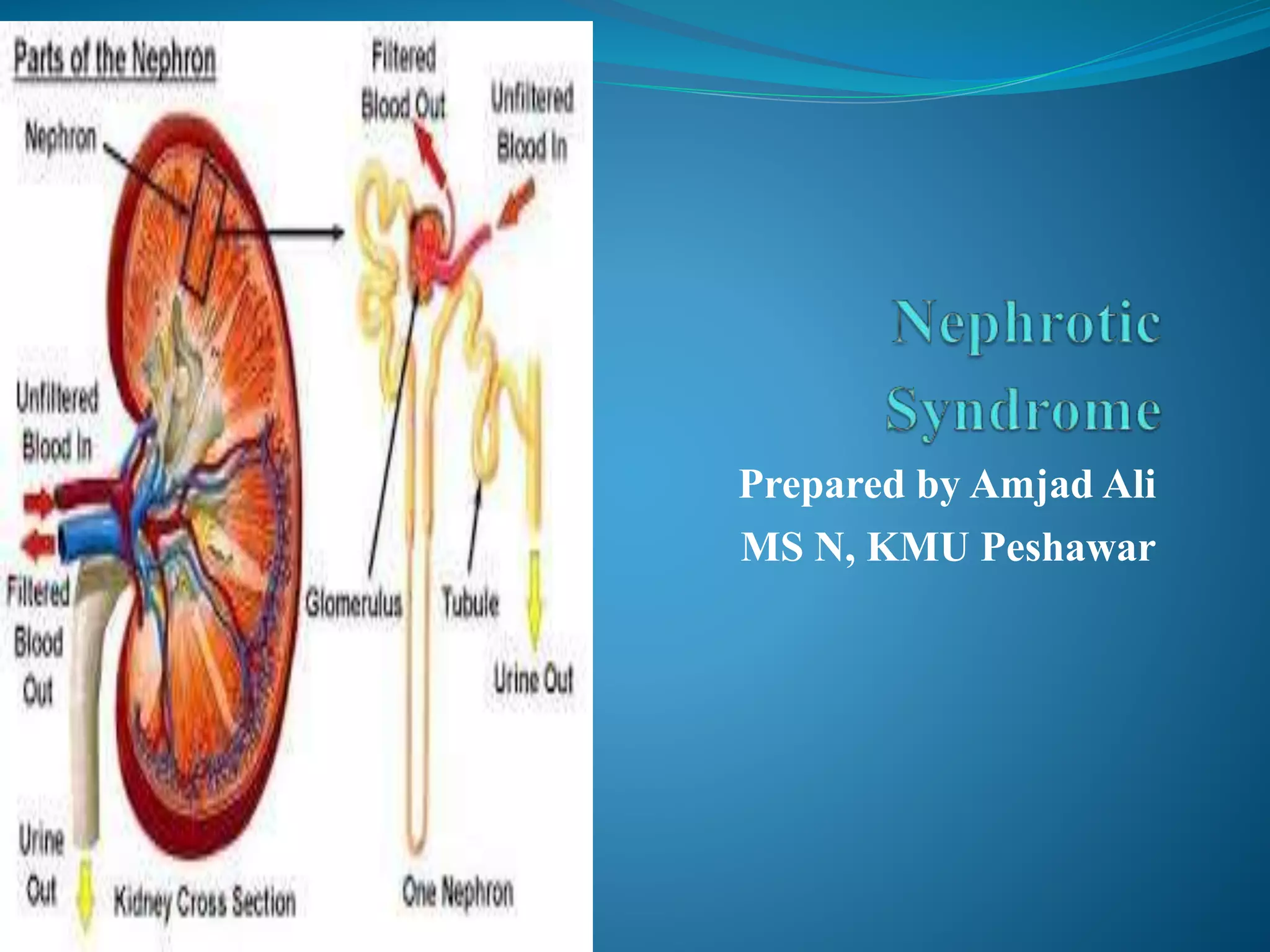
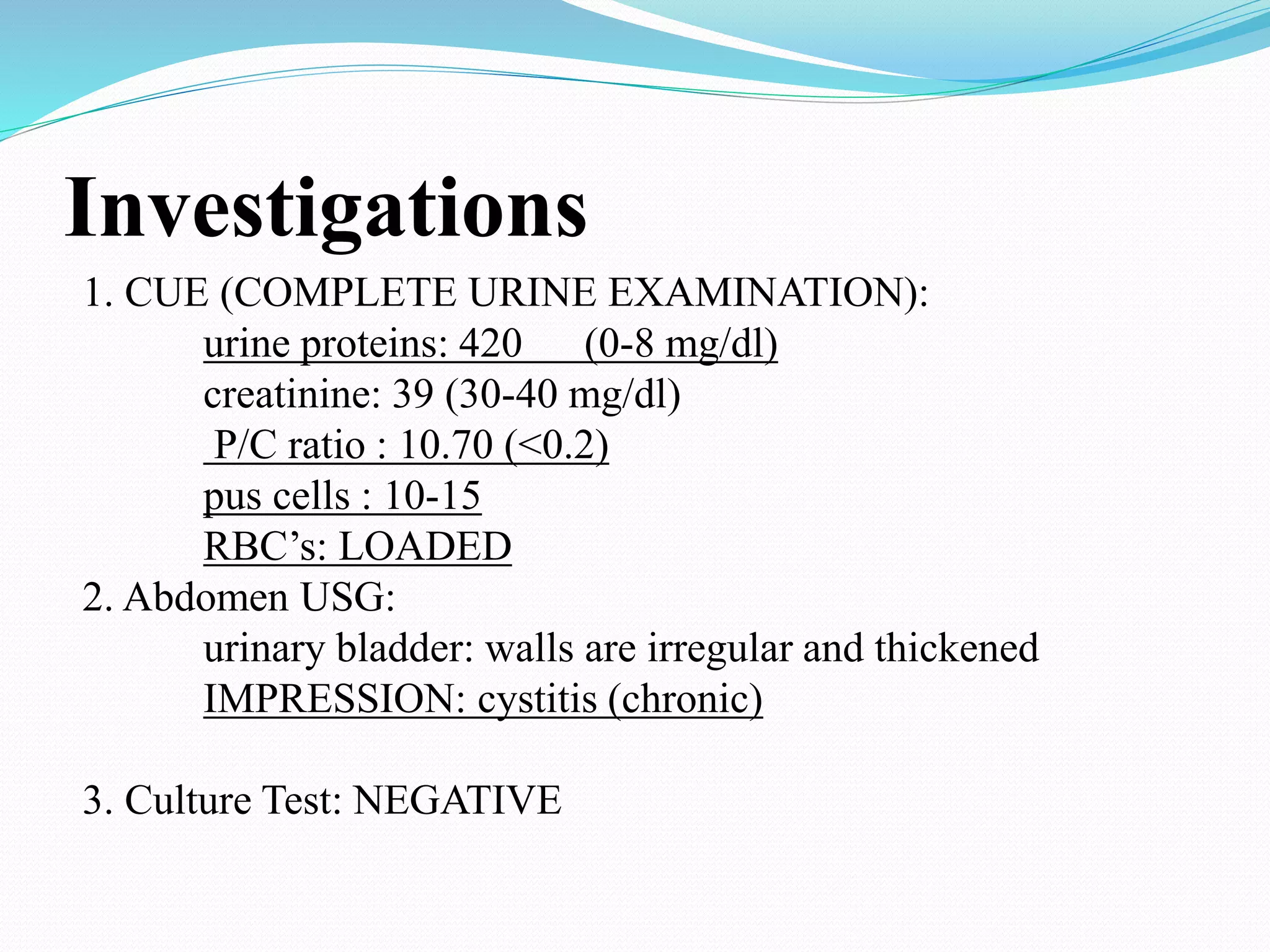
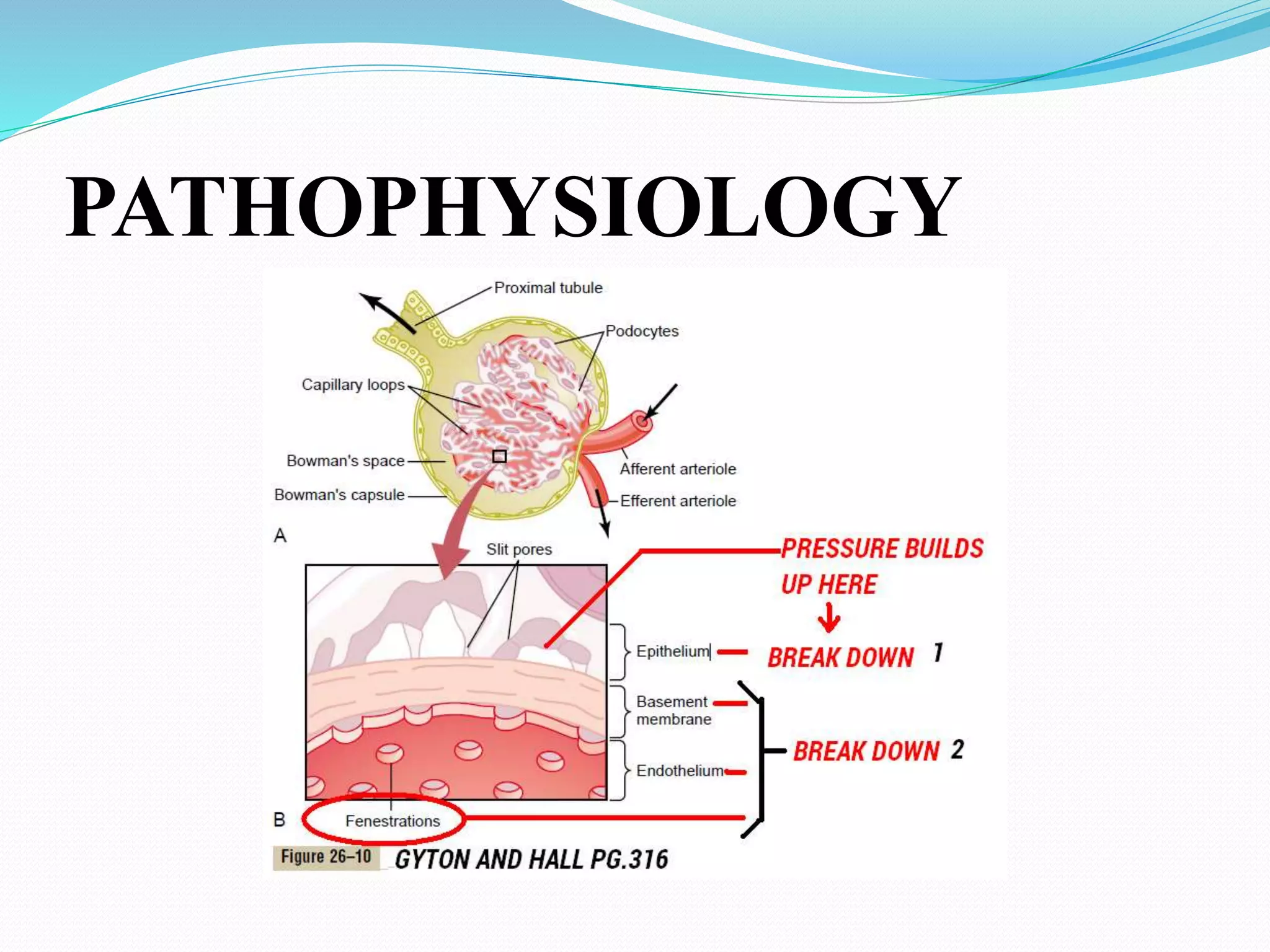
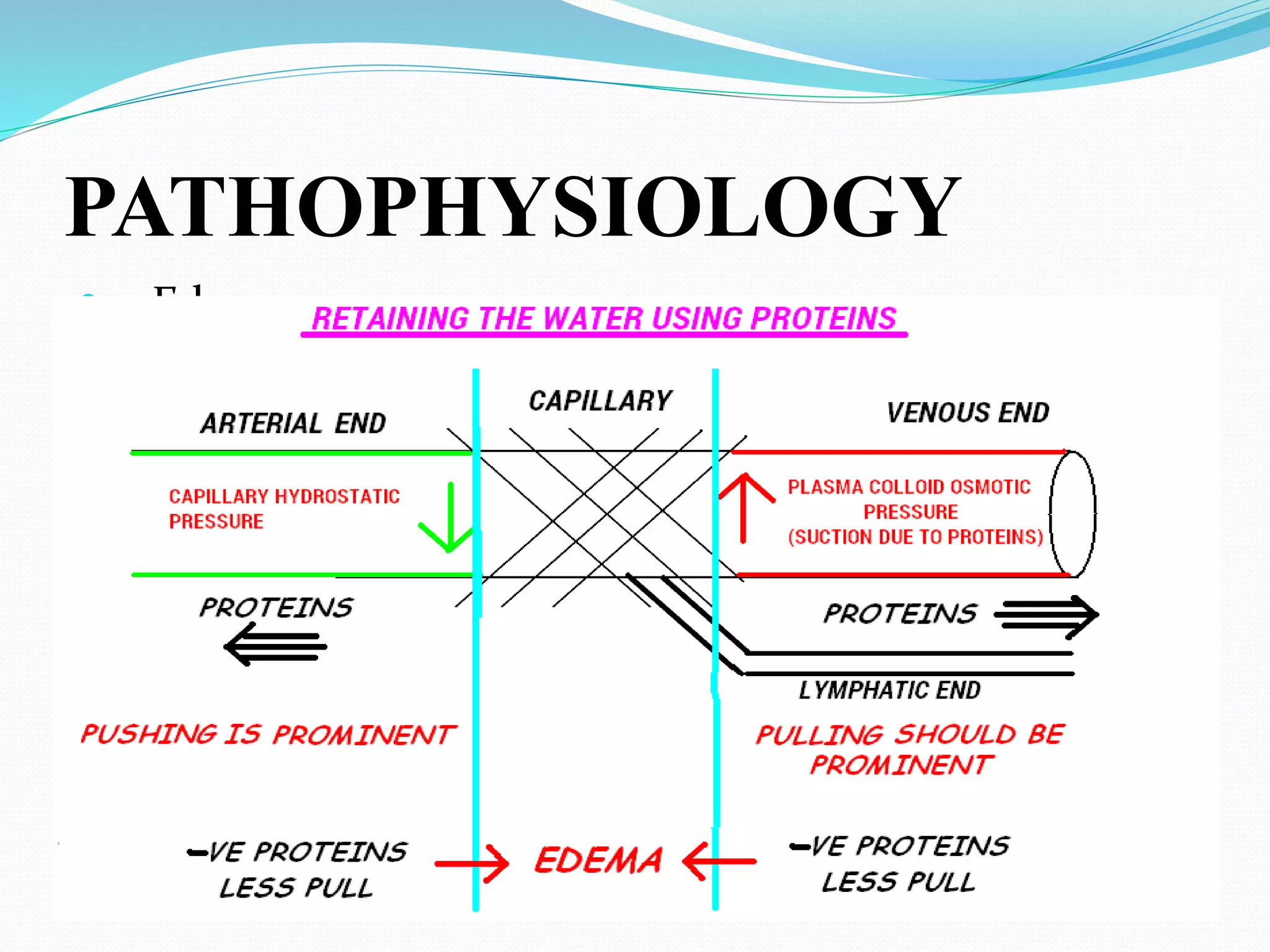
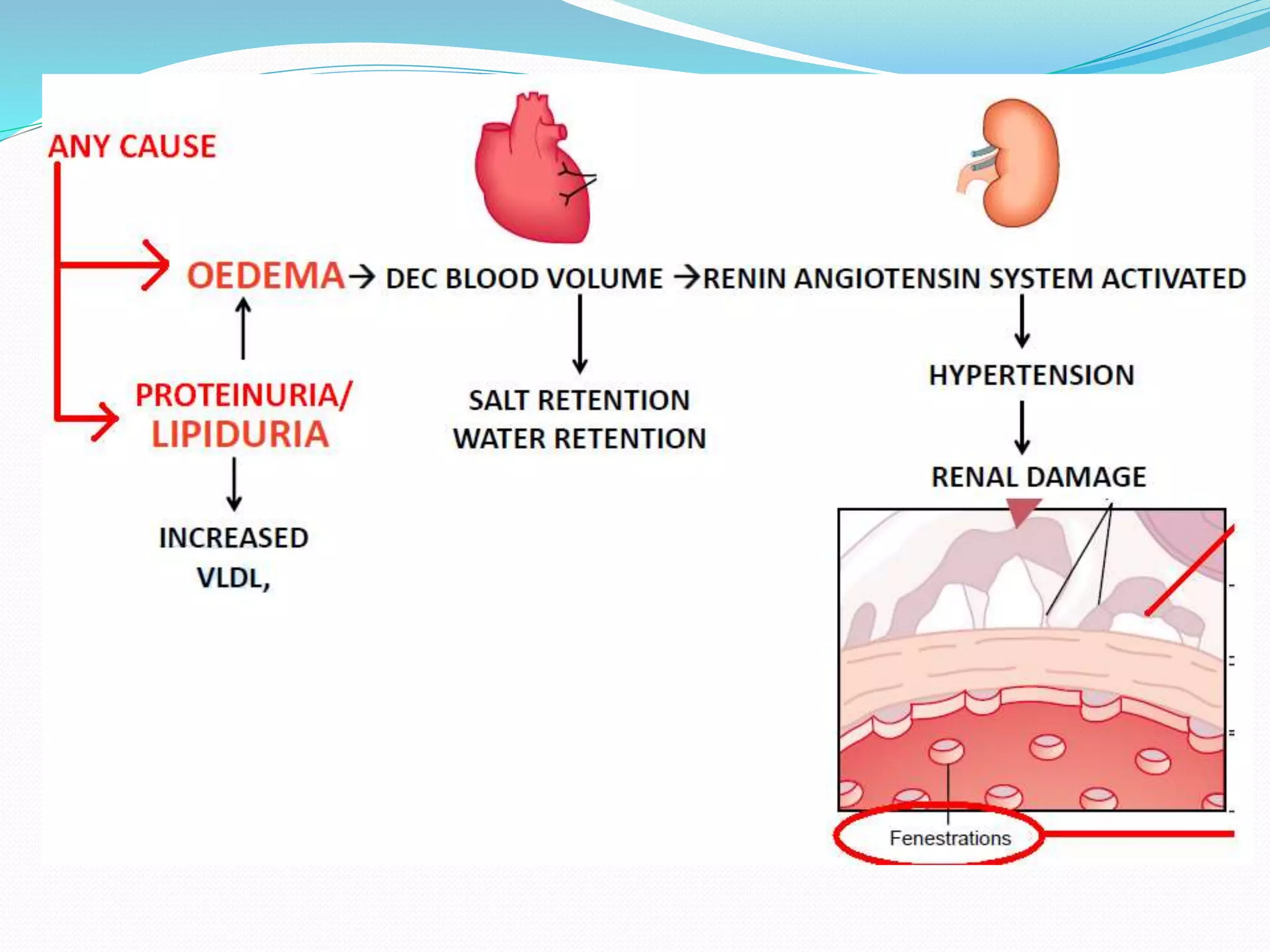
A 6-year-old male child was admitted to the pediatric ward with hematuria and burning urination. Tests revealed protein in his urine and thickened bladder walls on ultrasound. This is consistent with chronic cystitis. The document goes on to define nephrotic syndrome, discuss its pathophysiology, incidence, etiology including genetic and secondary causes, clinical features, lab investigations, management including diet and steroids, complications, and nursing considerations like monitoring intake/output and administering medications.