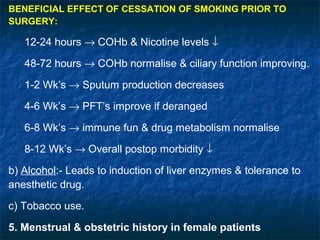
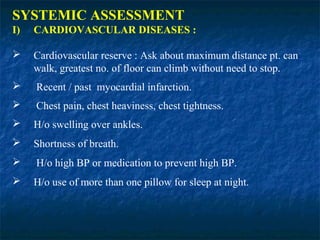
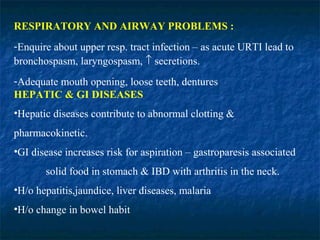
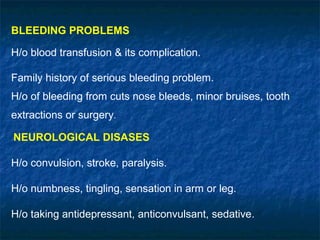
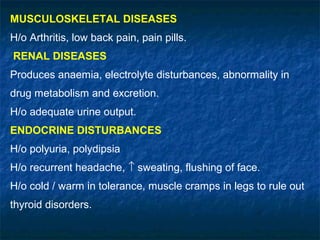
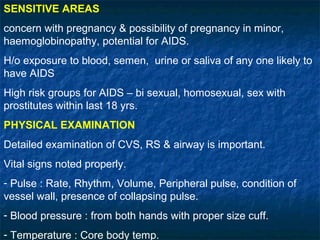
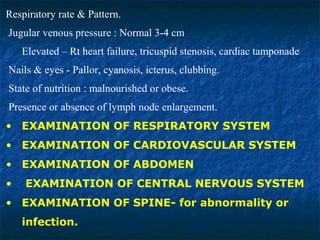
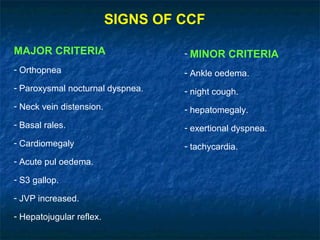
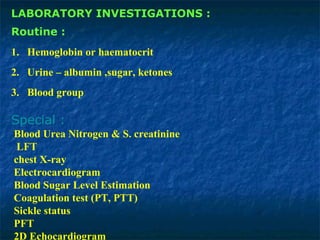
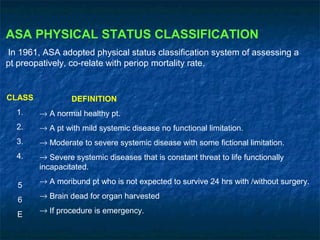
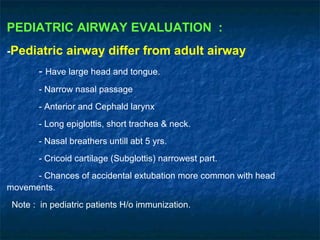
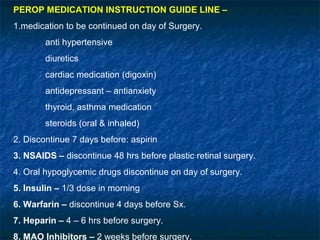
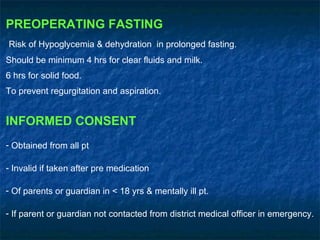
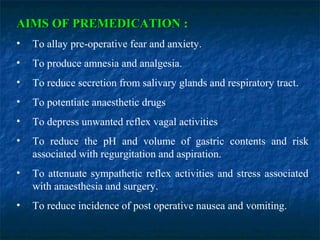
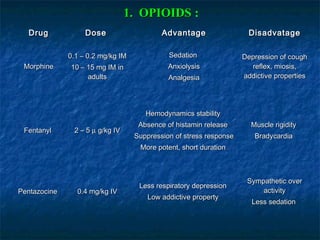
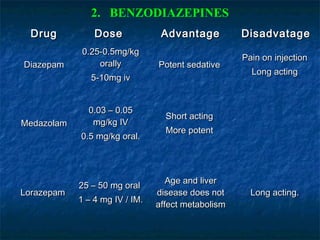
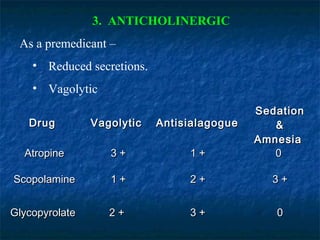
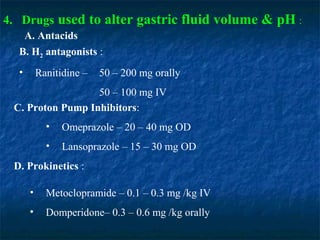
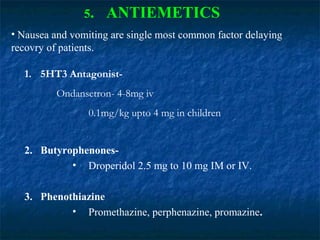
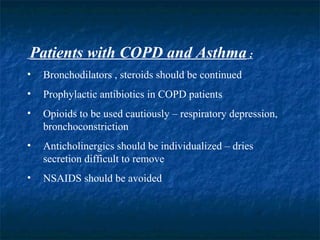
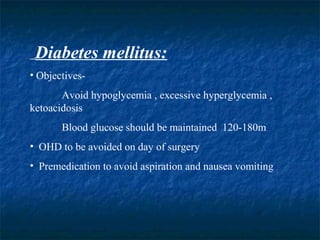
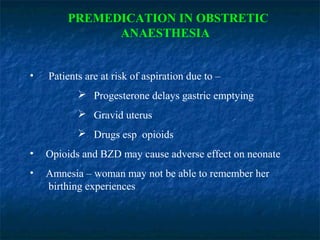
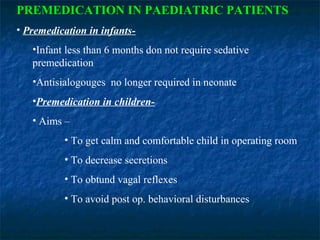
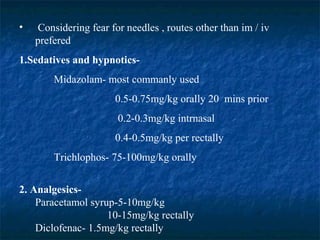
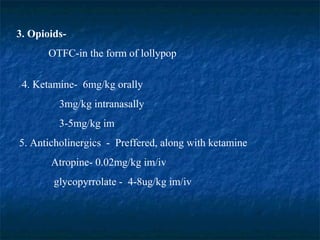
This document provides information on pre-anesthetic checkups and premedication. It discusses the goals of preoperative medical assessment which include reducing surgery morbidity, increasing perioperative care quality while decreasing costs, and helping the patient return to function quickly. It covers topics like history taking, physical examination, laboratory investigations, ASA physical status classification, pediatric considerations, medication guidelines, preoperative fasting, and informed consent. Common premedication drugs are also outlined along with their advantages and disadvantages.