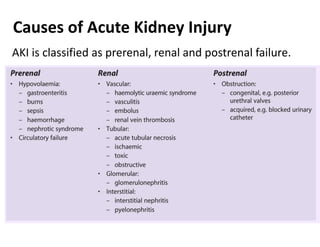
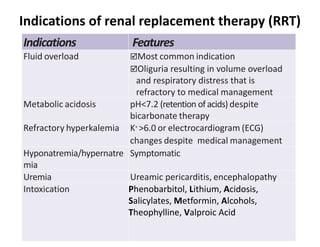
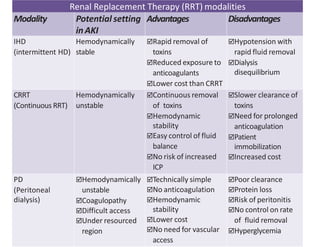
Acute Kidney Injury (AKI) is an acute impairment of renal function resulting in retention of waste products. It is classified as Stage I, II or III based on increases in serum creatinine and decreases in urine output. AKI can be prerenal, renal or postrenal and has various causes like dehydration, infections and medications. Treatment involves fluid management, nutritional support, treating complications, renal replacement therapy like hemodialysis if needed, and follow-up to monitor for residual or chronic kidney disease.