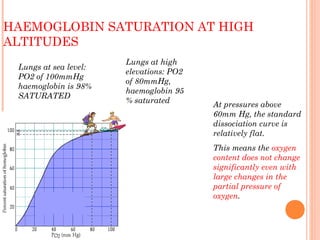
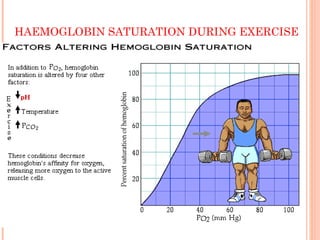
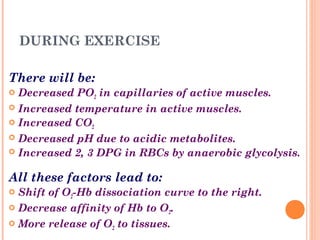
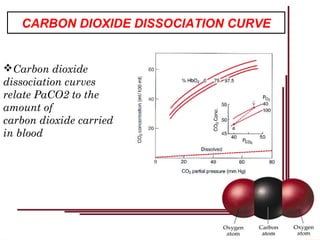
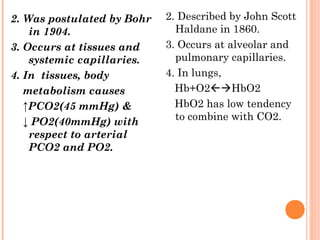
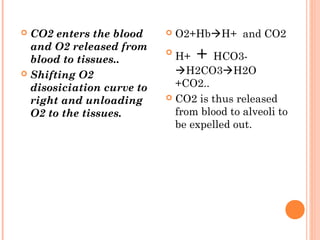
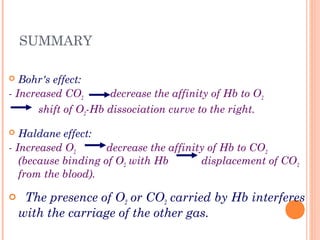
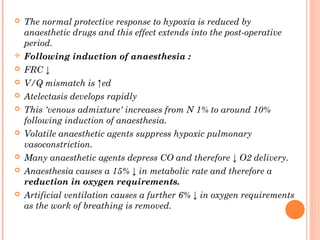
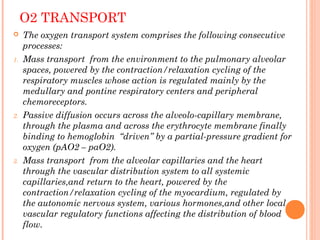
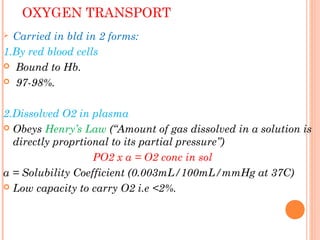
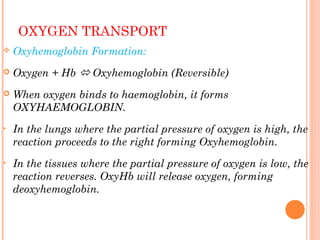
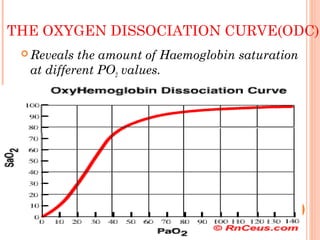
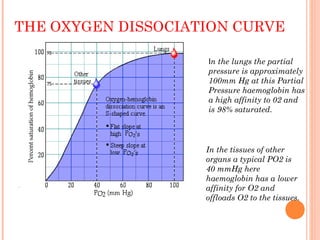
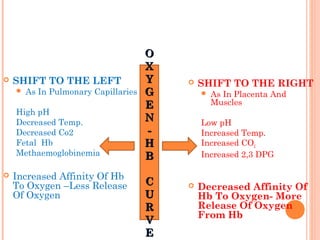
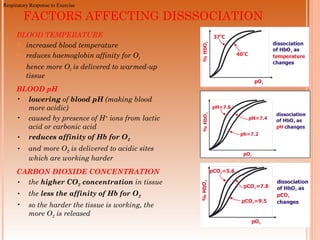
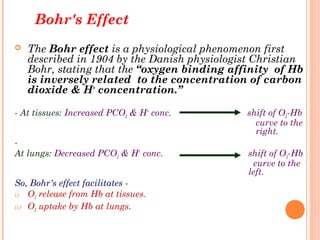
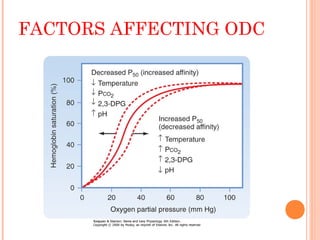
Following induction of anesthesia, factors such as decreased functional residual capacity, increased ventilation/perfusion mismatching, and development of atelectasis can increase venous admixture from 1% to around 10%. Anesthetic agents also suppress hypoxic pulmonary vasoconstriction and decrease cardiac output, reducing oxygen delivery. However, anesthesia and artificial ventilation lower oxygen requirements by around 15-21% due to decreased metabolism and work of breathing. Oxygen is transported in the blood bound to hemoglobin or dissolved in plasma, and the oxygen dissociation curve illustrates hemoglobin's changing affinity for oxygen at different partial pressures. Multiple factors can shift this curve, facilitating either oxygen loading or unloading as needed.

![CONTD..
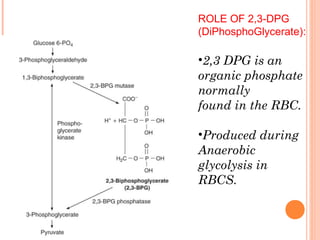
2,3 DPG has a tendency to bind to β chains
of Hb and thereby decrease the affinity of
Hemoglobin for oxygen.
HbO2 + 2,3 DPG → Hb-2,3 DPG +
O2
It promotes a rightward shift and
enhances oxygen unloading at the tissues.
This shift is longer in duration than that
due to [H+] or PCO2 or temperature.](https://image.slidesharecdn.com/oxygendissociationcurve-170720115931/85/Oxygen-dissociation-curve-28-320.jpg)
![•
EFFECTS OF ANEMIA & CARBON MONOXIDE ON
THE OXYGEN DISSOCIATION CURVE
↓O2 content.
SaO2remains normal
Carbon Monoxide [CO]
affinity of Hb for CO is 250
fold relative to O2 competes
with O2 binding
L shift- interfere with O2
unloading at tissues causing
severe tissue hypoxia.
Sigmoidal HbO2 curve
becomes Hyperbolic.](https://image.slidesharecdn.com/oxygendissociationcurve-170720115931/85/Oxygen-dissociation-curve-35-320.jpg)