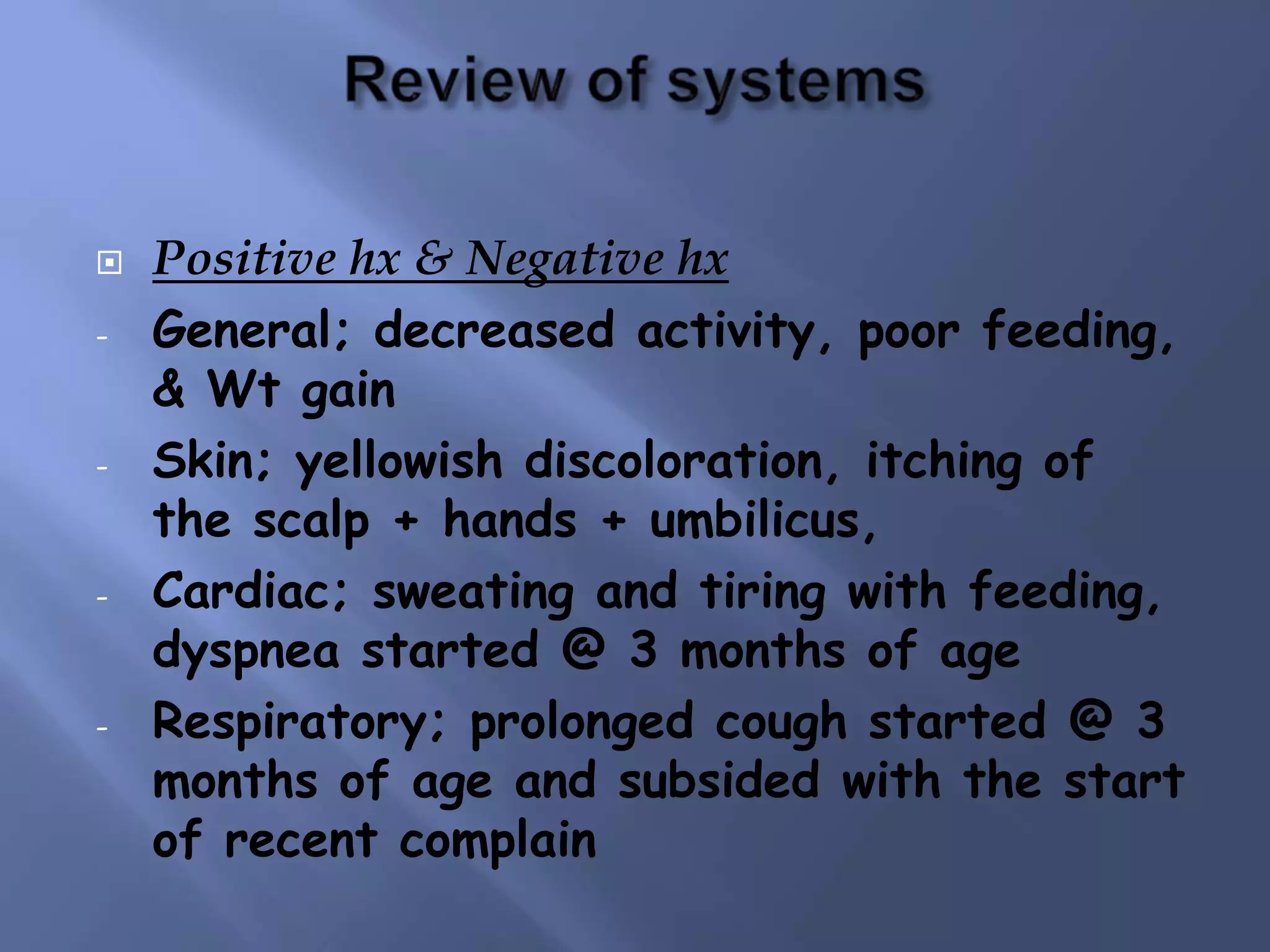
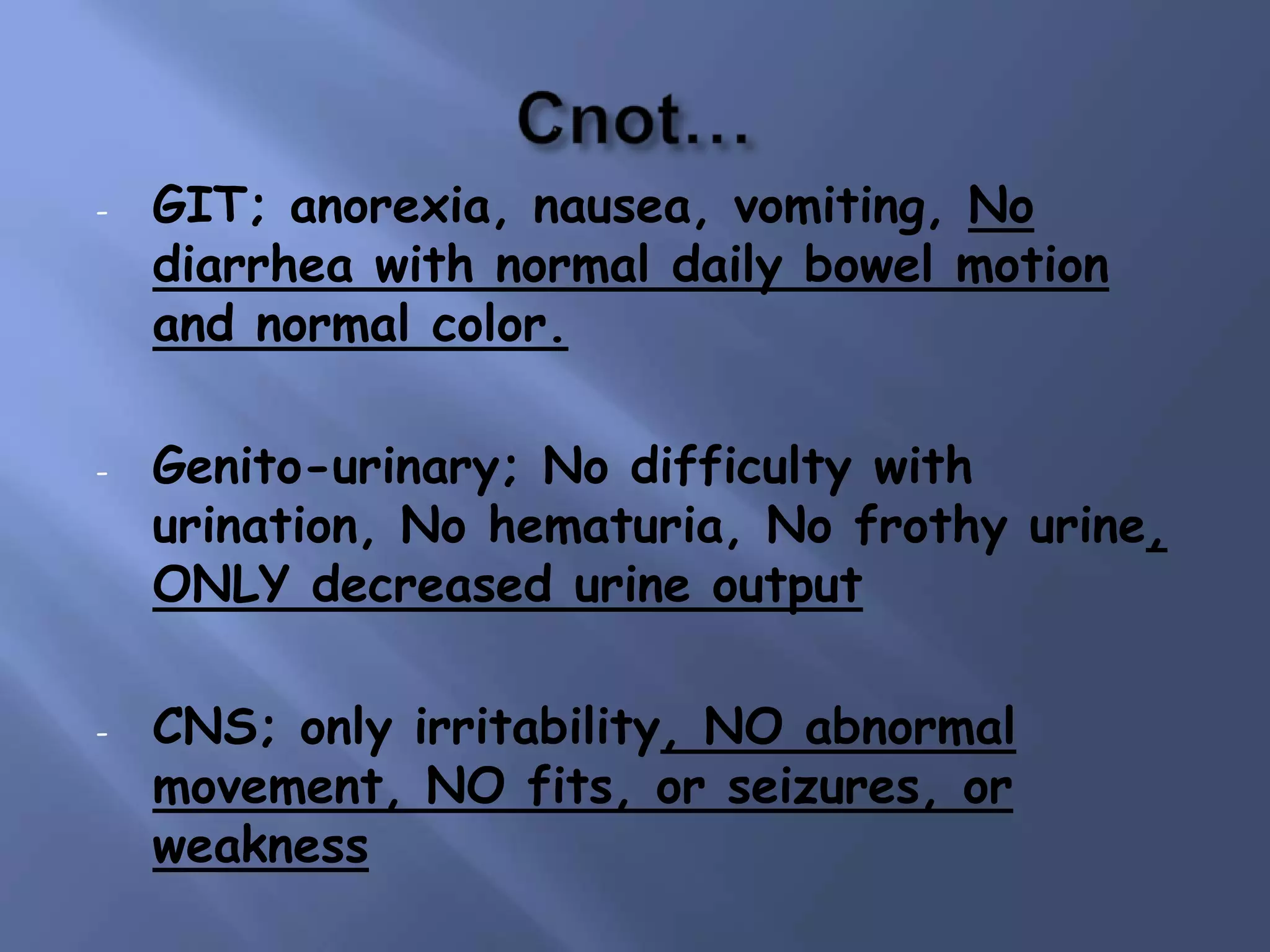
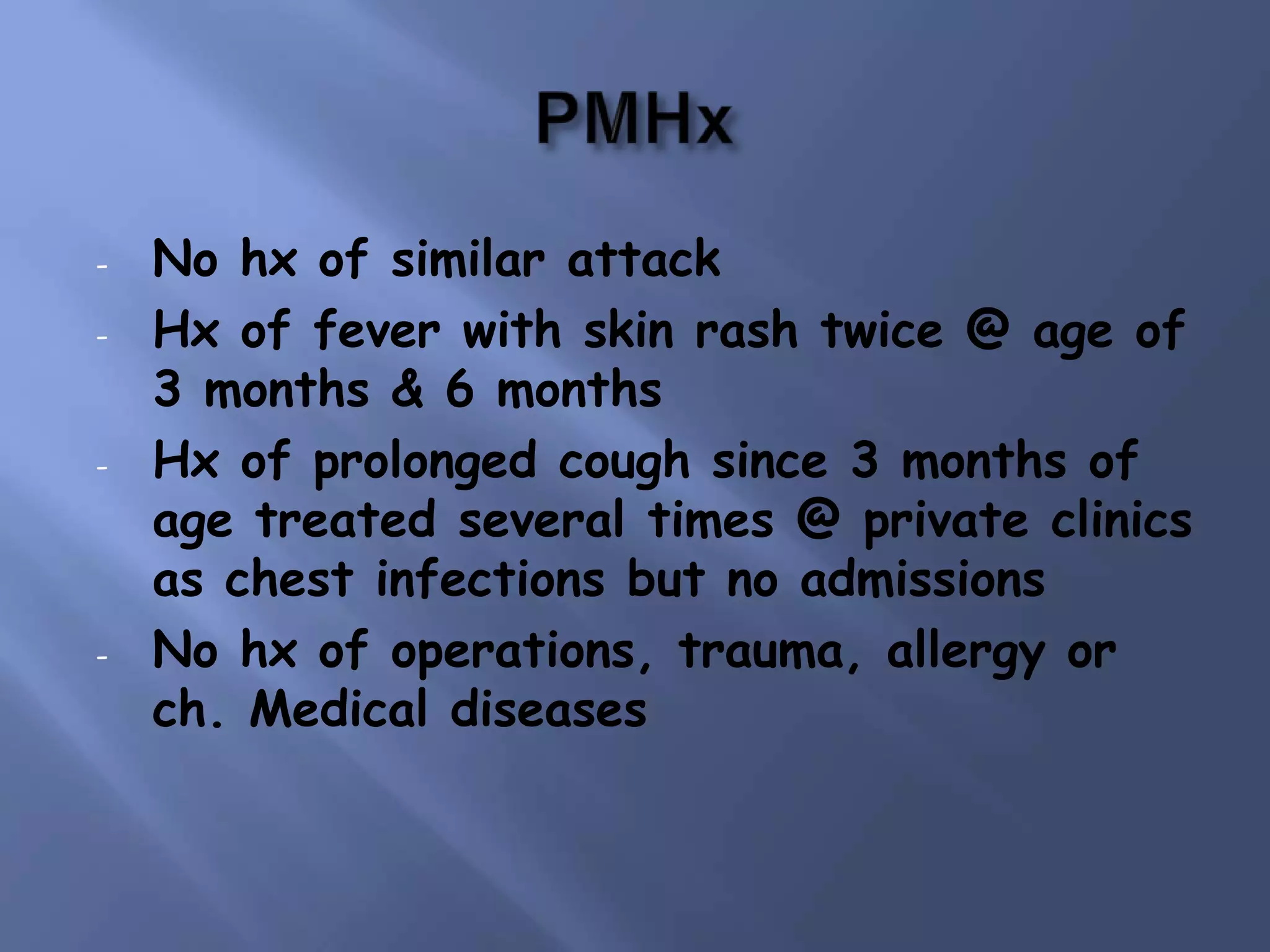
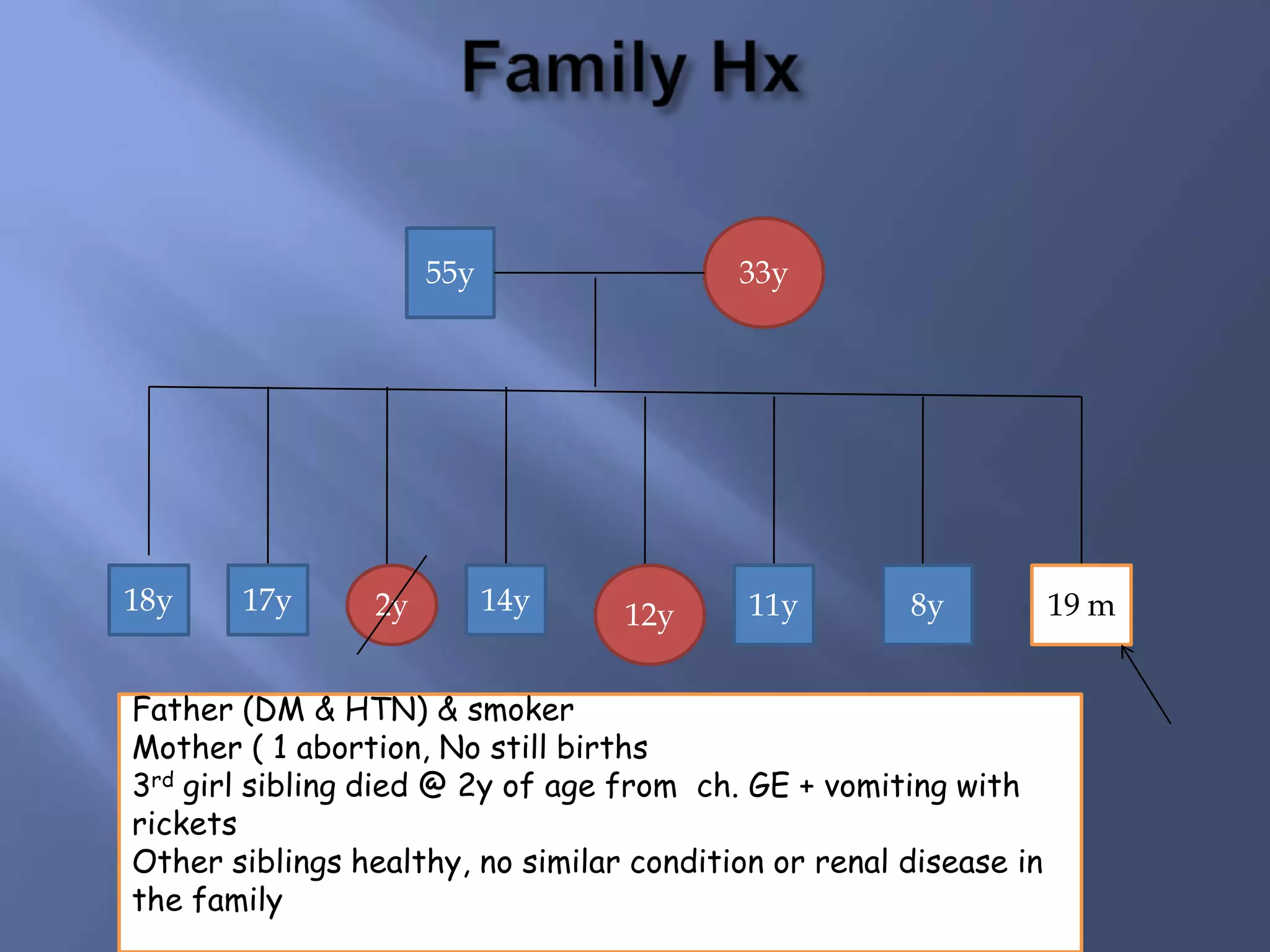
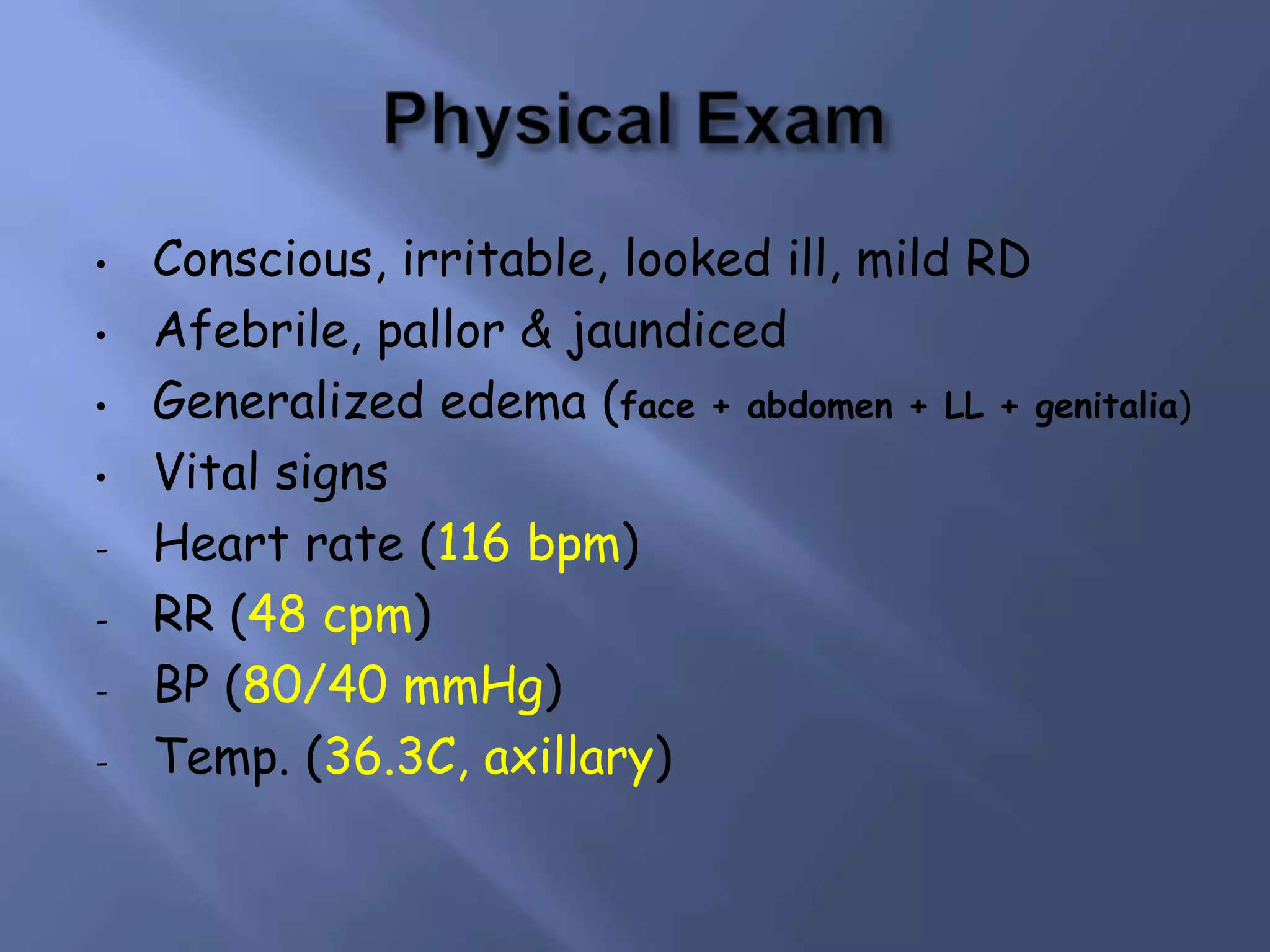
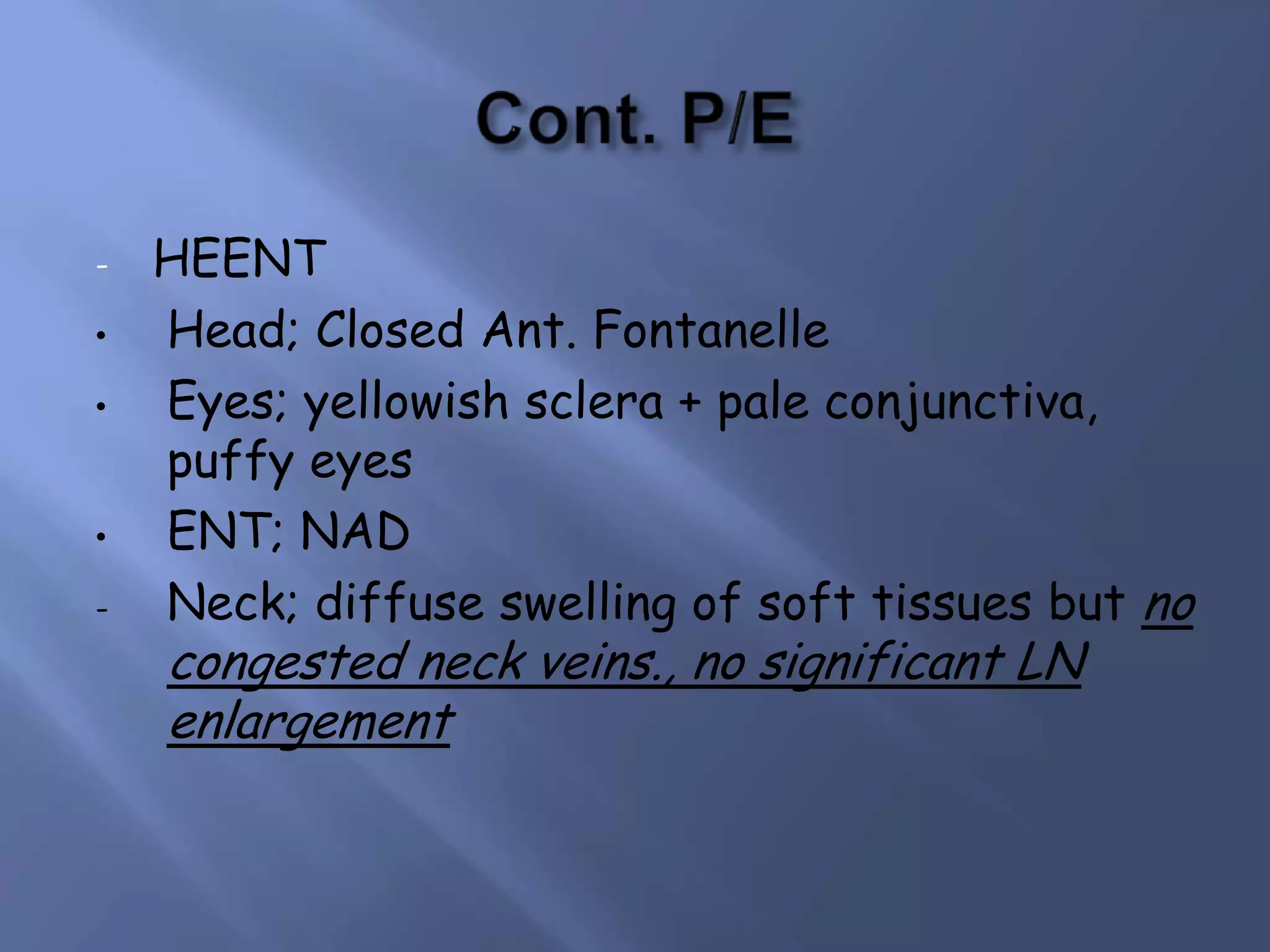
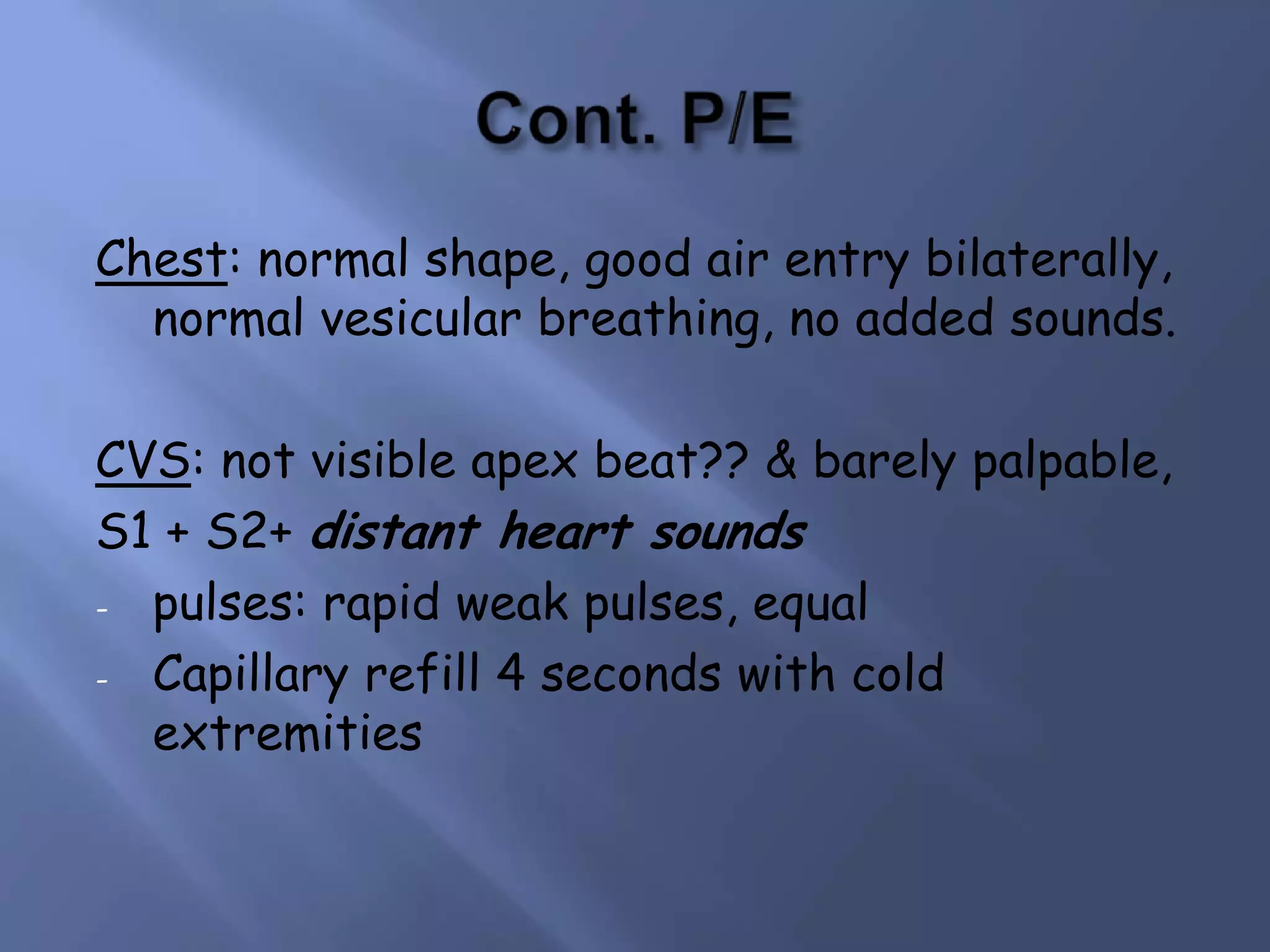
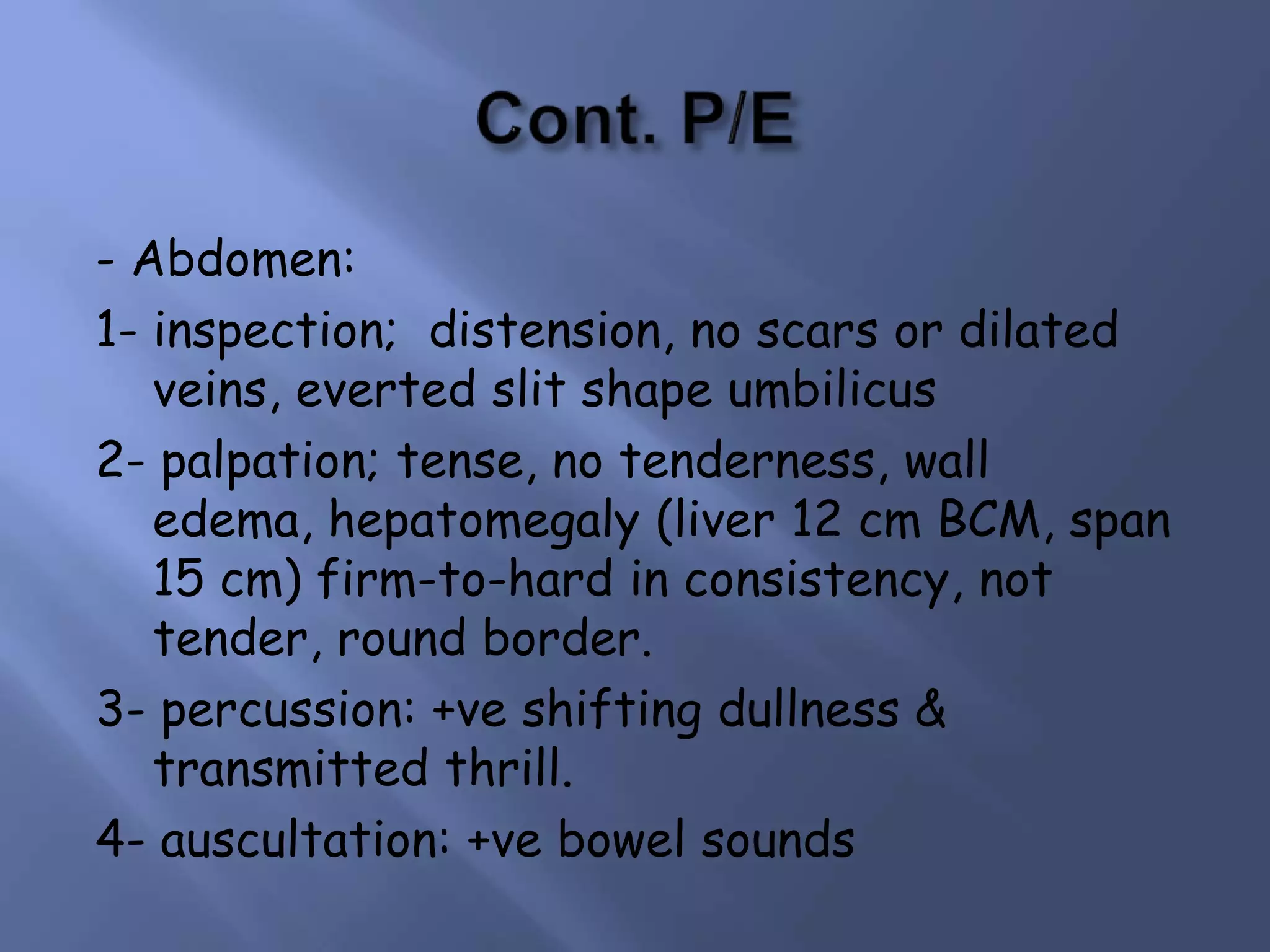
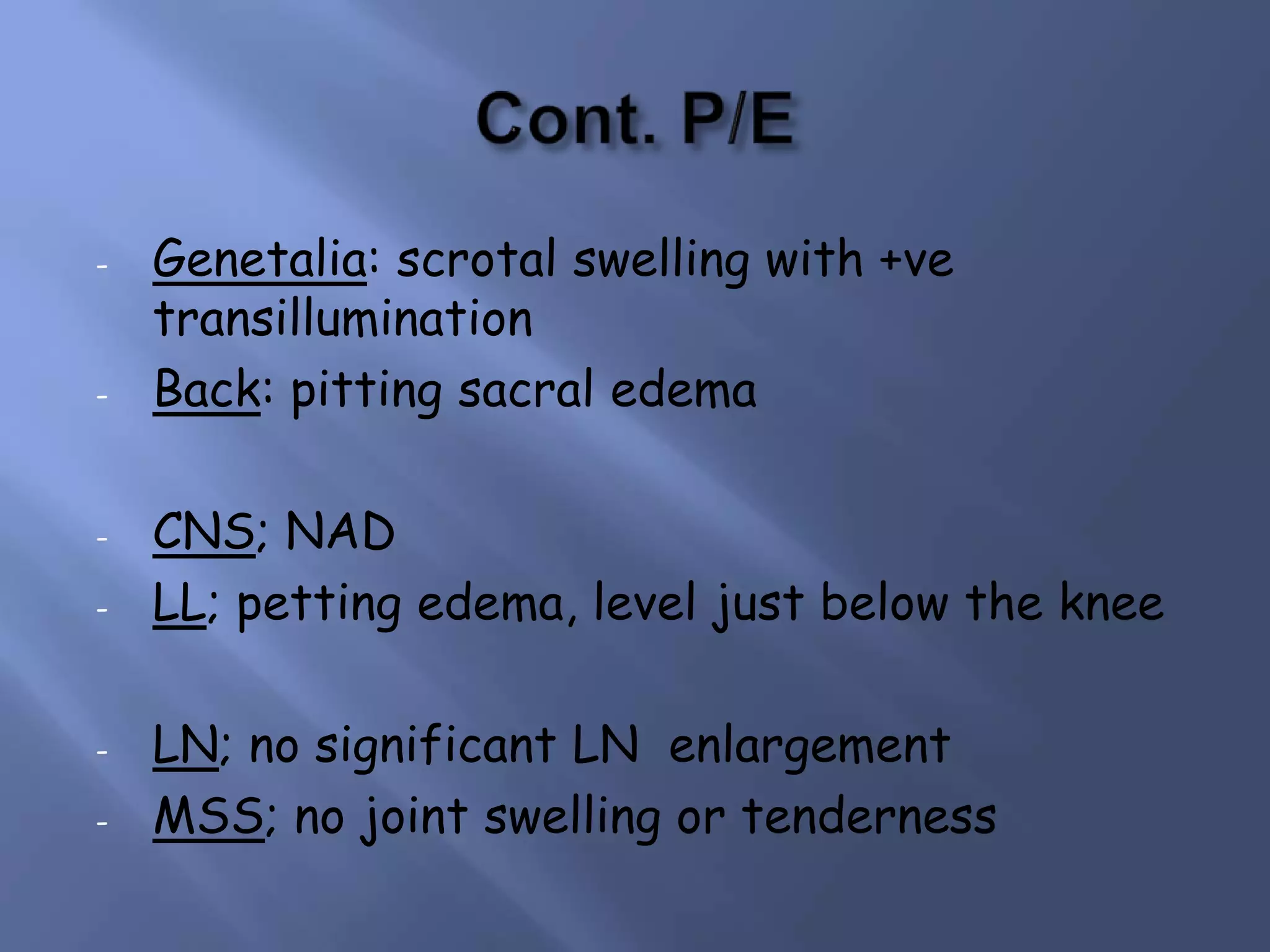
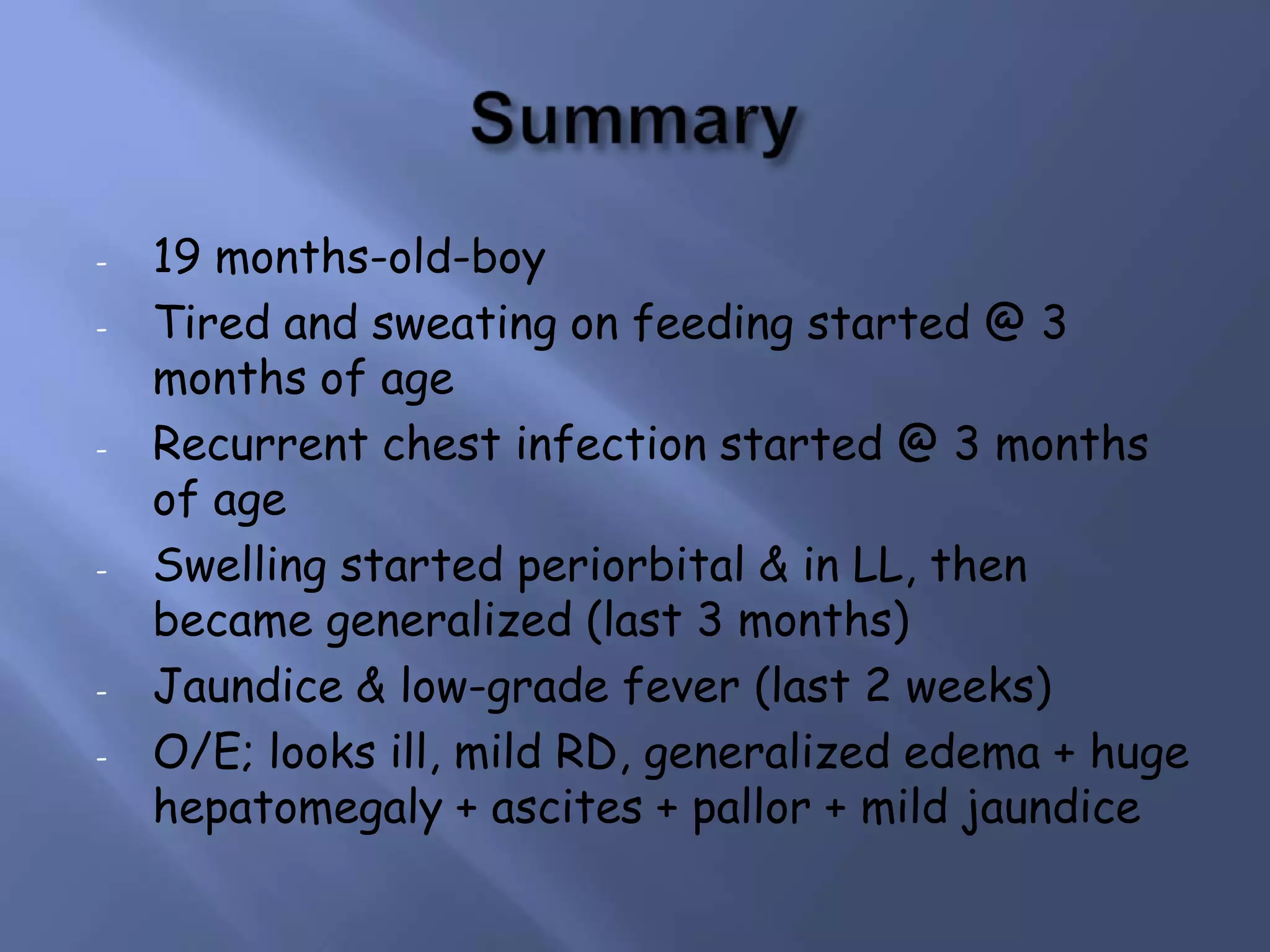
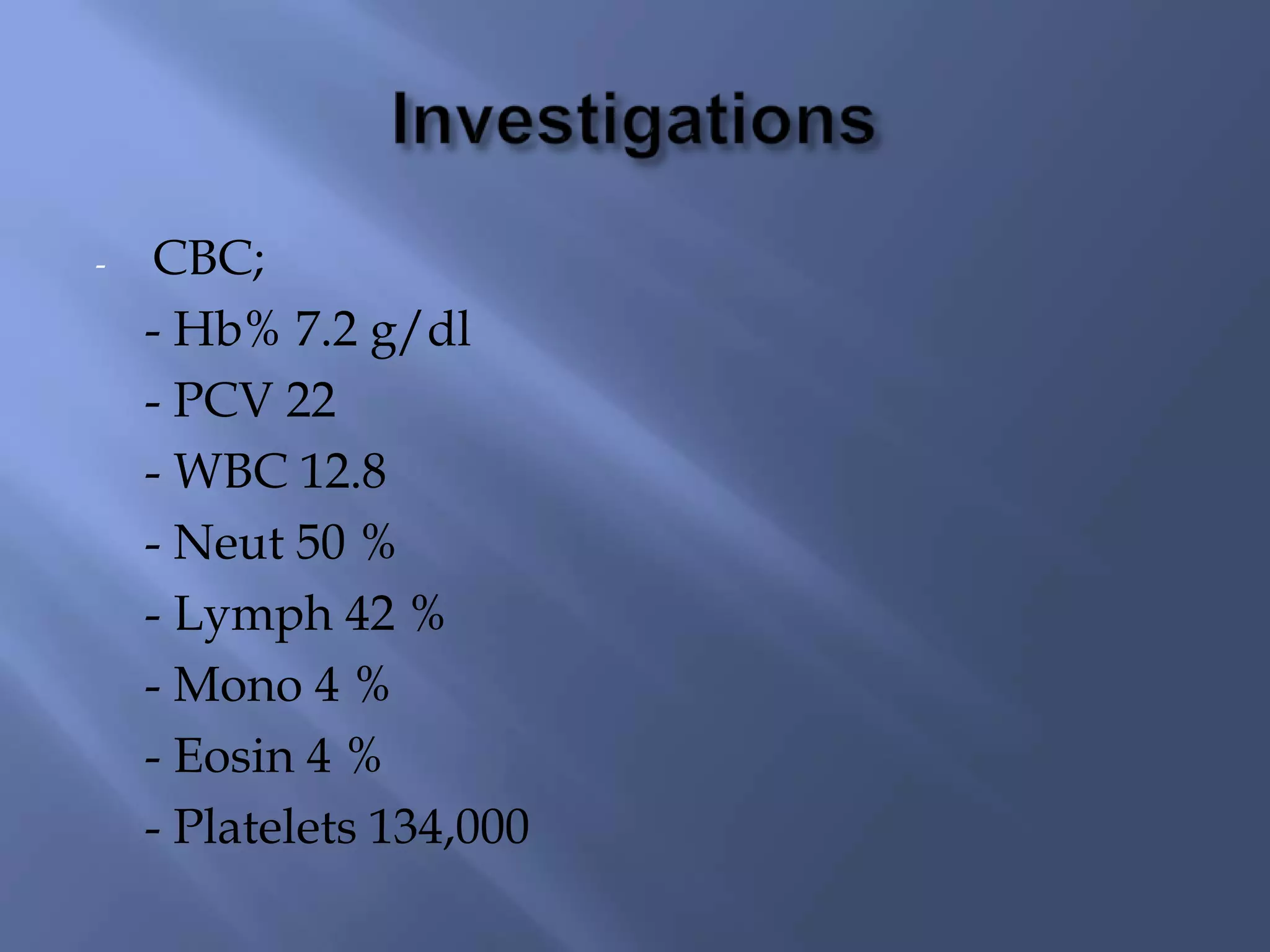
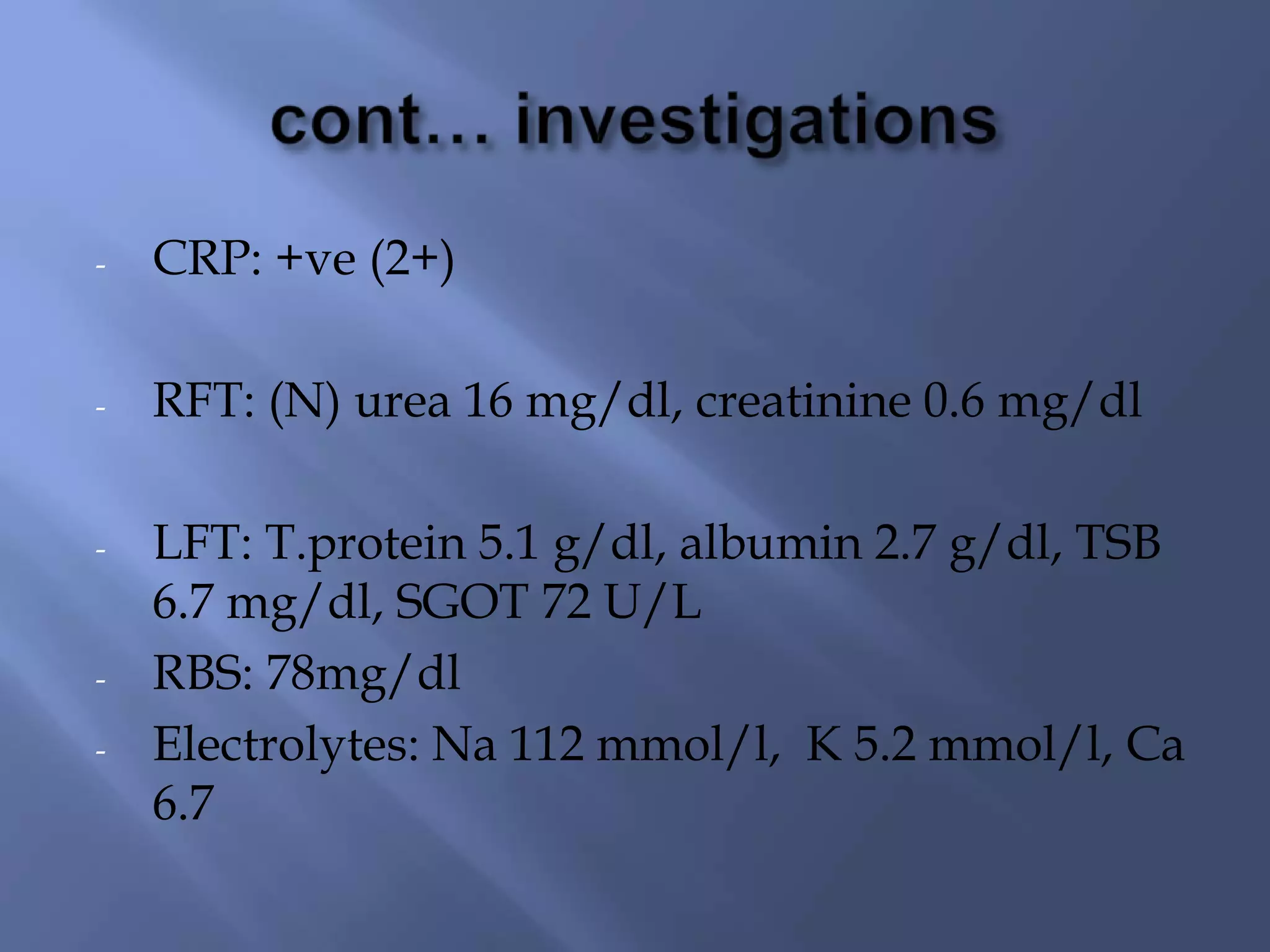
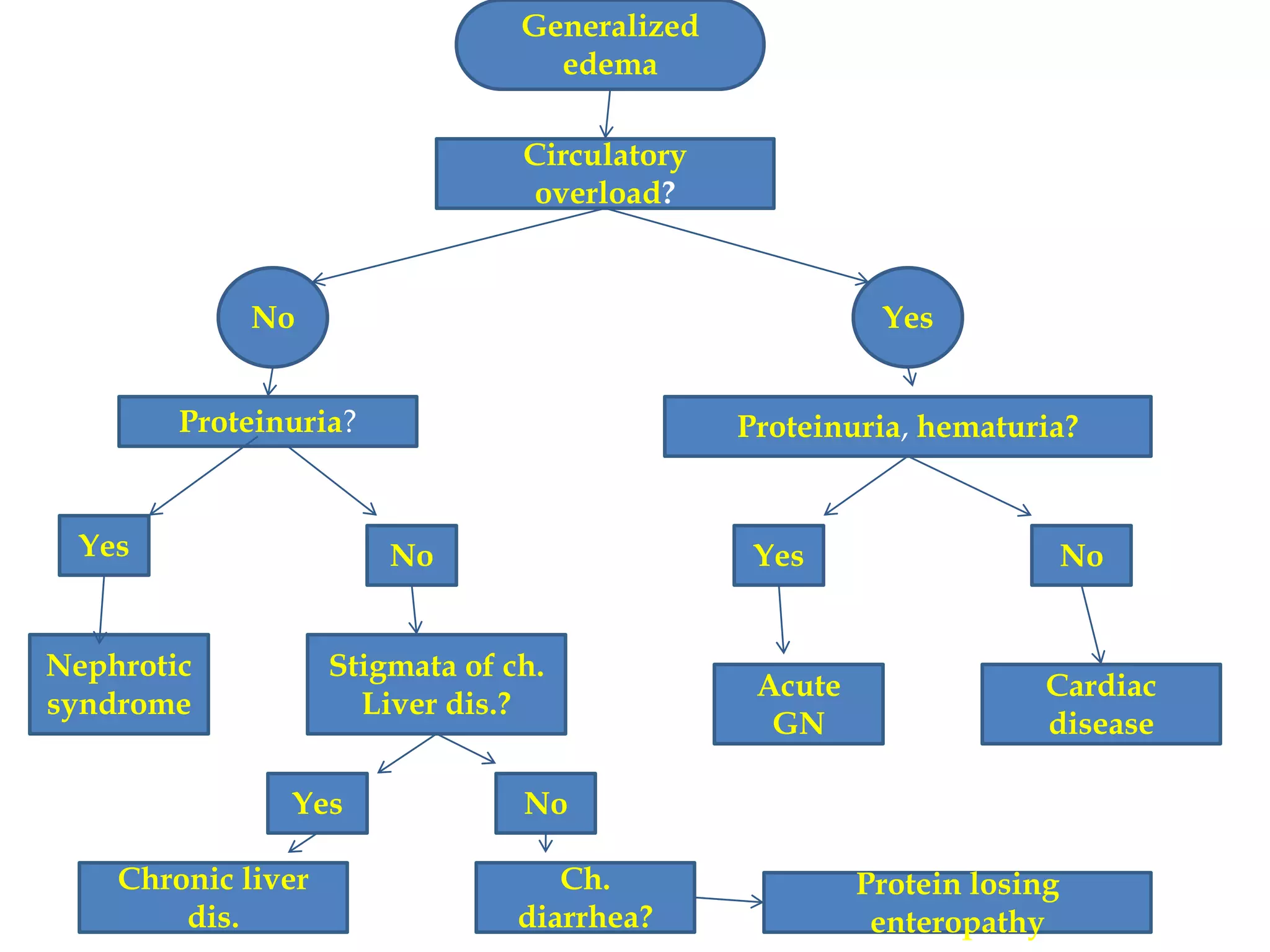
- A 19-month-old boy presented with generalized body swelling that began 3 months prior and gradually progressed. On examination, he had generalized edema, hepatomegaly, ascites, pallor, and mild jaundice.
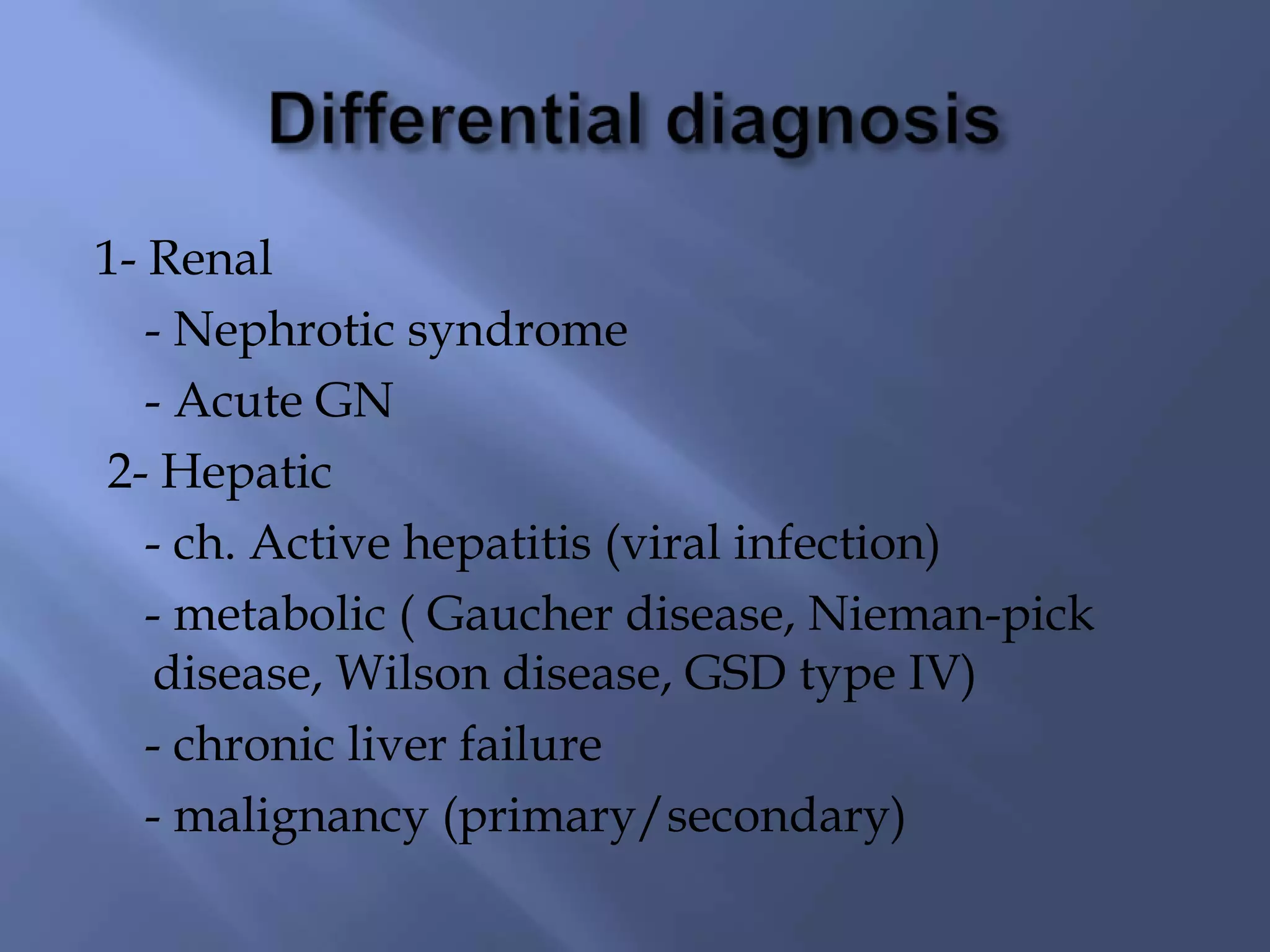
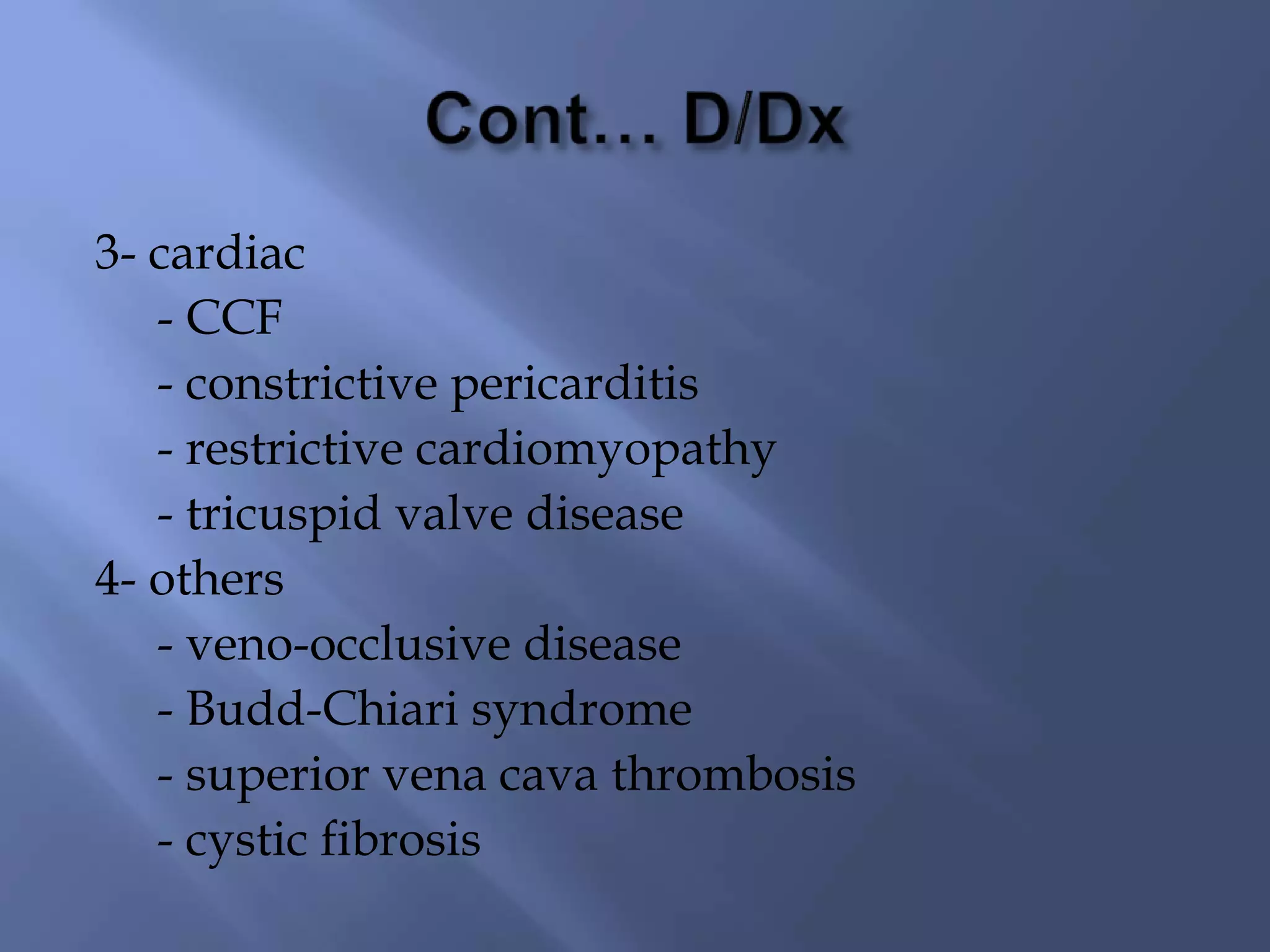
- Differential diagnoses included cardiac causes like congestive heart failure, restrictive cardiomyopathy, and constrictive pericarditis as well as hepatic causes such as viral hepatitis, metabolic diseases, or malignancy.
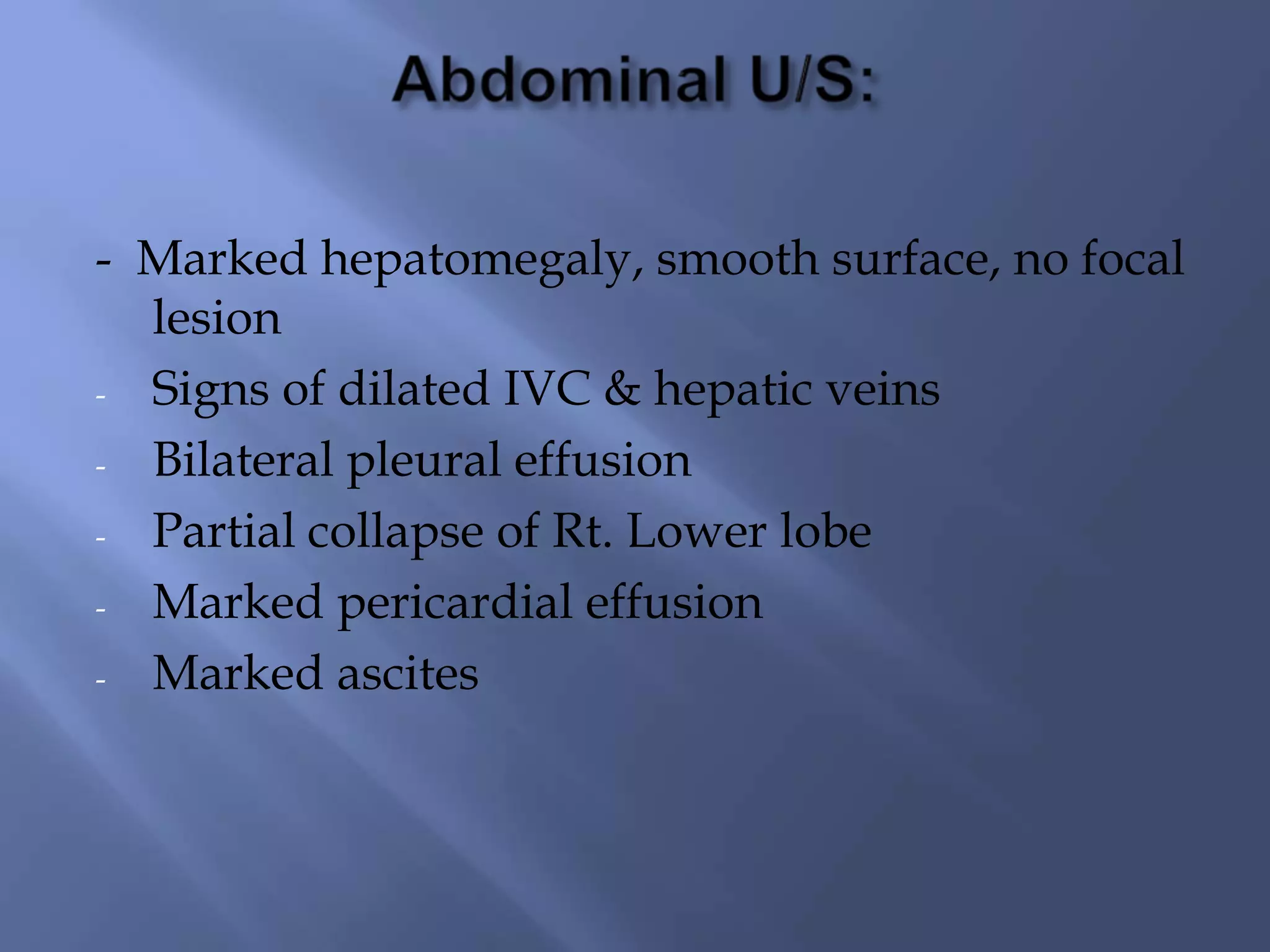
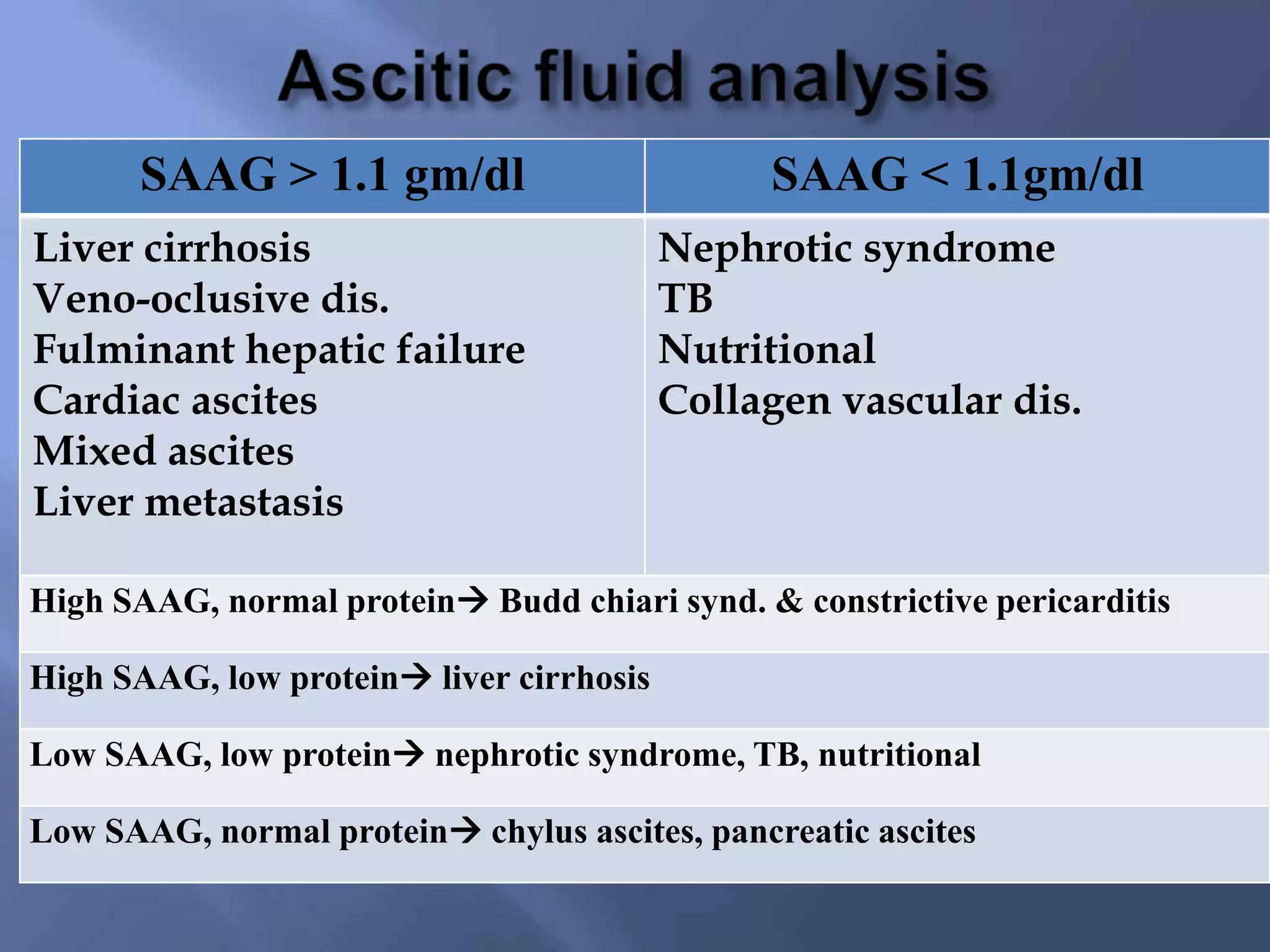
- Imaging showed markedly enlarged liver with dilated hepatic veins and IVC, ascites, pleural effusion, and pericardial effusion. This was consistent with restrictive cardiomyopathy and congestive heart failure.