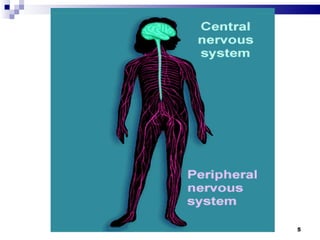
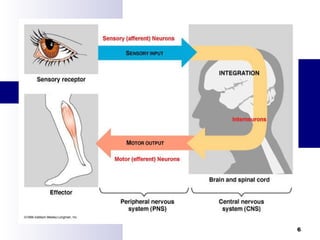
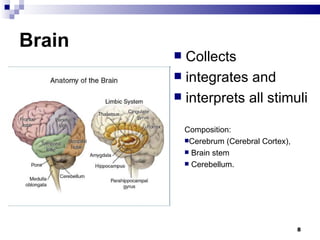
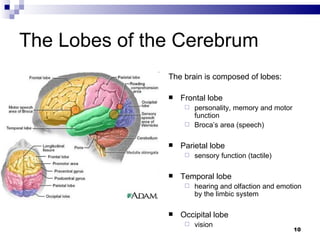
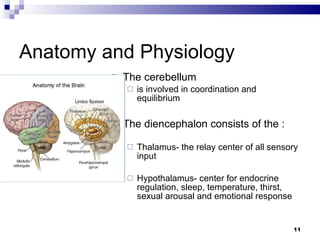
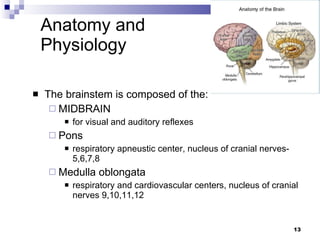
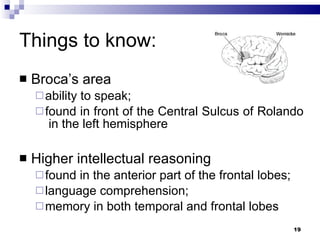
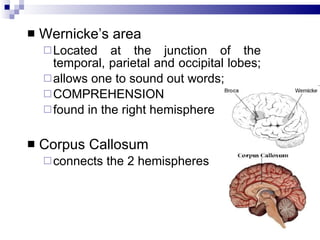
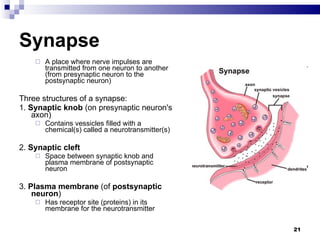
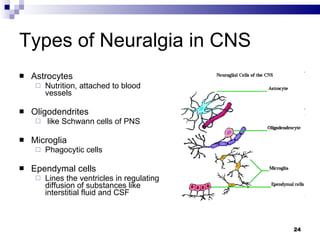
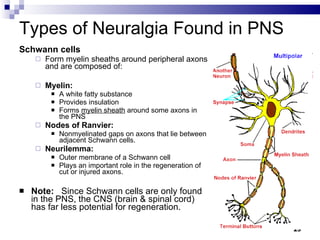
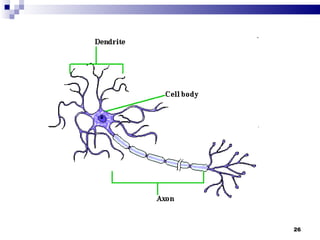
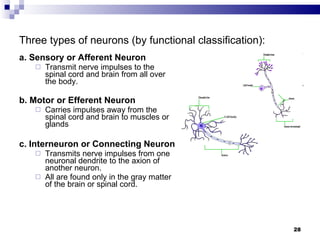
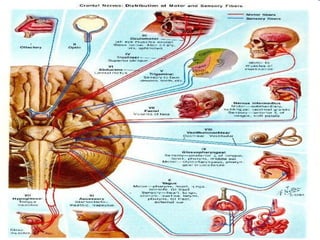
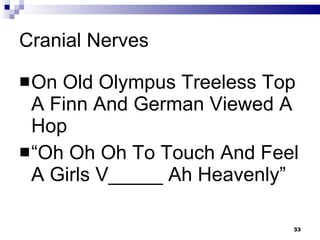
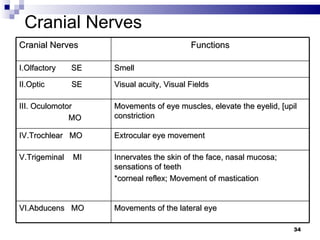
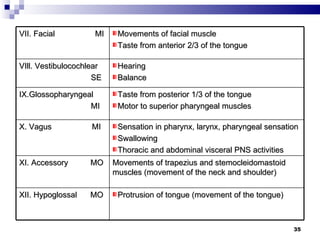
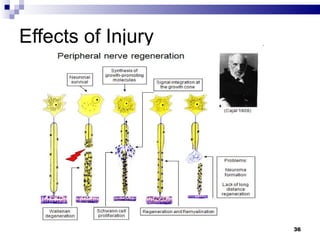
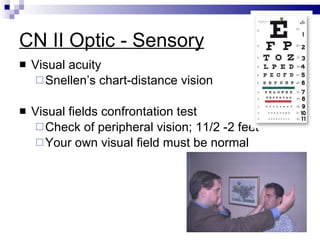
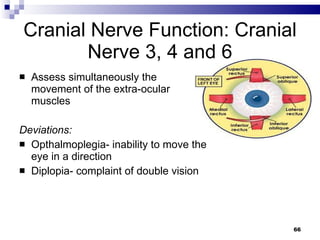
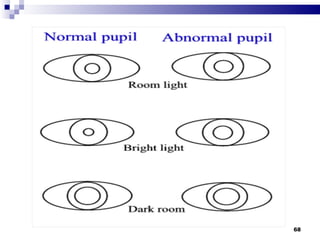
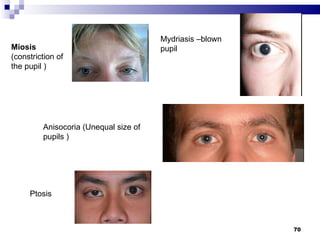
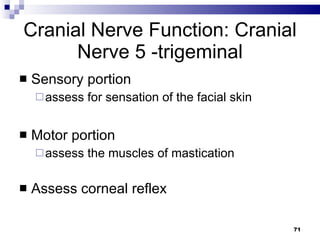
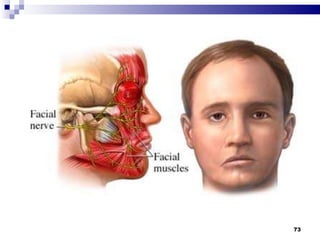
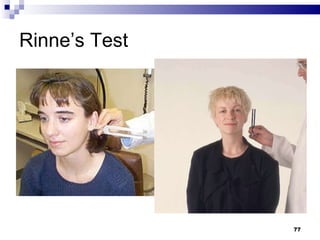
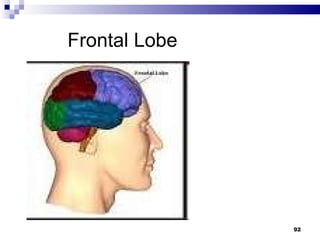
The document discusses the structure and function of the nervous system. It describes the central nervous system including the brain and spinal cord. It discusses the lobes of the cerebrum and their functions. It also describes the peripheral nervous system, autonomic nervous system, neurons, neuroglia cells, neurotransmitters, and the 12 pairs of cranial nerves.