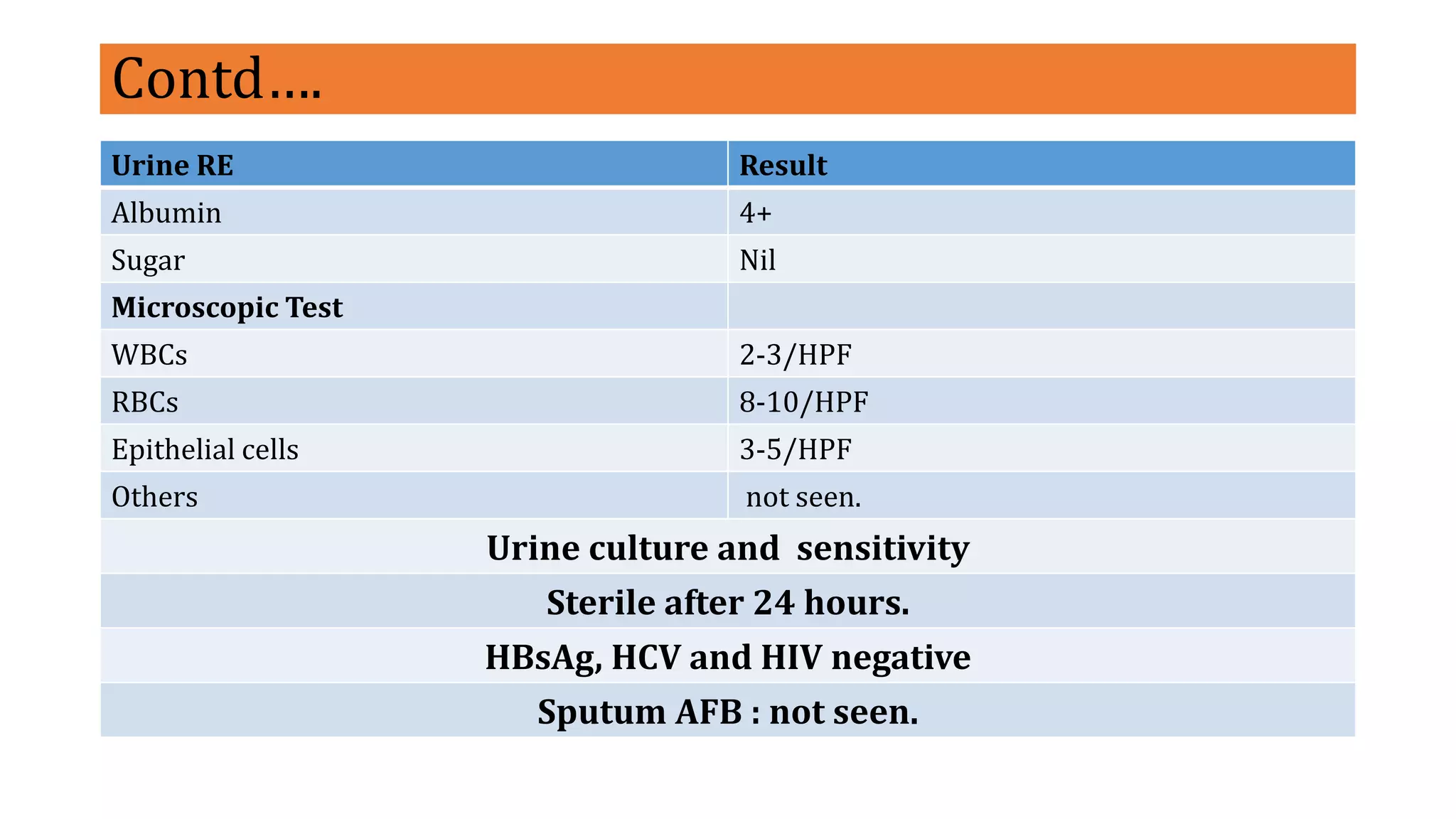
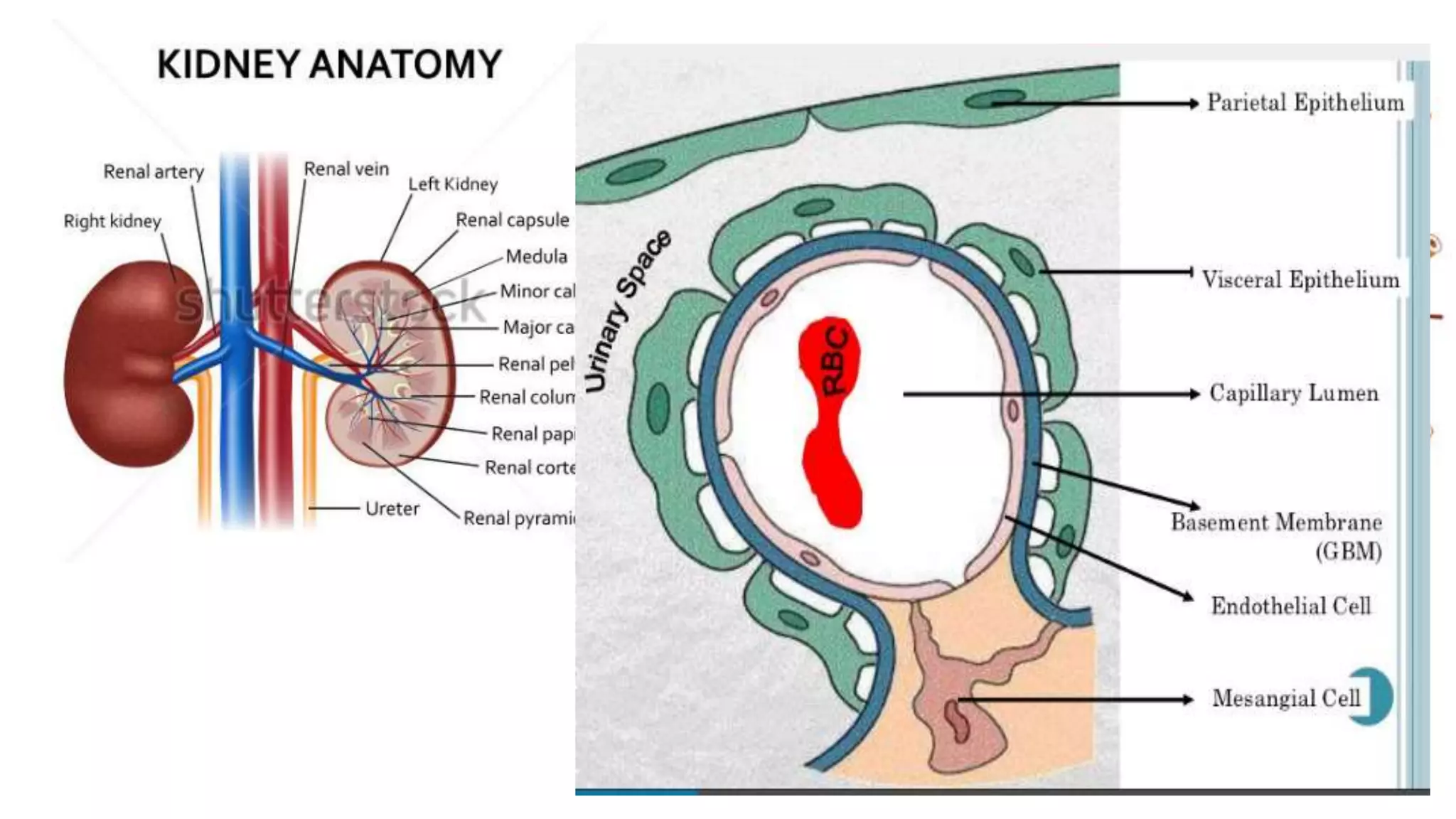
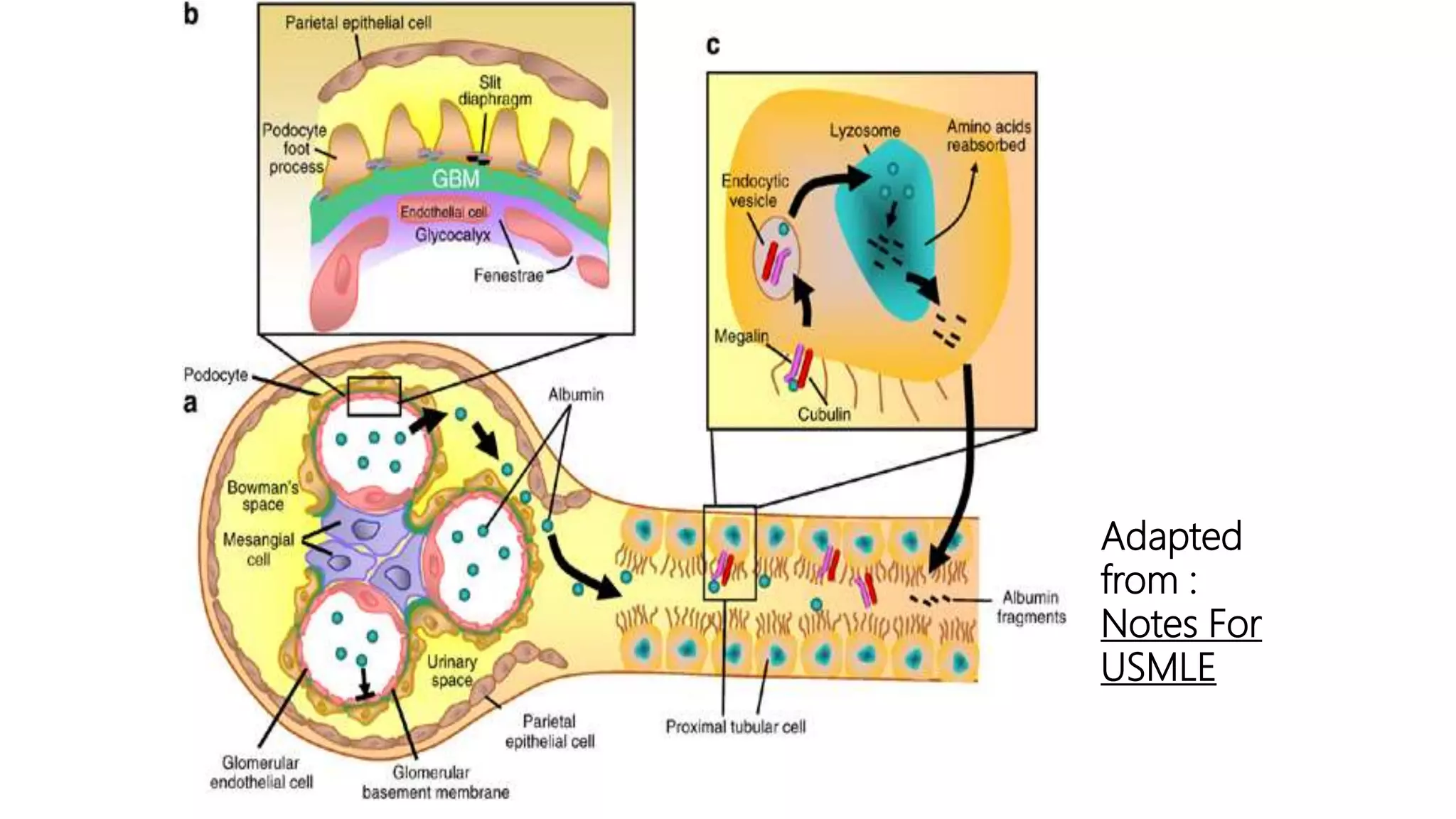
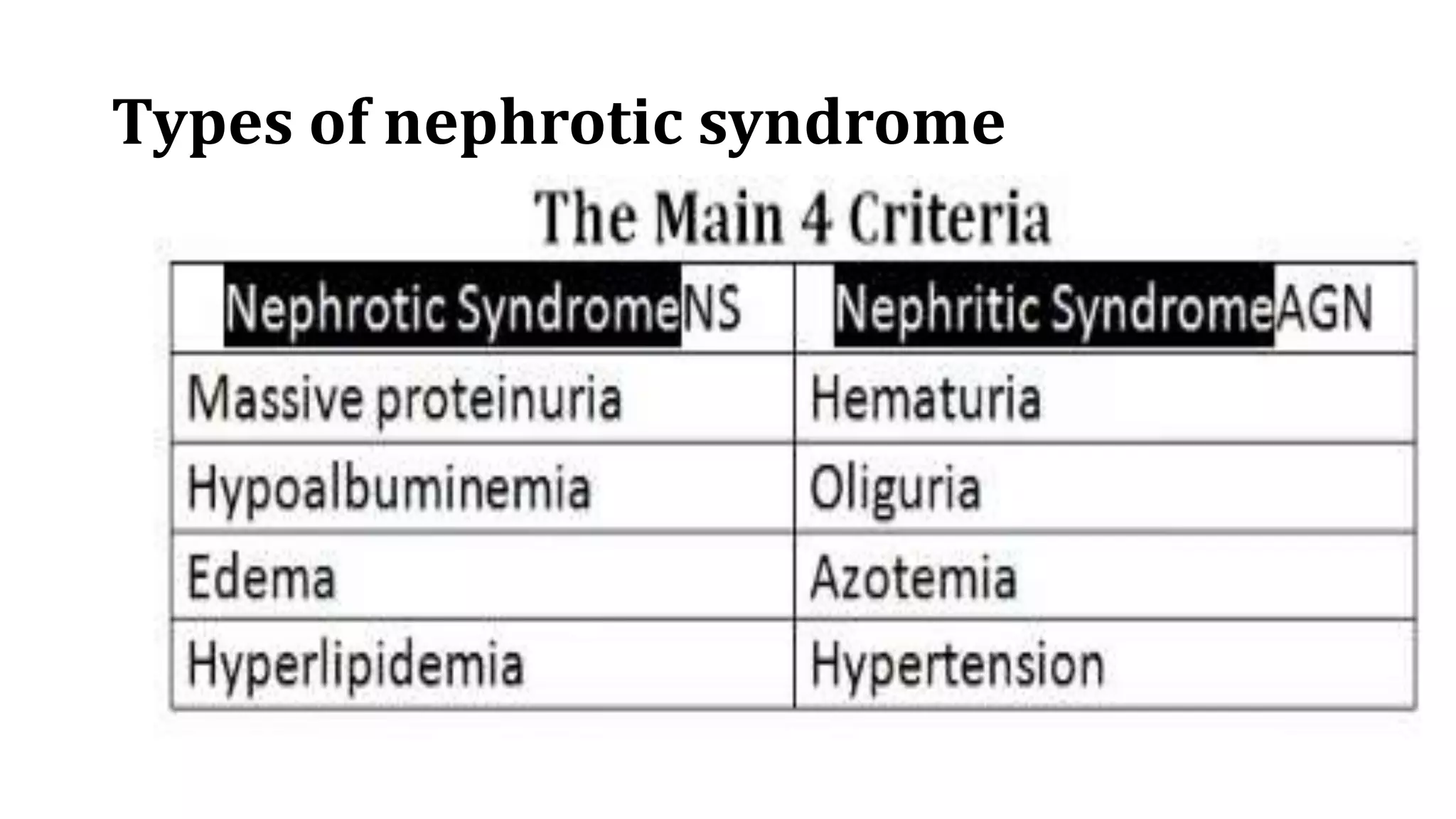
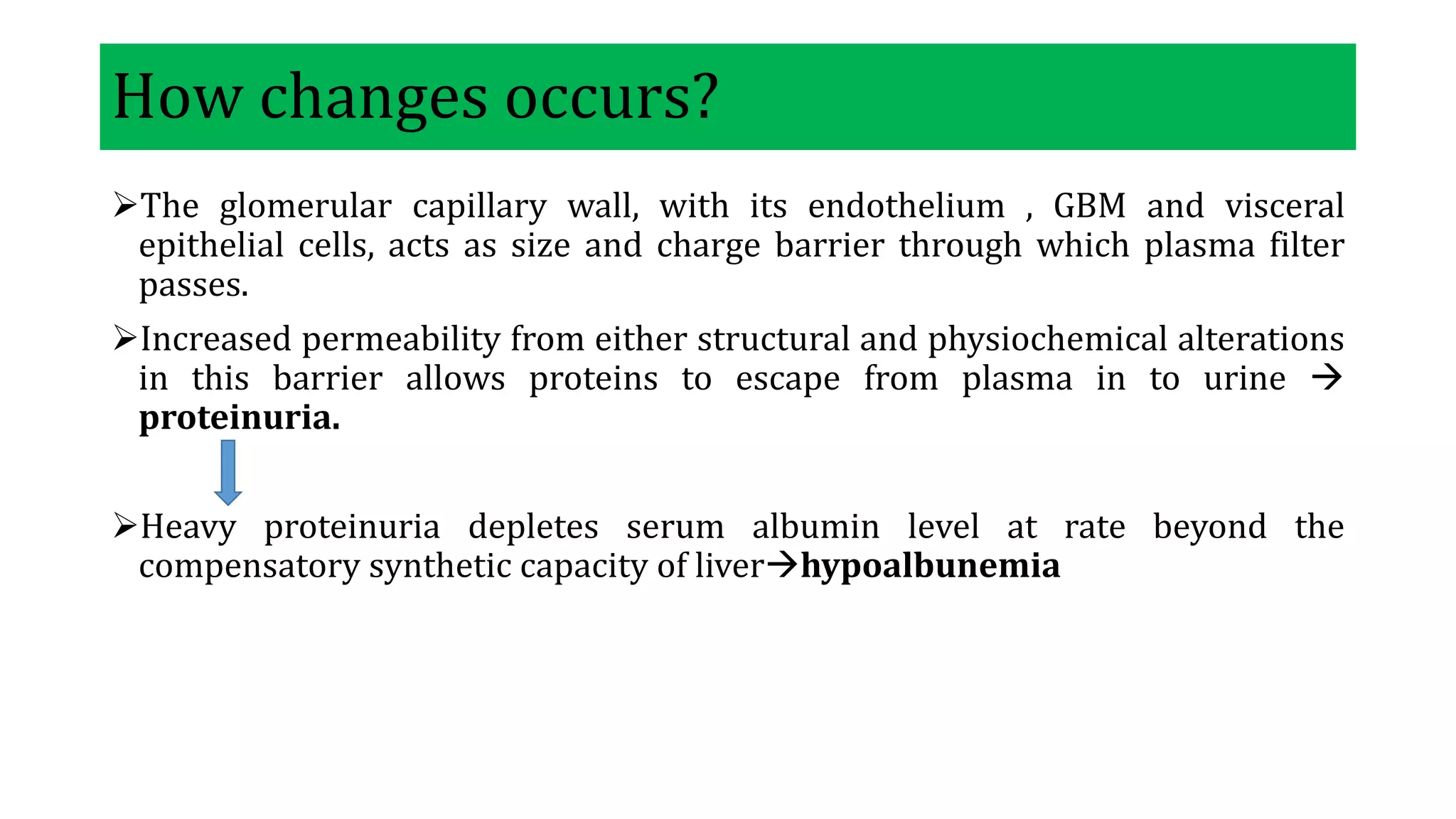
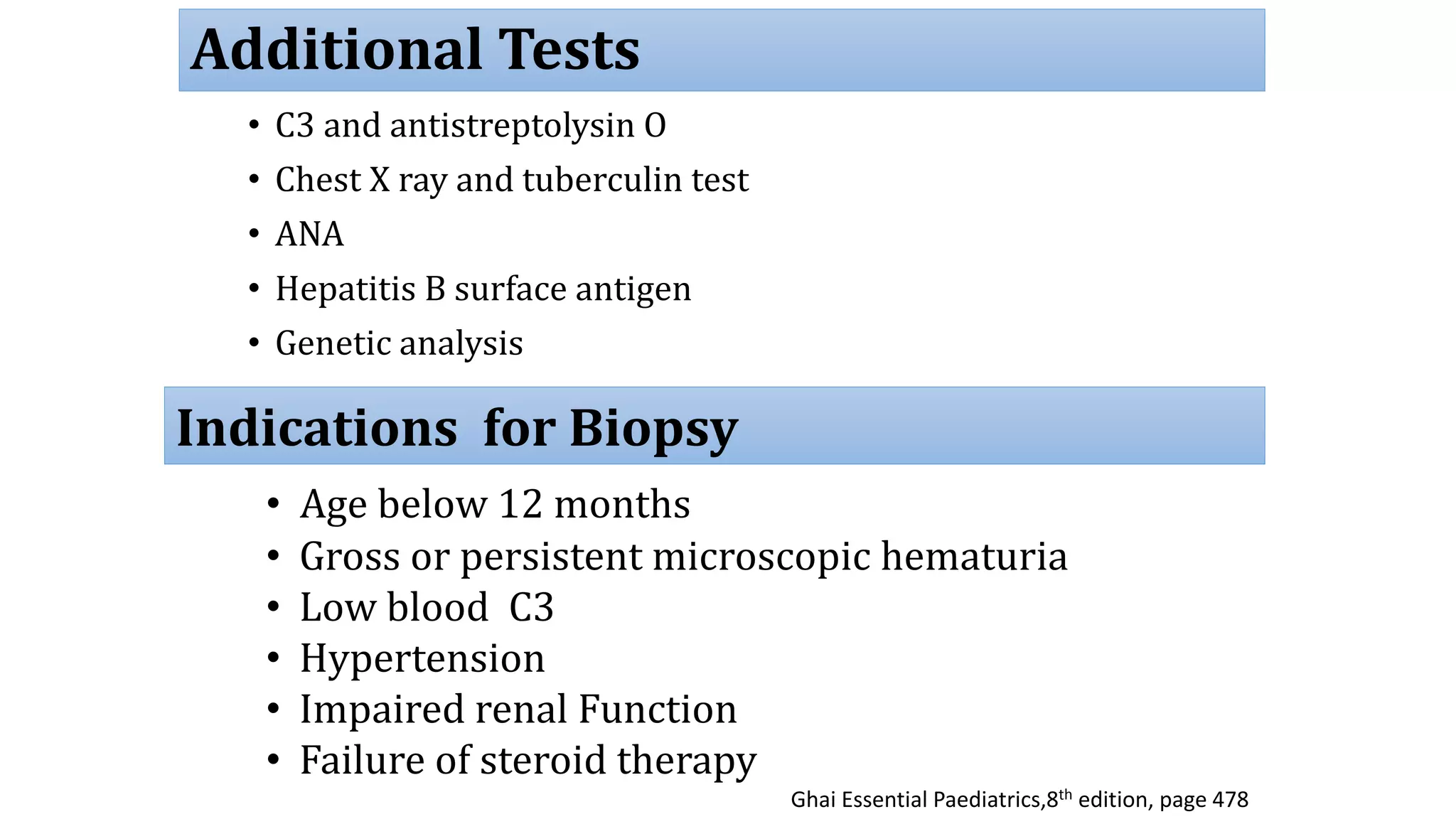
This case study describes a 2.5 year old male child presenting with generalized swelling of the body for 5 days. On examination, facial puffiness and pitting edema of the limbs were observed. Laboratory investigations found nephrotic range proteinuria, hypoalbuminemia, and hyperlipidemia. A preliminary diagnosis of nephrotic syndrome, likely minimal change disease, was made. The child was started on treatment and further investigation with a renal biopsy was recommended to confirm the diagnosis.